- Search
| Ann Rehabil Med > Volume 48(3); 2024 > Article |
|
Abstract
FUNDING INFORMATION
This study was supported by the Special Research Fund for ARM Development of the Korean Academy of Rehabilitation Medicine in 2023.
AUTHOR CONTRIBUTION
Conceptualization: Park JM, Shin JC. Methodology: Park JM. Formal analysis: Park JM. Funding acquisition: Shin JC. Project administration: Park JM. Visualization: Park JM. Writing – original draft: Park JM. Writing – review and editing: Park JM, Kim YW, Lee SJ, Shin JC. Approval of final manuscript: all authors.
SUPPLEMENTARY MATERIALS
Supplementary Fig. S1.
Supplementary Fig. S2.
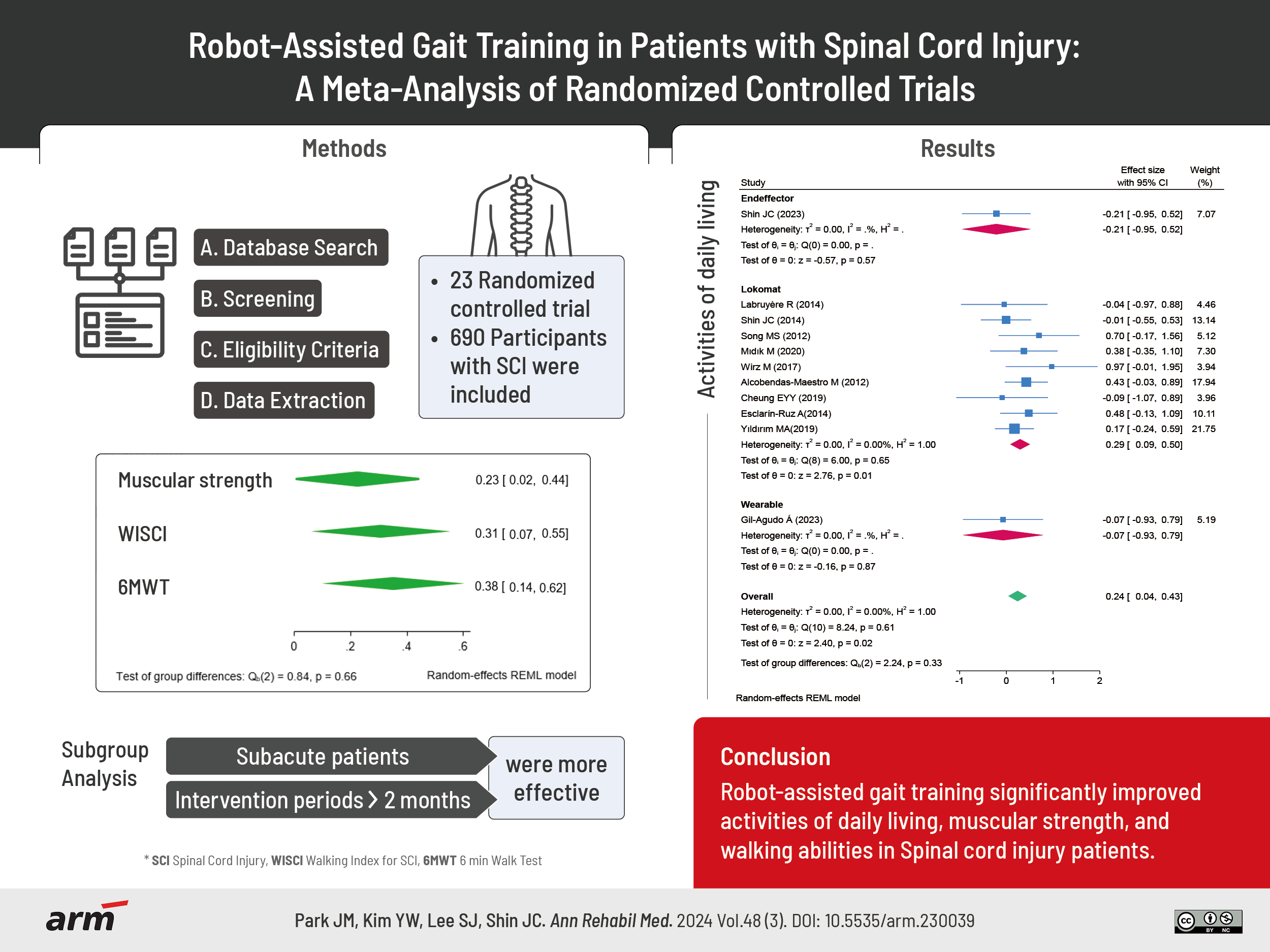
Fig. 1.

Fig. 2.

Fig. 3.
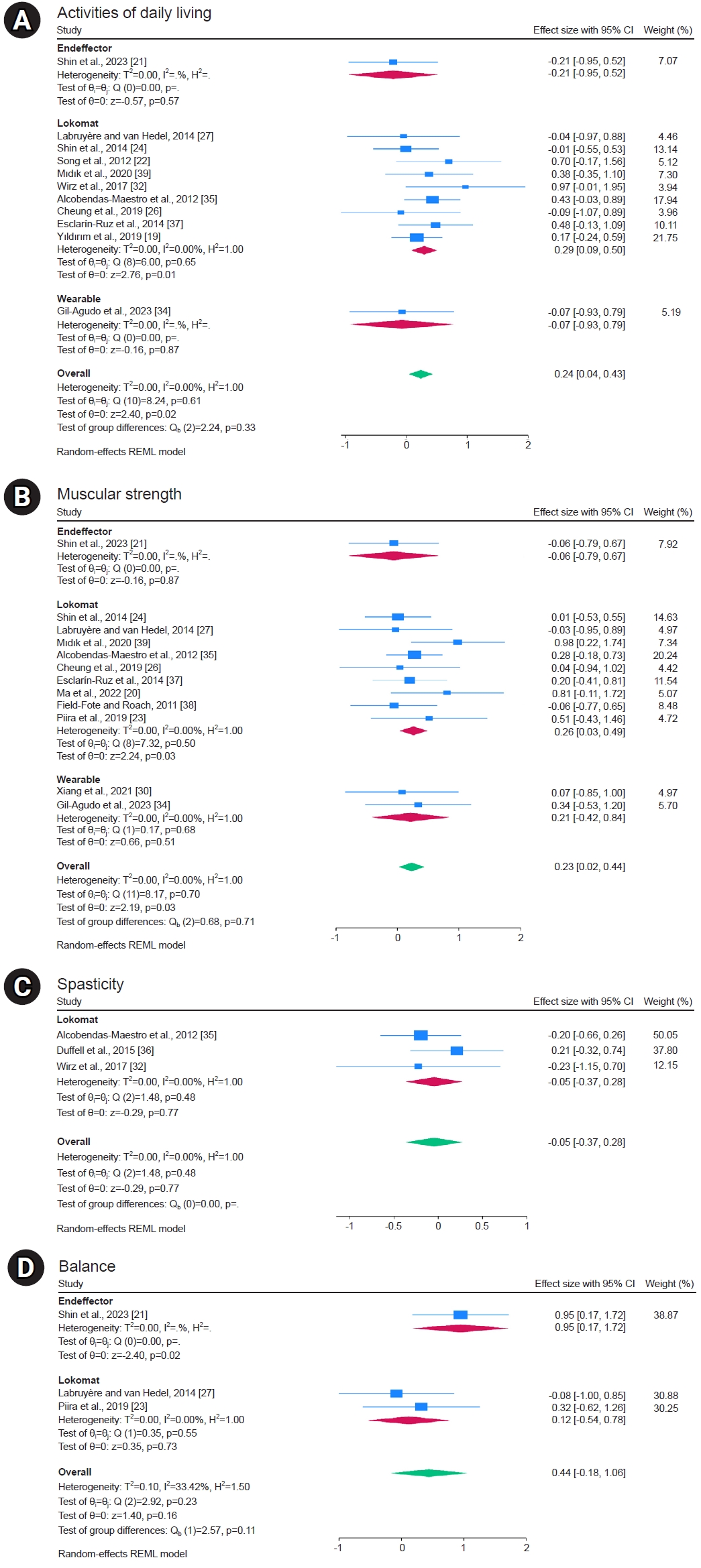
Fig. 4.
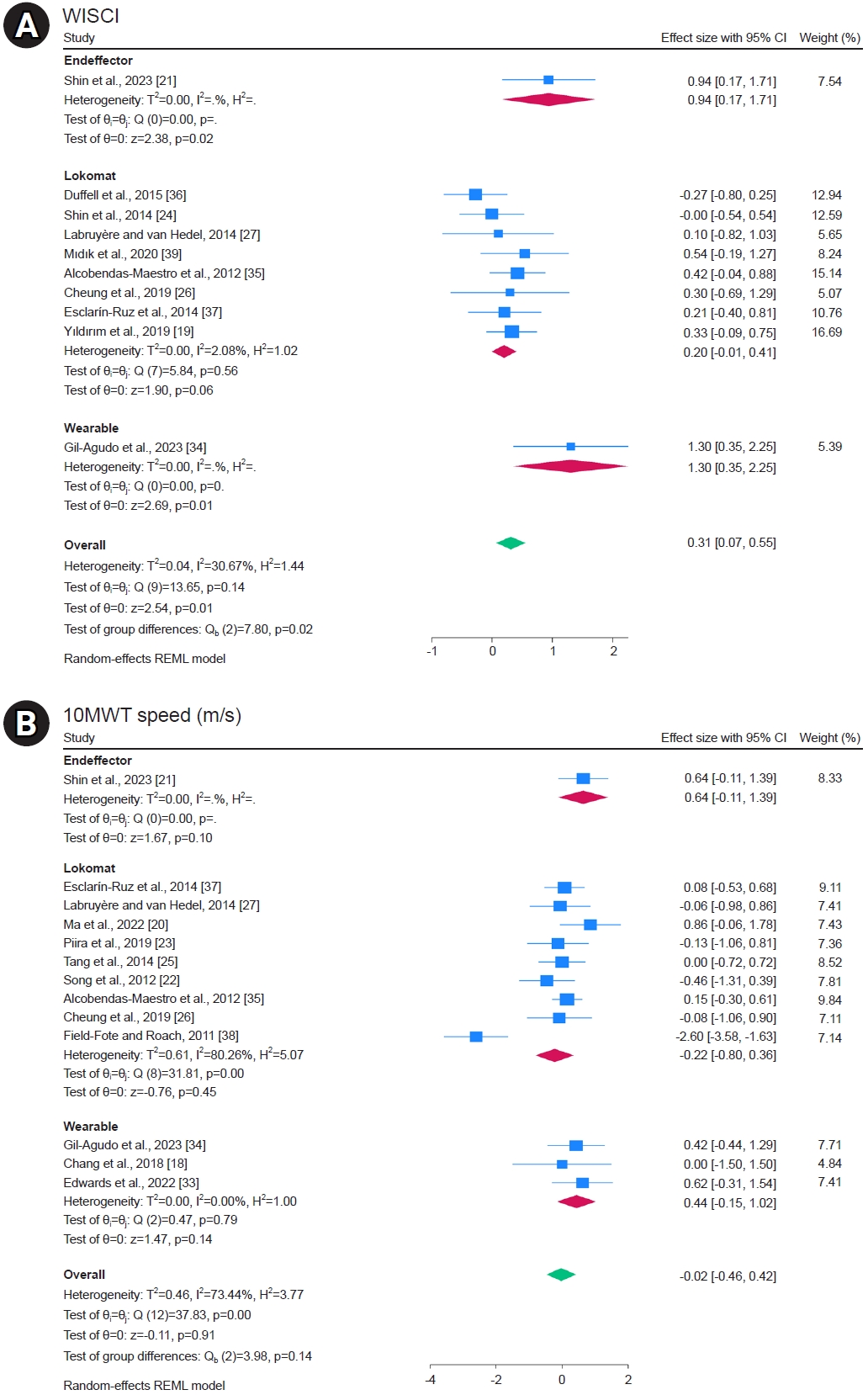
Fig. 5.

Fig. 6.

Table 1.
| Study | No. of participants (experimental/control) | Age, years2 (experimental/control) | ASIA grade (experimental/control) | Onset duration (experimental/control) (day) | Tetraplegia/paraplegia (experimental/control) | Initial WISCI (experimental/control) | Intervention protocol | Control protocol | Outcome measure | Main findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Treadmill training exoskeleton robot-Lokomat | ||||||||||
| Alcobendas-Maestro et al., 2012 [35] | 37/38 | 45.2±15.5/49.5±12.8 | C 68/71 | 117.4±43.3/136.3±64.9 | Tetraplegia 59/61 | 5.1±3.8/4.1±2.8 | -Lokomat 30-min | Standard physical treatment | 1. Speed (m/s) | No significant differences were found at entry between treatment groups |
| D 32/29 | Paraplegia 41/39 | 40 sessions (8 wk) | 40 walking training | 2. WISCI II | The WISCI II for the Lokomat group (16 [8.5–19]) was better than that for overground therapy (9 [8–16]) | |||||
| -Body weight support was initially set at 60% of each individual’s weight and then decreased in accordance with load tolerance, but not <25% support | sessions of 1 h duration (8 wk) | 3. Walk distance (m) | The 6MWT and LEMS displayed significant differences in favor of Lokomat therapy, but were not corrected for multiple comparisons | |||||||
| 4. FIM-Locomotor | ||||||||||
| 5. LEMS | ||||||||||
| 6. Ashworth | ||||||||||
| 7. VAS | ||||||||||
| Cheung et al., 2019 [26] | 8/8 | 55.6±4.9/53.0±12.9 | C 7/4 | 510.0±210.3/312.0±189.3 | Tetraplegia 8/8 | 14.6±4.3/17.0±2.8 | -Lokomat 30-min | Standard physical treatment | 1. Speed (cm/s) | The Lokomat group improved walking ability and cardiopulmonary function in patients with SCI |
| D 1/4 | 24 sessions (3 times per week for 8 weeks) | 30-min | 2. WISCI II | However, there were no significant differences in the control group | ||||||
| -Body weight support was set at 40% of body weight to minimize individual difference | 24 sessions (3 times per week for 8 weeks) | 3. SCIM III | ||||||||
| 4. LEMS | ||||||||||
| 5. Maximal oxygen consumption (L/kg/min) | ||||||||||
| 6. PEF (L/s) | ||||||||||
| 7. FEV1 (L) | ||||||||||
| 8. FVC (L) | ||||||||||
| Duffell et al., 2015 [36] | 27/29 | 46.6±12.6/47.8±13.1 | C N/R | 3394.5±3942.0/2956.5±2956.5 | N/R | 14.7±5.2/13.8±5.8 | -Lokomat 30–45 min | Standard physical treatment | 1. Speed (m/s) | Walking speed and endurance improved, with no difference between interventions |
| D N/R | 12 sessions (3 times per week for 4 weeks) | 2. Distance (m) | ||||||||
| 3. Time (s) | ||||||||||
| 4. WISCI II | ||||||||||
| 5. MAS | ||||||||||
| Esclarín-Ruz et al., 2014 [37] | 21/21 | 43.6±12.0/44.9±7.0 | C 14/16 | 125.6±65.2/140.3±45.5 | Tetraplegia 16/16 | 5.9±4.5/4.9±4.1 | -Lokomat 30-min | Standard physical treatment | 1. 10MWT (m/s) | RAGT yielded better results in the 6MWT and LEMS in patients |
| D 7/5 | Paraplegia 5/5 | 40 sessions (8 wk) | 30-min | 2. 6MWT (m) | ||||||
| -Body weight support was initially set at 60% of each individual’s weight and then decreased in accordance with load tolerance, but not <25% support | 40 sessions (8 wk) | 3. FIM-Locomotor | ||||||||
| 4. LEMS | ||||||||||
| Field-Fote and Roach, 2011 [38] | 14/17 | 45.0±8.0/42.2±15.7 | N/R | >365 | N/R | LEMS | - Lokomat | Standard physical treatment | 1. Speed (m/s) | In chronic motor incomplete SCI, there were no significant between-group differences |
| 12.7±6.9/12.9±5.3 | 60 sessions (12 wk) | Manual assistance for stepping | 2. Distance walked (m) | |||||||
| -Guidance forces were set at | 3. LEMS | |||||||||
| 100% to provide maximal assistance throughout the step cycle | ||||||||||
| Gorman et al., 2016 [31] | 12/6 | 51.5±12.7/52.0±15.4 | C 2/0 | >365 | Tetraplegia 8/6 | LEMS | -Lokomat 25–45-min | Standard physical treatment | 1. Body mass (kg) | Robot group improved peak VO2 than control group |
| D 10/6 | Paraplegia 4/0 | 34.2±11.5/36.2±8.4 | 36 sessions (12 wk) | 2. Tissue fat (%) | ||||||
| -Ultimately, partial | 3. Lean tissue (kg) | |||||||||
| body weight support was set between 70%–80% if the participant was able to support his or her weight | 4. Bone mineral content (kg) | |||||||||
| 5. VO2 peak (ml/kg/min) | ||||||||||
| Labruyère and van Hedel, 2014 [27] | 9/9 | 59±11 | N/R | 1500.0±1680.0 | Tetraplegia 6 | 14.0±3.0 | -Lokomat 45 min | Strength training | 1. 10MWT (m/s) | Chronic incomplete SCI dependent on walking assistance, robot group was not more effective in improving walking-related outcome compared to lower extremity strength training |
| Paraplegia 3 | 16 sessions (4wk) | 45-min | 2. WISCI | |||||||
| -30% bodyweight support and a speed of 1–2 km/h | 16 sessions (4 wk) | 3. SCIM | ||||||||
| 4. BBS | ||||||||||
| 5. LEMS | ||||||||||
| 6. Figure eight test | ||||||||||
| 7. Gait symmetry | ||||||||||
| 8. PCI | ||||||||||
| 9. BBS | ||||||||||
| Ma et al., 2022 [20] | 10/10 | 8.4±1.1/8.6±1.2 | N/R | 400.8±147.0/468.0±158.1 | N/R | 16.2±1.3/15.9±2.2 | -Lokomat 30-min | Standard physical treatment | 1. 10MWT (m/s) | RAGT may significantly improve the immediate motor function and walking ability of children with thoracolumbar incomplete SCI |
| 40 sessions (8 wk) | 60-min | 2. 6MWT (m) | ||||||||
| -70%–40% bodyweight support | 40 sessions (8 wk) | 3. LEMS | ||||||||
| 4. PCI | ||||||||||
| 5. WISCI | ||||||||||
| 6. Centre of pressure (cm2) | ||||||||||
| Mıdık et al., 2020 [39] | 15/15 | 35.4±12.1/37.9±10.0 | C 6/10 | 411.4±637.9/861.6±662.5 | Tetraplegia 0/0 | 9.8±1.4/11.0±1.1 | -Lokomat 30-min | Standard physical treatment | 1. WISCI | Conventional rehabilitation is useful in terms of the improvement in the lower extremity motor function, walking, and functional status in men with incomplete SCI. Additional RAGT provides a better improvement in the lower extremity motor function and functional independence |
| D 9/5 | Paraplegia 15/15 | 15 sessions (5 wk) | 30-min | 2. SCIM | ||||||
| -In addition to standard physical treatment | 25 sessions (5 wk) | 3. LEMS | ||||||||
| -50% bodyweight support and a speed of 1.5 km/h | ||||||||||
| Nooijen et al., 2009 [40] | 12/13 | 44.3±8.9/38.2±14.6 | N/R | 3327.5±3214.8/1569.2±1545.4 | Tetraplegia 0/11 | N/R | -Lokomat 60-min | Standard physical treatment | 1. Cadence (steps/min) | No significant differences were found among training groups; however, there was an interaction effect, indicating that step and stride length improved least in the robot-assisted gait training group |
| Paraplegia 15/2 | 60 sessions (12 wk) | 60-min | 2. Symmetry index (%) | |||||||
| -30% bodyweight support | 60 sessions (12 wk) | 3. Step length (m) | ||||||||
| 4. Stride length (m) | ||||||||||
| 5. Intralimb coordination | ||||||||||
| 6. Timing of onset knee | ||||||||||
| Piira et al., 2019 [23] | 7/12 | 55.0±8.0/46.0±15.0 | C 1/5 | 7665.0±839.0/5475.0±6570.0 | Tetraplegia 4/6 | LEMS | -Lokomat 20–30 min | Standard physical treatment | 1. 10MWT (m/s) | In chronic SCI, robot-assisted gait training did not restore independent walking function |
| D 6/7 | Paraplegia 3/6 | 26.6±22.0/27.8±31.9 | 60 sessions (24 wk) | 60 sessions (24 wk) | 2. 6MWT (m) | A modest, but non-significant, effect was seen on muscle strength and balance | ||||
| -<40% bodyweight support | 3. LEMS | |||||||||
| 4. BBS | ||||||||||
| 5. Modified functional reach test | ||||||||||
| Shin et al., 2014 [24] | 27/26 | 43.2±14.4/48.2±11.5 | N/R | 99.9±90.6/81.9±59.1 | Tetraplegia 15/16 | 5.9±10.9/6.9±12.6 | -Lokomat 40-min | Standard physical treatment | 1. WISCI | RAGT combined with conventional physiotherapy could yield more improvement in ambulatory function than conventional therapy alone |
| Paraplegia 12/10 | 12 sessions (4 wk) | 30-min | 2. SCIM | |||||||
| -In addition to standard physical treatment | 40 sessions (4 wk) | 3. LEMS | ||||||||
| -50% bodyweight support and a speed of 1.5 km/h | 4. Ambulatory motor index (AMI) | |||||||||
| Tang et al., 2014 [25] | 15/15 | 38.1±7.1/39.2±8.1 | D 15/15 | Median 189 | Tetraplegia 0/0 | N/R | -Lokomat | 40 min 1 session | 1. 10MWT (m/s) | RAGT not only decreased reaction time, but also improved the walking ability |
| Paraplegia 15/15 | 40 min 1 session | Ergo_bike rate of 45 rpm with a work load of 60 W | 2. Probe reaction time | |||||||
| -35%–70% bodyweight support and a speed of 1.5–1.8 km/h | ||||||||||
| Wirz et al., 2017 [32] | 9/9 | 35.56±13.8/34.3±16.0 | B 3/6 | 35.1±18.6/43.2±25.7 | Tetraplegia 7/6 | N/R | -Lokomat 50-min | Standard physical treatment | 1. SCIM | No significant differences were found among training groups |
| C 6/3 | Paraplegia 2/3 | 34 sessions (8 wk) | 25-min | 2. Spasticity (MAS) | ||||||
| -Speed of 1.6–3.5 km/h | 34 sessions (8 wk) | |||||||||
| Yıldırım et al., 2019 [19] | 44/44 | 32±5.2/36.5±5.5 | A 21/18 | 90±13.7/90±13.7 | Tetraplegia 9/7 | 5.0±6.9/5.0±5.1 | -Lokomat 30-min | Standard physical treatment | 1. WISCI | RAGT combined with conventional therapy was found to be superior to the conventional therapy in terms of gait function and level of disability |
| BCD 23/26 | Paraplegia 35/37 | 16 sessions (8 wk) | 30-min | 2. FIM | ||||||
| -Standard physical treatment | 40 sessions (twice a day) | |||||||||
| 30-min 40 sessions (twice a day) (8 weeks) | (8 wk) | |||||||||
| Song et al., 2012 [22] | 11/11 | 53.7±8.8/53.3±6.0 | N/R | 20.2±5.0/20±4.8 | Tetraplegia 9/10 | N/R | -Lokomat 20-min | Standard physical treatment | 1. Balance (TETRAX fall risk) | RAGT significantly improved in walking ability and lower fall risk |
| Paraplegia 2/1 | 20 sessions (4 wk) | 20-min | 2. 10MWT (m/s) | |||||||
| -Standard physical treatment | 20 sessions (4 wk) | 3. 6MWT (m) | ||||||||
| 20-min | 4. MBI | |||||||||
| 20 sessions (4 wk) | ||||||||||
| Wearable gait robot-Ekso, HANK, AIDER | ||||||||||
| Chang et al., 2018 [18] | 4/3 | 56.0±17.0/60.0±2.0 | C 1/1 | 5475.0±5110.0/2555.0±1095.0 | Tetraplegia 2/1 | N/R | -Ekso 60-min | Standard physical treatment | 1. 10MWT (m/s) | RAGT could be applied to individuals with incomplete SCI to facilitate gait recovery |
| D 3/2 | Paraplegia 2/2 | 15 sessions (3 wk) | 60-min | 2. 6MWT (m) | ||||||
| 15 sessions (3 wk) | 3. TUG (s) | |||||||||
| 4. Step length (m) | ||||||||||
| Edwards et al., 2022 [33] | 9/10 | 41.7±8.5/51.9±14.5 | C 6/3 | 3066.0±3134.2/2568.3±1594.1 | Tetraplegia 7/8 | 12.1±4.4/13.8±4.5 | -Ekso GT 45-min | Body weight support | 1. Gait speed (m/s) | RAGT not statistically significant in gait speed |
| D 3/7 | Paraplegia 2/2 | 36 sessions (12 wk) | treadmill training | |||||||
| 45-min | ||||||||||
| 36 sessions (12 wk) | ||||||||||
| Evans et al., 2021 [28] | 8/8 | 41.0±11.0/38.0±14.0 | C 4/5 | 4745.0±2920.0/2555.0±2190.0 | Tetraplegia 8/8 | N/R | -Ekso GT 60-min | 60-min 72 sessions (24 wk) | 1. Heart rate | Cardiovascular efficiency of exoskeleton walking improved, particularly over the first 6 weeks |
| D 4/3 | Paraplegia 0/0 | 72 sessions (24 wk) | Warm-up and mobility (5 min) | 2. Heart rate variability | ||||||
| Resistance training (20–30 min) | 3. Systolic blood pressure (mmHg) | |||||||||
| Cardiovascular training (20–30 min) | 4. Diastolic blood pressure (mmHg) | |||||||||
| 5. Ankle brachial pressure index (ABPI) | ||||||||||
| 6. Distance (m) | ||||||||||
| 7. Rating of perceived exertion (Borg) | ||||||||||
| Gil-Agudo et al., 2023 [34] | 11/10 | 41.0±12.4/51.8±11.9 | C 8/4 | 144.6±39/166.5±69 | Tetraplegia 4/2 | 11.9±4.3/11.7±3.8 | -HANK 30-min | Standard physical treatment | 1. LEMS | Exoskeleton improved their walking independence as measured by the WISCI-II after the treatment |
| D 3/6 | Paraplegia 7/8 | 15 sessions (5 wk) | 30-min | 2. 10MWT (m/s) | ||||||
| 15 sessions (5 wk) | 3. TUG (s) | |||||||||
| 4. 6MWT (m) | ||||||||||
| 5. WISCI | ||||||||||
| 6. SCIM | ||||||||||
| Shackleton et al., 2022 [29] | 8/8 | 40.5±11.2/38.4±14.3 | C 4/5 | 5037.0±3029.5/2664.5±2336.0 | Tetraplegia 8/8 | N/R | -Ekso Bionics 60-min | Standard physical treatment | 1.Bone mineral density (g/cm2) | Twenty-four weeks of robot locomotor training is possibly a sufficient duration to prevent the progressive decline of bone mineral density |
| D 4/3 | Paraplegia 0/0 | 72 sessions (24 wk) | 60-min | 2. Fat mass (kg, %) | ||||||
| 72 sessions (24 wk) | 3. Fat-free soft tissue mass (kg) | |||||||||
| Xiang et al., 2021 [30] | 9/9 | 39.8±12.2/36.6±11.8 | A 8/4 | 60.0±118.5/60.0±13.1 | Tetraplegia 5/4 | N/R | -AIDER 60-min | Standard physical treatment | 1. FVC (L) | Exoskeleton-assisted walking has potential benefits to facilitate pulmonary function parameters among individuals with lower thoracic neurological level of SCI compared with conventional therapy |
| B 0/3 | Paraplegia 4/5 | 16 sessions (4 wk) | 60-min | 2. FEV1 (L) | ||||||
| C 1/3 | -40%–60% maximal heart rate | 16 sessions (4 wk) | 3. PEF (L/s) | |||||||
| 4. Maximal voluntary ventilation (MVV) (L) | ||||||||||
| 5. Distance (m) | ||||||||||
| 6. Heart rate | ||||||||||
| 7. Rating of Perceived Exertion | ||||||||||
| 8. SpO2 | ||||||||||
| 9. LEMS | ||||||||||
| End effector gait robot-Morning walk | ||||||||||
| Shin et al., 2023 [21] | 16/13 | 49.5±27.0/59.6±7.5 | C 2/4 | 61.7±44.9/58.2±50.7 | Tetraplegia 14/10 | WISCI II | -Morning walk 30-min | Standard physical treatment | 1. WISCI | End-effector robot gait training could improve balance and gait abilities substantially better than conventional therapy |
| D 14/9 | Paraplegia 2/2 | 3.6±4.6/3.7±6.6 | 20 sessions (4 wk) | 90-min | 2. SCIM | |||||
| -20% body weight support | 20 sessions (4 wk) | 3. LEMS | ||||||||
| -Standard physical treatment 60-min | 4. Proprioception | |||||||||
| 20 sessions (4 wk) | 5. BBS | |||||||||
| 6. WISCI II | ||||||||||
| 7. SCIM III | ||||||||||
ASIA, American Spinal Injury Association; WISCI, walking index for spinal cord injury; N/R, not recorded; LEMS, lower extremity motor score; FIM, functional independence measure; VAS, visual analogue scale; SCIM, spinal cord independence measurement; PEF, peak expiratory flow; FEV1, forced expiratory volume in the first second; MAS, modified Ashworth scale; 10MWT, 10 meter walk test; 6MWT, 6 min walk test; BBS, Berg balance scale; PCI, Physiological Cost Index; TETRAX, Tetrax (Sunlight Medical Ltd.); MBI, modified Barthel index; TUG, Timed Up and Go Test; FVC, forced vital capacity; RAGT, robotic-assisted gait training.
Table 2.
GRADE, Grading of Recommendations Assessment, Development and Evaluation; FIM, functional independence measure; SCIM, spinal cord independence measurement; MBI, modified Barthel index; LEMS, lower extremity motor score; MAS, modified Ashworth scale; BBS, Berg balance scale; WISCI, walking index for spinal cord injury; 10MWT, 10 meter walk test; 6MWT, 6 min walk test; FEV1, forced expiratory volume in first second; SMD, standardized mean difference; MD, mean difference; N/A, not applicable.
a)Risk of bias based on the Revised Cochrane Risk of Bias Tool for Randomized Trials (RoB2).
b)Downgraded if significant and unexplained heterogeneity (I2>50%, p<0.10) was not explained by the meta-regression or subgroup analysis results.
c)Downgraded if there were any factors related to the participants, interventions, or results that limited the generalizability of the results.
d)Downgraded if the 95% confidence interval crossed the benefit-or-harm boundary.
e)Downgraded if there was evidence of publication bias using Egger’s test or suspecting publication bias when visualizing with funnel plots.
f)Because all included studies were meta-analyses of randomized clinical trials, the certainty of the evidence was graded as high for all outcomes by default and then downgraded according to pre-specified criteria. The quality was graded as high, medium, low, or very low.
**p<0.05.
Table 3.
REFERENCES
- TOOLS