1. Wolfe CD. The impact of stroke. Br Med Bull 2000;56:275-286. PMID:
11092079.



2. Balami JS, Chen RL, Buchan AM. Stroke syndromes and clinical management. QJM 2013;106:607-615. PMID:
23483140.



3. Winstein CJ, Gardner ER, McNeal DR, Barto PS, Nicholson DE. Standing balance training: effect on balance and locomotion in hemiparetic adults. Arch Phys Med Rehabil 1989;70:755-762. PMID:
2802955.

4. Kelly VE, Eusterbrock AJ, Shumway-Cook A. A review of dual-task walking deficits in people with Parkinson's disease: motor and cognitive contributions, mechanisms, and clinical implications. Parkinsons Dis 2012;2012:918719PMID:
22135764.



5. de Haart M, Geurts AC, Huidekoper SC, Fasotti L, van Limbeek J. Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Arch Phys Med Rehabil 2004;85:886-895. PMID:
15179641.


6. Abernethy B. Dual-task methodology and motor skills research: some applications and methodological constraints. J Hum Mov Stud 1988;14:101-132.
7. McCulloch K. Attention and dual-task conditions: physical therapy implications for individuals with acquired brain injury. J Neurol Phys Ther 2007;31:104-118. PMID:
18025956.


8. Plummer-D'Amato P, Altmann LJ, Saracino D, Fox E, Behrman AL, Marsiske M. Interactions between cognitive tasks and gait after stroke: a dual task study. Gait Posture 2008;27:683-688. PMID:
17945497.


9. Bowen A, Wenman R, Mickelborough J, Foster J, Hill E, Tallis R. Dual-task effects of talking while walking on velocity and balance following a stroke. Age Ageing 2001;30:319-323. PMID:
11509310.



10. Hyndman D, Ashburn A, Yardley L, Stack E. Interference between balance, gait and cognitive task performance among people with stroke living in the community. Disabil Rehabil 2006;28:849-856. PMID:
16777772.


11. Hyndman D, Pickering RM, Ashburn A. Reduced sway during dual task balance performance among people with stroke at 6 and 12 months after discharge from hospital. Neurorehabil Neural Repair 2009;23:847-854. PMID:
19556368.


12. Kizony R, Levin MF, Hughey L, Perez C, Fung J. Cognitive load and dual-task performance during locomotion poststroke: a feasibility study using a functional virtual environment. Phys Ther 2010;90:252-260. PMID:
20023003.



13. McCulloch KL, Buxton E, Hackney J, Lowers S. Balance, attention, and dual-task performance during walking after brain injury: associations with falls history. J Head Trauma Rehabil 2010;25:155-163. PMID:
20473089.


14. Melzer I, Tzedek I, Or M, Shvarth G, Nizri O, Ben-Shitrit K, et al. Speed of voluntary stepping in chronic stroke survivors under single- and dual-task conditions: a case-control study. Arch Phys Med Rehabil 2009;90:927-933. PMID:
19480867.


15. Yang YR, Wang RY, Chen YC, Kao MJ. Dual-task exercise improves walking ability in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil 2007;88:1236-1240. PMID:
17908563.


16. Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther 2008;88:559-566. PMID:
18292215.



17. Jung HY, Park JH, Shim JJ, Kim MJ, Hwang MR, Kim SH. Reliability test of Korean version of Berg Balance Scale. J Korean Acad Rehabil Med 2006;30:611-618.
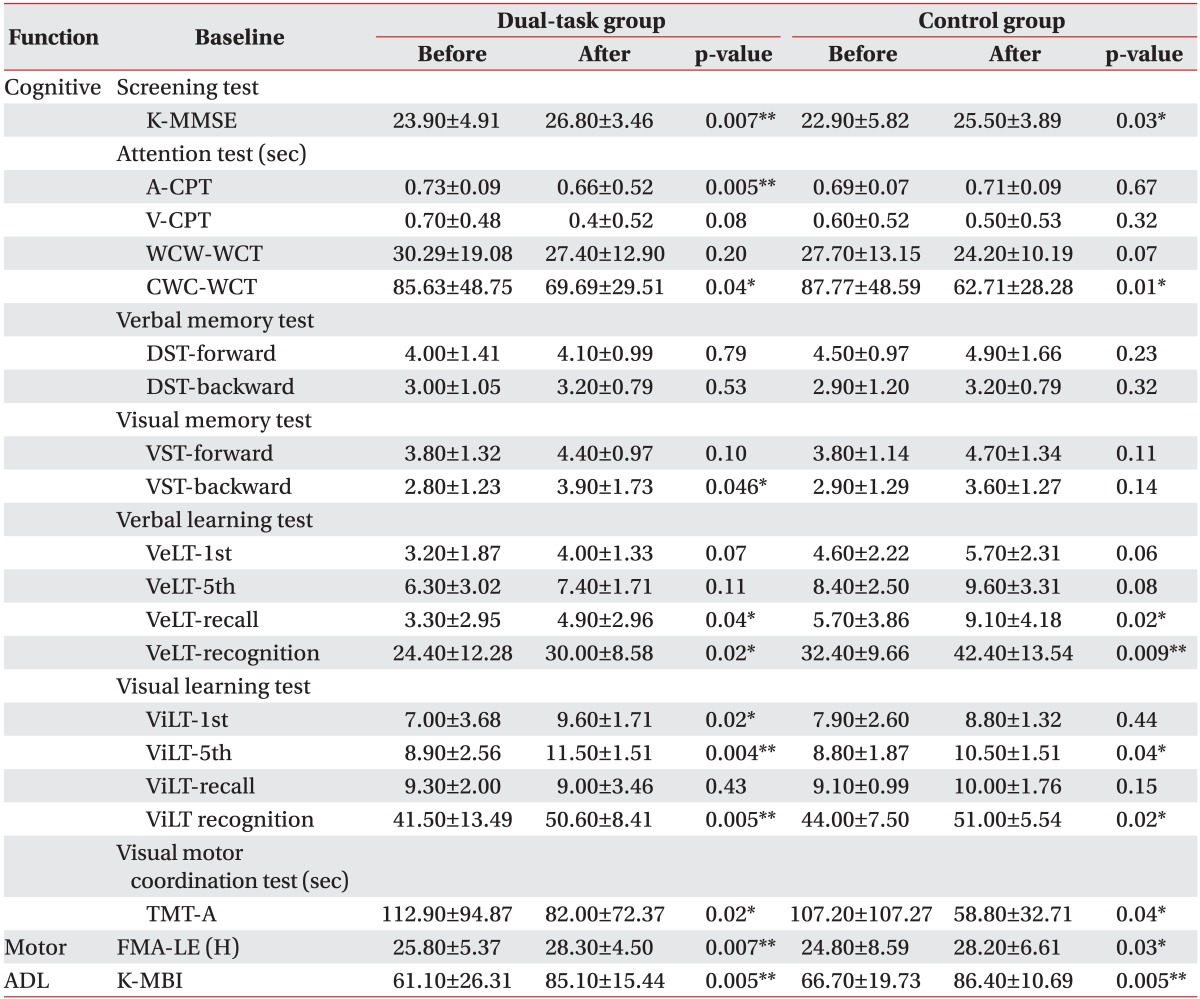
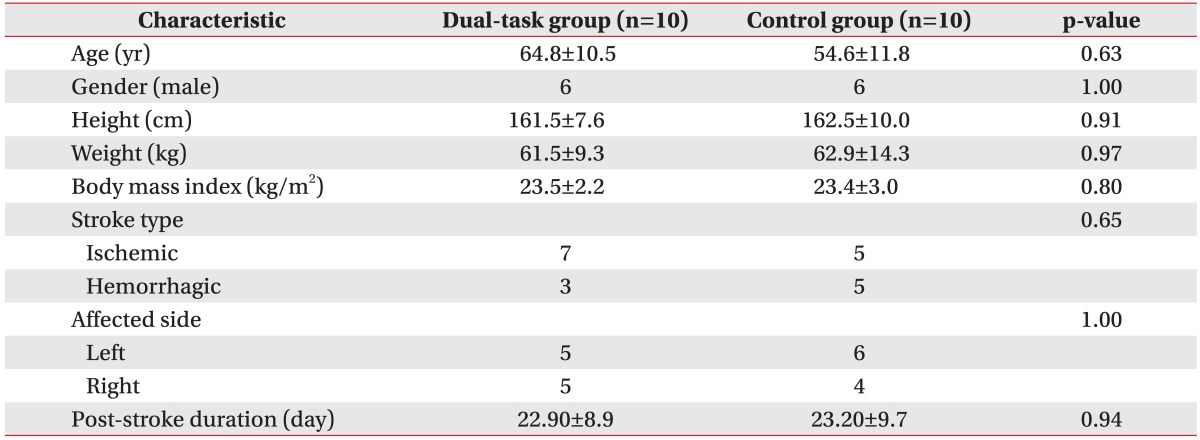
18. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc 1997;15:300-308.
19. Kim YH, Shin SH, Park SH, Ko MH. Cognitive assessment for patient with brain injury by computerized neuropsychological test. J Korean Acad Rehabil Med 2001;25:209-216.
20. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med 2007;31:283-297.
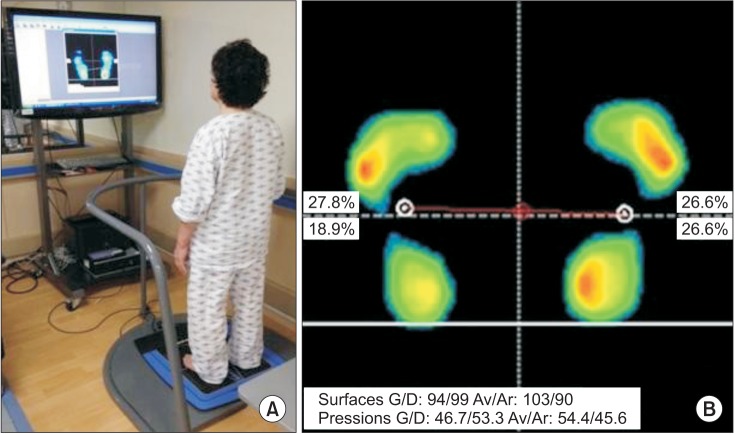
21. Hong SH, Im S, Park GY. The effects of visual and haptic vertical stimulation on standing balance in stroke patients. Ann Rehabil Med 2013;37:862-870. PMID:
24466521.



22. Gopalai AA, Senanayake SM, Kiong LC, Gouwanda D. Real-time stability measurement system for postural control. J Bodyw Mov Ther 2011;15:453-464. PMID:
21943619.


23. Lee SW, Shin DC, Song CH. The effects of visual feedback training on sitting balance ability and visual perception of patients with chronic stroke. J Phys Ther Sci 2013;25:635-639. PMID:
24259819.



24. French B, Thomas L, Leathley M, Sutton C, McAdam J, Forster A, et al. Does repetitive task training improve functional activity after stroke? A Cochrane systematic review and meta-analysis. J Rehabil Med 2010;42:9-14. PMID:
20111838.


25. Wevers L, van de Port I, Vermue M, Mead G, Kwakkel G. Effects of task-oriented circuit class training on walking competency after stroke: a systematic review. Stroke 2009;40:2450-2459. PMID:
19461035.


26. Bensoussan L, Viton JM, Schieppati M, Collado H, Milhe de, Mesure S, et al. Changes in postural control in hemiplegic patients after stroke performing a dual task. Arch Phys Med Rehabil 2007;88:1009-1015. PMID:
17678663.


27. Marshall SC, Grinnell D, Heisel B, Newall A, Hunt L. Attentional deficits in stroke patients: a visual dual task experiment. Arch Phys Med Rehabil 1997;78:7-12. PMID:
9014950.


28. Ben-Yishay Y, Piasetsky EB, Rattok J. A systematic method for ameliorating disorders in basic attention. In: Meier M, Benton A, Diller L, editors. Neuropsychological rehabilitation. New York: Guilford Press; 1987. p.165-181.
29. Lee SJ, Chun MH, Han EY, Lee JA. The correlation between postural control and attention during performance of dual task in stroke patients. J Korean Acad Rehabil Med 2010;34:20-26.


30. Hyndman D, Ashburn A. People with stroke living in the community: attention deficits, balance, ADL ability and falls. Disabil Rehabil 2003;25:817-822. PMID:
12851091.


31. McDowd JM, Filion DL, Pohl PS, Richards LG, Stiers W. Attentional abilities and functional outcomes following stroke. J Gerontol B Psychol Sci Soc Sci 2003;58:P45-P53. PMID:
12496301.



32. Robertson IH, Ridgeway V, Greenfield E, Parr A. Motor recovery after stroke depends on intact sustained attention: a 2-year follow-up study. Neuropsychology 1997;11:290-295. PMID:
9110335.