- Search
| Ann Rehabil Med > Volume 40(4); 2016 > Article |
Abstract
Objective
Methods
Results
CONFLICT OF INTEREST:
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
Fig. 1
Positioning of the air-filled lingual pressure sensor of the Iowa Oral Performance Instrument between the tongue and an oral structure.
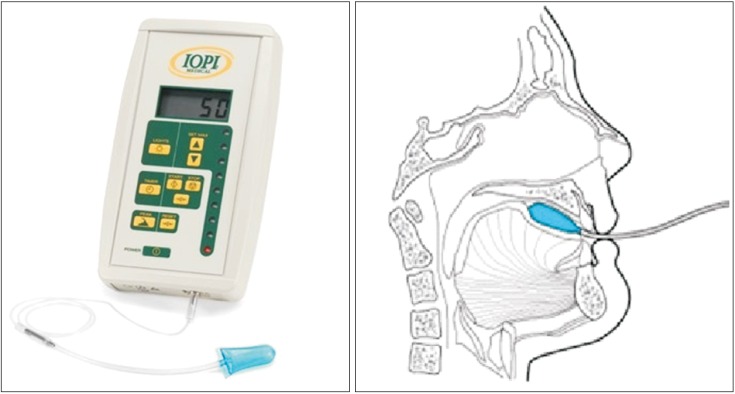
Fig. 2
Correlation between premature bolus loss (PBL) and mean tongue pressure. A larger amount of PBL was associated with a lower maximal tongue pressure (Jonckheere– Terpstra rank correlation test, p<0.05). AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; LP, lip closure pressure.
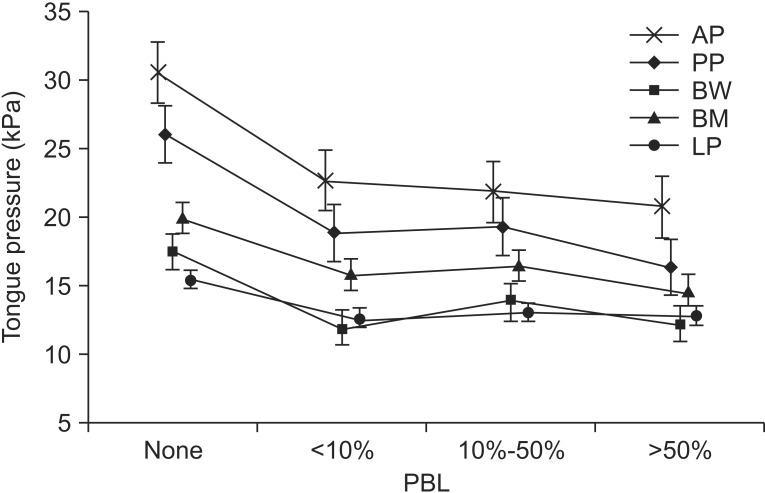
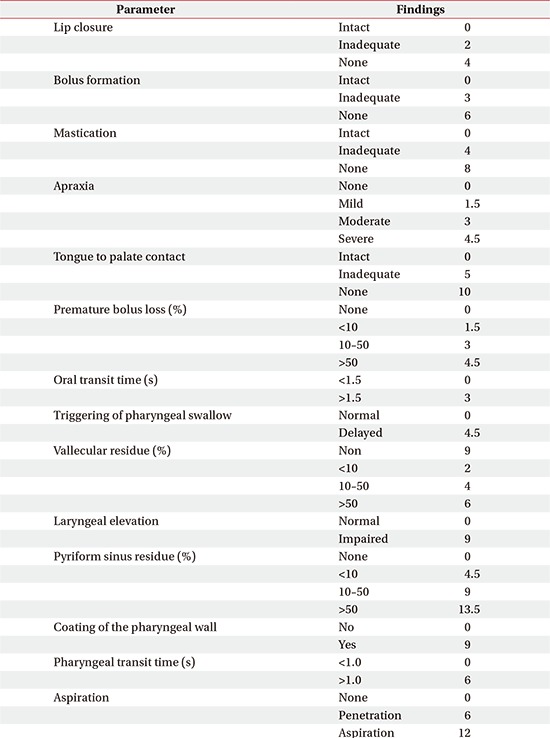
Table 2
The relationships of LP, tongue pressure, and functional outcome with lip closure and bolus formation (unit, kPa)

Values are presented as mean±standard deviation.
LP, lip pressure; AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; K-MMSE, the Korean version of Mini-Mental State Examination; K-MBI, the Korean version of Modified Barthel Index.
*p<0.05, Mann–Whitney U test.
Table 3
The relationships of LP, tongue pressure, and functional outcome with mastication and oral transit time (unit, kPa)
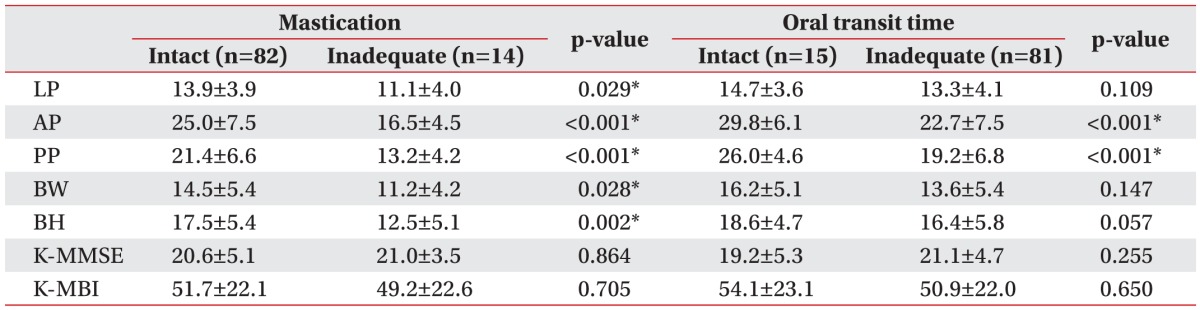
Values are presented as mean±standard deviation.
LP, lip pressure; AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; K-MMSE, the Korean version of Mini-Mental State Examination; K-MBI, the Korean version of Modified Barthel Index.
*p<0.05, Mann–Whitney U test.
Table 4
The relationships of LP, tongue pressure, and functional outcome with premature bolus loss and tongue-topalate contact (unit, kPa)
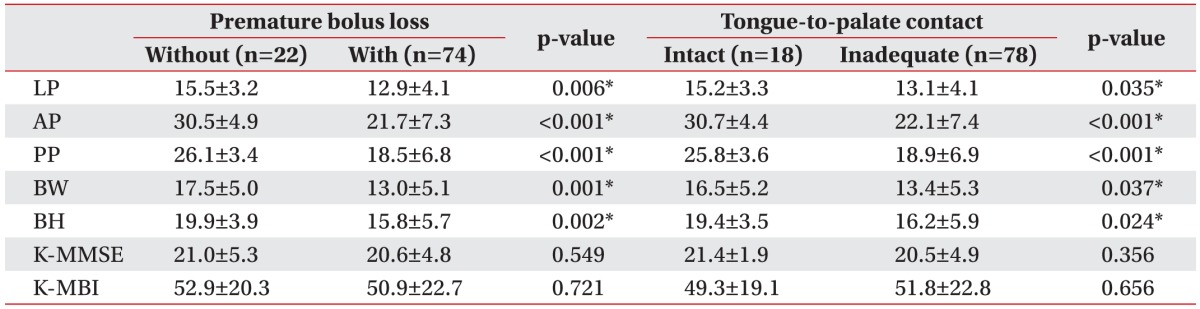
Values are presented as mean±standard deviation.
LP, lip pressure; AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; K-MMSE, the Korean version of Mini-Mental State Examination; K-MBI, the Korean version of Modified Barthel Index.
*p<0.05, Mann–Whitney U test.
- TOOLS
-
METRICS

- Related articles in ARM
-
Changes in Pharyngeal Width Over Time as an Indicator of Dysphagia in Stroke Patients2020 June;44(3)