- Search
| Ann Rehabil Med > Volume 38(4); 2014 > Article |
Abstract
Objective
To investigate the effectiveness of commercial gaming-based virtual reality (VR) therapy on the recovery of paretic upper extremity in subacute stroke patients.
Methods
Twenty patients with the first-onset subacute stroke were enrolled and randomly assigned to the case group (n=10) and the control group (n=10). Primary outcome was measured by the upper limb score through the Fugl-Meyer Assessment (FMA-UL) for the motor function of both upper extremities. Secondary outcomes were assessed for motor function of both upper extremities including manual function test (MFT), box and block test (BBT), grip strength, evaluated for activities of daily living (Korean version of Modified Barthel Index [K-MBI]), and cognitive functions (Korean version of the Mini-Mental State Examination [K-MMSE] and continuous performance test [CPT]). The case group received commercial gaming-based VR therapy using Wii (Nintendo, Tokyo, Japan), and the control group received conventional occupational therapy (OT) for 30 minutes a day during the period of 4 weeks. All patients were evaluated before and after the 4-week intervention.
Results
There were no significant differences in the baseline between the two groups. After 4 weeks, both groups showed significant improvement in the FMA-UL, MFT, BBT, K-MBI, K-MMSE, and correct detection of auditory CPT. However, grip strength was improved significantly only in the case group. There were no significant intergroup differences before and after the treatment.
Stroke is one of the leading causes of disability in the world [1] and has a large impact on patients and their family members [2]. Neurological symptoms after a stroke vary according to the location and extent of the brain lesion, but motor weakness and cognitive impairment are the most frequently reported symptoms [3]. Immediately after a stroke, up to 85% of the survivors experience impairment of the hemiparetic upper extremity [4]. Eighty percent of these patients achieve their best upper extremity function within 3 weeks of stroke onset and 95% achieve it within 9 weeks [4]. However, between 55% and 75% of the stroke survivors have persistent functional limitations of the upper extremity, resulting in dependency for activities of daily living (ADL) [5]. Attention deficits are also commonly observed after stroke. Although the exact frequency is a matter of debate, the prevalence has been estimated to be 46%-92% in the acute phase [6] and 24%-51% at discharge [7,8]. One report suggested that up to 50% of the stroke survivors developed attention deficits that persisted for years after the stroke [9].
Since virtual reality (VR) technologies were first developed, VR-based therapy has been viewed as a promising rehabilitation tool [10]. VR-based therapy uses interactive simulations that are created by computer hardware and software to provide environments that mimic the real, three-dimensional environment, which encourage users to be engaged in activities [11] regardless of their physical disability. Currently, VR technologies in stroke rehabilitation have predominantly targeted motor recovery. A Cochrane review concluded that VR was an effective treatment for recovery of upper extremity motor function and ADL after stroke, when compared to the conventional rehabilitation therapy [12]. Furthermore, Kim et al. [13] demonstrated that VR training combined with computer-based cognitive rehabilitation had a significant effect on visual attention and short-term visuospatial memory in stroke patients with cognitive impairment.
Unfortunately, most VR interventions are hospital-based and have several obstacles to overcome, such as being expensive and bulky, and most of them are dependent on therapist. However, commercial computer gaming equipment uses a wireless controller to interact with the player through a motion detection system and avatar technology (e.g., Wii; Nintendo, Tokyo, Japan), and this has been used as a new style of VR equipment [14]. The commercial gaming is relatively cheap and easy to use, and a few studies have reported that it can promote motor recovery after stroke [14,15,16,17,18].
However, most of the existing trials were pilot studies [2,14,15,18,19] and they only compared commercial computer gaming to recreational therapy [2,14]. There is no study that has compared commercial computer gaming (Wii) with conventional occupational therapy (OT). Also, the existing studies only recruited patients with mild hemiparesis, because the intervention required the patient to grip the remote control [2,14]. In addition, although commercial gaming-based VR therapy is composed of complex activities using visual and auditory stimulation and requires continuous attention, there was no research about cognitive training by commercial gaming.
The aim of this study was to determine whether commercial gaming-based VR therapy was as effective as conventional OT for functional recovery of the hemiparetic upper extremity and attention deficits in subacute stroke patients.
Twenty patients who experienced a stroke for the first time within the last 3 months were recruited from the Department of Rehabilitation at Jeju National University Hospital between September 1, 2012 and June 30, 2013. Our protocol was reviewed and approved by the Institutional Review Board of Jeju National University Hospital, and all participants provided written informed consent before the selection procedure.
This was a randomized, single-blind study. Participants were randomly allocated in a 1:1 ratio to the 2 study groups. The randomization schedule was achieved by using a 'sealed envelope' technique. The assessor was blinded whether the participants were in case group or control group.
The study sample comprised of ten males and ten females with a mean age of 64.72±10.6 years. The inclusion criteria were as follows: 1) clinical diagnosis of subacute stroke confirmed by neuroimaging (computed tomography or magnetic resonance imaging), 2) hemiparesis of the upper extremity (upper limb score of the Fugl-Meyer Assessment <50), 3) a manual muscle testing (MMT) grade of more than 2/5 in the hemiparetic shoulder, and 4) ability to follow instructions that involved more than one step. The exclusion criteria were as follows: 1) cognitive dysfunction or aphasia severe enough to preclude task performance, 2) visual impairment or spatial neglect, 3) contracture or deformities in upper extremity, 4) metallic implants in the intracranial space or a pacemaker, and 5) previous history of epilepsy.
Participants were randomly assigned to the experimental group (n=10) or the control group (n=10). Participants in the experimental group received commercial gaming-based VR movement therapy using the Wii (Nintendo) for 30 minutes a day. Participants in the control group received conventional OT for 30 minutes a day. Both interventions were delivered five times a week for 4 weeks, and both groups also received conventional rehabilitation therapy except for OT.
To prevent further injury, all participants in the experimental group who had more than grade 2/5 and less than grade 3/5 in MMT of the shoulder wore a shoulder sling during the commercial gaming-based VR movement therapy under the supervision of occupational therapist. The patients in the experimental group who could not grip the remote control used a newly developed forearm orthosis which fixed the remote control onto the hemiparetic forearm with straps (Fig. 1). We use the Wii Sports Resort (Nintendo) program which consists of 12 games. The swordplay, table tennis, and canoe games were used in the current study, as these involve motor function and are of interest to older patients. The swordplay game involved performing flexion, extension, internal and external rotation of the shoulder, and flexion and extension of the elbow. The table tennis and canoe games also required upper extremity motions including internal and external rotation of the shoulder, flexion and extension of the elbow, and pronation and supination of the forearm. All the participants were instructed to play the games with their hemiparetic upper extremity. However, the patients who had motor weakness of proximal upper extremity of less than grade 3 in MMT were allowed to use non-paretic hand to support the hemiparetic side.
Conventional OT was goal-oriented and highly repetitive trainings assisted by occupational therapist. It was composed of stretching and strengthening exercises using full range of motion of the upper extremity, which was a task-oriented therapy for the ADL, fine motor training, and sensory motor recovery. The occupational therapist chose the appropriate tasks for the individual patient and developed them in stages.
Outcome measurements were evaluated before and at the end of the 4-week intervention in all participants.
The upper limb score in the Fugl-Meyer Assessment (FMA-UL) was used for primary outcome measure to assess the motor function of both upper extremities including the shoulder, elbow, forearm, wrist, and hand. The FMA-UL is widely used for comprehensive clinical examination of arm function, and the maximal score of FMA-UL is 66 points [20].
The patients were also evaluated of the upper extremity motor functions by manual function test (MFT), box and block test (BBT), and grip strength. The MFT consisted of 8 items as follows: forward and lateral elevation of the arm, touching the occiput and the back with the palm of the hand, grasping, pinching, carrying a cube, and pegboard manipulations. The MFT score ranged from 0 points (severely impaired) to 32 points (full function) [21]. The BBT was used to evaluate gross manual dexterity of the hemiparetic upper extremity. The number of cubes that the participant transferred during 1 minute was counted; a higher number indicated better function [22]. Grip strength of the paretic hand was evaluated using a dynamometer. The participant was seated with the hand resting comfortably on the laps and was instructed to flex the fingers maximally. The procedure was repeated three times and the highest score from the three trials was used for analysis [23].
The Korean version of the Mini-Mental State Examination (K-MMSE) was used to evaluate cognitive function [24]. The visual and auditory continuous performance tests (CPTs) of the computerized neuropsychological test (CNT; MaxMedica Inc., Seoul, Korea) were used to assess attention. Performance on the CPTs was quantified using reaction time and commission errors [25].
The Korean version of the Modified Barthel Index (K-MBI) was used to evaluate ADL function. The K-MBI was a reliable, valid tool for measuring the ADL of patients in Korea [26].
The change in each outcome measurement from pre- to post-intervention was evaluated separately in each group using a Wilcoxon signed-rank test. The change in each outcome measurement from pre- to post-intervention was compared between the two groups using a Mann-Whitney test. A p-value of less than 0.05 was considered as significant. Statistical analyses were performed using SPSS for Windows ver. 20 (IBM-SPSS Inc., Armonk, NY, USA).
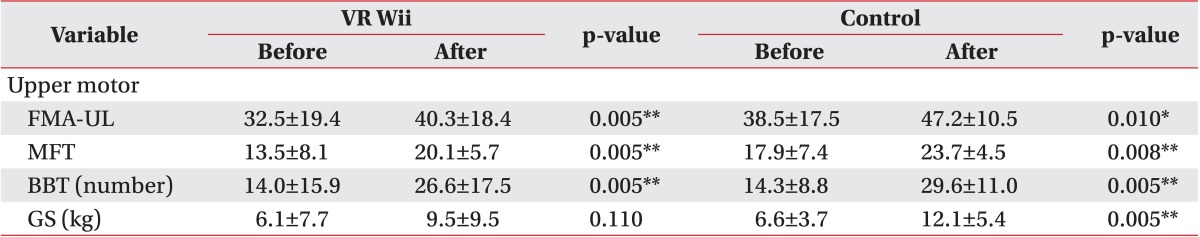
The baseline demographic characteristics of the participants are summarized in Table 1. Demographic characteristics including gender, age, body mass index, stroke type (ischemic or hemorrhagic), affected side (right or left), and the duration from stroke to the first evaluation were not significantly different between the two groups. Twenty-one patients were eligible, but one patient refused to consent. All 20 participants completed both treatments. None of the participants experienced a serious adverse event during the study period.
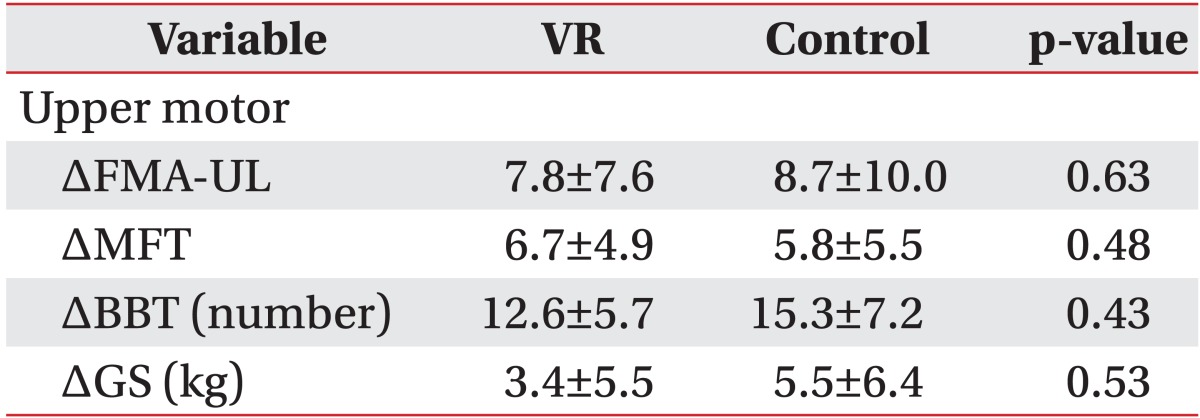
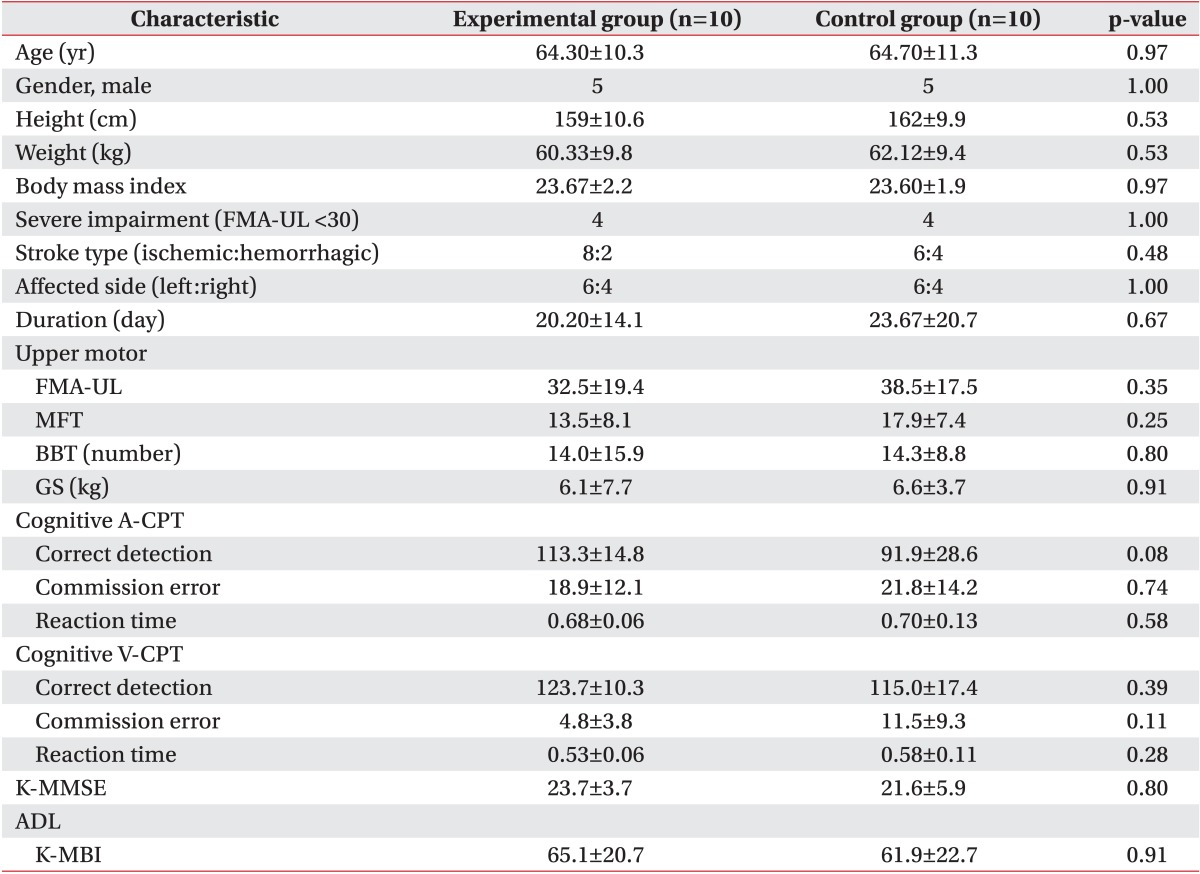
Hemiparetic upper extremity motor function outcomes score are presented in Tables 2 and 3. There were no significant differences between the two groups at baseline (Table 1). FMA-UL, MFT, and BBT scores improved from pre- to post-intervention in both groups. Grip strength of hemiparetic hand improved only in the control group (Table 2). There were no significant differences between the two groups before and after the 4-week intervention (Table 3).
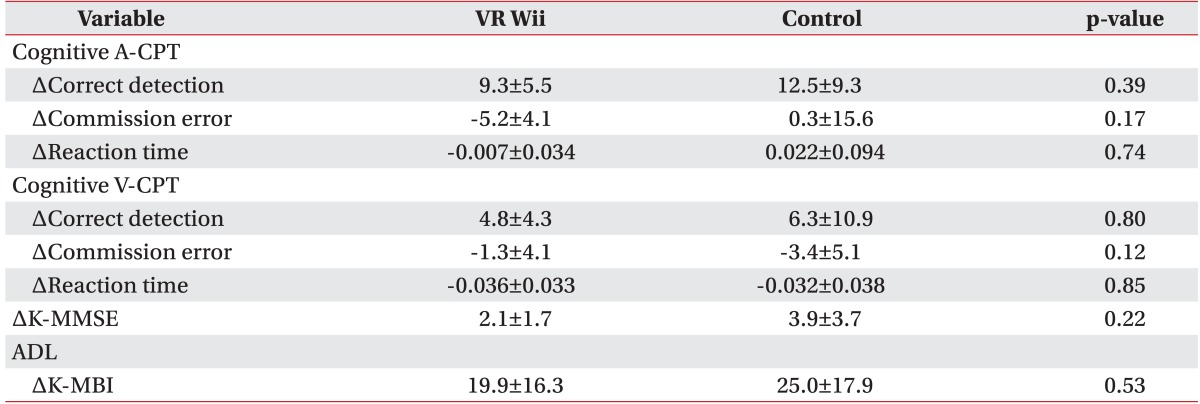
There were no significant differences between the two groups at baseline (Table 1). K-MMSE score, the number of correct detections in the auditory CPT, and K-MBI scores increased from pre- to post-intervention in both groups (Table 4). The number of commissure errors in the auditory CPT and number of correct detections in the visual CPT improved only in the experimental group (Table 4). The K-MMSE, visual and auditory CPT, and K-MBI scores did not reveal any statistical differences between the two groups before or after the 4-week intervention (Table 5).
Our results demonstrated that commercial gaming-based VR movement therapy was as effective as conventional OT for the recovery of upper extremity gross motor function and ADL in subacute stoke patients with moderate to severe motor impairment.
Coupar et al. [27] reported that the most significant predictor of upper limb recovery after stroke was the initial severity of motor impairment or function, and the severely hemiplegic patients might develop persistent disability. Therefore, various methods for gaining the best possible improvements in upper extremity function had been studied including bilateral movement therapy, constraint induced movement therapy, functional electrical stimulation, VR, and OT. Although there is no standard protocol for upper extremity therapy after a stroke, the current focus is on high-intensity, task-oriented, repetitive training of the paretic upper extremity [28,29].
Commercial gaming-based VR movement therapy would be an effective alternative to high-intensity, task-oriented, repetitive training after a stroke. However, the use of this therapy had been limited, because it could not be applied to patients who were unable to grip the remote control. We developed a forearm orthosis that could hold the remote control, and it enabled severely hemiparetic patients (FMA-UL <30) to participate in the VR movement therapy in the present study. We evaluated the function of the paretic upper extremity using the FMA-UL, MFT, BBT, and grip strength. The FMA-UL is a valid and reliable scale that is widely being used for comprehensive clinical examination of arm function [30], and we selected this as the primary outcome. The total FMA-UL is 66 points, and the scores between 50 and 65 indicate mild impairments, scores between 30 and 49 indicate moderate impairments, and scores below 30 indicate severe impairments [31,32]. After the 4-week intervention, both groups showed improvement in the score of FMA-UL. Also, both groups showed significant improvements in K-MBI, MFT, and BBT scores; but only the control group showed an improvement in hand grip strength. These results indicated that our VR movement therapy had significant effects on ADL and arm function, but not on hand grip strength. Cochrane review of VR for stroke reported that VR did not show significant differences in grip strength compared to alternative therapy [12,33]. The conclusion of our study is almost consistent with those of others described above, except that grip strength has been improved after the treatment only in control group. The lack of improvement in hand grip strength could be explained by several hypotheses. First, previous studies recruited patients with better functions in BBT and grip strength [14] or in FMA-UL [18], than those of our research. In the present study, the participants with severe hemiparesis who could not grip the remote control used a forearm orthosis to participate in the VR movement therapy. Therefore, they did not perform a hand grip movement during the therapy. Secondly, our VR movement therapy protocol consisted primarily of gross arm motions including shoulder, elbow, and forearm movements, and it did not include strengthening or fine motor training of the paretic hand and complex cognitive tasks.
Although we observed improvements in some CPT parameters, reaction time in the visual and auditory CPTs did not significantly change after the intervention. Therefore, the results showed incoherent findings in both groups; there was no difference in the changes from pre- to post-intervention between the experimental and control groups.
Specific cognitive training program were composed of various complex tasks including attention, memory, learning, and problem solving. Although our participants had to interact with computer-stimulated environment which required continuous attention to achieve higher score, our study did not provide any evidence supporting a sufficient, beneficial effect of commercial gaming-based VR movement therapy on attention.
Conventional OT is usually delivered in a hospital setting over a limited time frame, due to therapist-dependency and economic cost [34]. In contrast, commercial gaming-based VR movement therapy could provide continuous training of the upper limb, and it can be used at home or in a group setting. Commercial gaming was familiar, interesting, and cheaper than other VR methods used in a hospital setting. Additionally, commercial gaming-based VR movement therapy enhanced motivation and interest which in turn increased the patients' compliance [35,36]. It provided interactive stimulation and feedback [11], which is fundamental to motor skill learning [37]. In addition, higher motivation has been associated with better rehabilitation outcomes [35].
A recent systematic review confirmed the effect of VR therapy on upper limb recovery and ADL function after a stroke and highlighted the potential value of commercial VR gaming as a tool for stroke rehabilitation [12]. Our conclusion was consistent with this view. However, much more evidence is needed to establish a standardized protocol that would be targeted at the specific impairment and the ADL of stroke patients.
There were several limitations to our study. Firstly, we were unable to perform subgroup analyses according to the baseline severity of motor impairment, due to the small sample size. Secondly, although we randomly assigned the patients into each group, the study was single-blind and it is possible that patients using the new VR technology were more motivated than patients receiving OT. Thirdly, due to the short duration of treatment, we are unable to conclude on the long-term effect of commercial gaming-based VR movement therapy on upper extremity motor function, cognitive function, or ADL. Fourthly, the commercial gaming programs were too easy and simple to be used as a cognitive training method. Although it used visual and auditory stimulus, specific cognitive virtual reality program might be recommended for a cognitive training. Finally, commercial gaming programs were designed for healthy individuals and the feedbacks were provided based on the movement itself; but the target movements were not necessarily the ideal adaptive responses. As a result, supervision of the caregiver might be necessary in subsequent trials to optimize VR therapy.
Further research involving a larger sample size and long-term for follow-ups should be performed to compare participants according to the baseline severity of upper extremity impairments and to establish a standardized gaming program for post-stroke rehabilitation.
In conclusion, our findings demonstrated that the commercial gaming-based VR movement therapy was as effective as the conventional OT for functional recovery of upper extremity motor function and ADL function. Therefore, we suggest the commercial gaming-based VR movement therapy to be used as an alternative method for self-oriented or home-based occupational rehabilitation therapy for subacute stroke patients.
ACKNOWLEGMENTS
This work was supported by a research grant from Jeju National University Hospital in 2012.
References
1. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol 2009;8:345-354. PMID: 19233730.


2. Saposnik G, Mamdani M, Bayley M, Thorpe KE, Hall J, Cohen LG, et al. Effectiveness of Virtual Reality Exercises in Stroke Rehabilitation (EVREST): rationale, design, and protocol of a pilot randomized clinical trial assessing the Wii gaming system. Int J Stroke 2010;5:47-51. PMID: 20088994.



3. Balami JS, Chen RL, Buchan AM. Stroke syndromes and clinical management. QJM 2013;106:607-615. PMID: 23483140.



4. Nakayama H, Jorgensen HS, Raaschou HO, Olsen TS. Recovery of upper extremity function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil 1994;75:394-398. PMID: 8172497.


5. Nichols-Larsen DS, Clark PC, Zeringue A, Greenspan A, Blanton S. Factors influencing stroke survivors' quality of life during subacute recovery. Stroke 2005;36:1480-1484. PMID: 15947263.


6. Stapleton T, Ashburn A, Stack E. A pilot study of attention deficits, balance control and falls in the subacute stage following stroke. Clin Rehabil 2001;15:437-444. PMID: 11518445.


7. Hyndman D, Pickering RM, Ashburn A. The influence of attention deficits on functional recovery post stroke during the first 12 months after discharge from hospital. J Neurol Neurosurg Psychiatry 2008;79:656-663. PMID: 17872979.


8. Rasquin SM, Lodder J, Ponds RW, Winkens I, Jolles J, Verhey FR. Cognitive functioning after stroke: a one-year follow-up study. Dement Geriatr Cogn Disord 2004;18:138-144. PMID: 15211068.


9. Barker-Collo S, Feigin VL, Parag V, Lawes CM, Senior H. Auckland Stroke Outcomes Study. Part 2: Cognition and functional outcomes 5 years poststroke. Neurology 2010;75:1608-1616. PMID: 21041784.


10. Weiss PL, Rand D, Katz N, Kizony R. Video capture virtual reality as a flexible and effective rehabilitation tool. J Neuroeng Rehabil 2004;1:12PMID: 15679949.



11. Weiss PL, Kizony R, Feintuch U, Katz N. Virtual reality in neurorehabilitation. In: Selzer M, Clarje S, Cohen L, Duncan P, Gage F, editors. Textbook of neural repair and neurorehabilitation: medical neurorehabilitation. Cambridge: Cambridge University Press; 2006. p.182-197.
12. Laver K, George S, Thomas S, Deutsch JE, Crotty M. Virtual reality for stroke rehabilitation. Stroke 2012;43:e20-e21.

13. Kim BR, Chun MH, Kim LS, Park JY. Effect of virtual reality on cognition in stroke patients. Ann Rehabil Med 2011;35:450-459. PMID: 22506159.



14. Saposnik G, Teasell R, Mamdani M, Hall J, McIlroy W, Cheung D, et al. Effectiveness of virtual reality using Wii gaming technology in stroke rehabilitation: a pilot randomized clinical trial and proof of principle. Stroke 2010;41:1477-1484. PMID: 20508185.



15. Celinder D, Peoples H. Stroke patients' experiences with Wii Sports during inpatient rehabilitation. Scand J Occup Ther 2012;19:457-463. PMID: 22339207.


16. Henderson A, Korner-Bitensky N, Levin M. Virtual reality in stroke rehabilitation: a systematic review of its effectiveness for upper limb motor recovery. Top Stroke Rehabil 2007;14:52-61. PMID: 17517575.

17. Leder RS, Azcarate G, Savage R, Savage S, Sucar LE, Reinkensmeyer D, et al. Nintendo Wii remote for computer simulated arm and wrist therapy in stroke survivors with upper extremity hemiparesis. Proceedings of the Virtual Rehabilitation Conference 2008 Aug 25-27; Vancouver, Canada. pp 74.
18. Mouawad MR, Doust CG, Max MD, McNulty PA. Wii-based movement therapy to promote improved upper extremity function post-stroke: a pilot study. J Rehabil Med 2011;43:527-533. PMID: 21533334.


19. Hurkmans HL, Ribbers GM, Streur-Kranenburg MF, Stam HJ, van den. Energy expenditure in chronic stroke patients playing Wii Sports: a pilot study. J Neuroeng Rehabil 2011;8:38PMID: 21756315.



20. Sanford J, Moreland J, Swanson LR, Stratford PW, Gowland C. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Phys Ther 1993;73:447-454. PMID: 8316578.



21. Moriyama S. Occupational therapy in stroke rehabilitation with reference to early stage program. Proceedings of the Joint Japanese-China Stroke Conference. Ikarigaseki, Japan: Reimeikyo Rehabilitation Hospital; 1987. p.114-124.
22. Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the Box and Block Test of manual dexterity. Am J Occup Ther 1985;39:386-391. PMID: 3160243.


23. Sunderland A, Tinson D, Bradley L, Hewer RL. Arm function after stroke: an evaluation of grip strength as a measure of recovery and a prognostic indicator. J Neurol Neurosurg Psychiatry 1989;52:1267-1272. PMID: 2592969.



24. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc 1997;15:300-308.
25. Riccio CA, Reynolds CR, Lowe P, Moore JJ. The continuous performance test : a window on the neural substrates for attention? Arch Clin Neuropsychol 2002;17:235-272. PMID: 14589726.



26. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med 2007;31:283-297.
27. Coupar F, Pollock A, Rowe P, Weir C, Langhorne P. Predictors of upper limb recovery after stroke: a systematic review and meta-analysis. Clin Rehabil 2012;26:291-313. PMID: 22023891.


28. Dobkin BH. Training and exercise to drive poststroke recovery. Nat Clin Pract Neurol 2008;4:76-85. PMID: 18256679.




29. Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol 2009;8:741-754. PMID: 19608100.


30. Platz T, Pinkowski C, van Wijck F, Kim IH, di Bella P, Johnson G. Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block Test: a multicenter study. Clin Rehabil 2005;19:404-411. PMID: 15929509.


31. Faria-Fortini I, Michaelsen SM, Cassiano JG, Teixeira-Salmela LF. Upper extremity function in stroke subjects: relationships between the international classification of functioning, disability, and health domains. J Hand Ther 2011;24:257-264. PMID: 21420279.


32. Michaelsen SM, Dannenbaum R, Levin MF. Task-specific training with trunk restraint on arm recovery in stroke: randomized control trial. Stroke 2006;37:186-192. PMID: 16339469.


33. Housman SJ, Scott KM, Reinkensmeyer DJ. A randomized controlled trial of gravity-supported, computer-enhanced arm exercise for individuals with severe hemiparesis. Neurorehabil Neural Repair 2009;23:505-514. PMID: 19237734.


34. Nef T, Quinter G, Müller R, Riener R. Effects of arm training with the robotic device ARMin I in chronic stroke: three single cases. Neurodegener Dis 2009;6:240-251. PMID: 19940461.


35. Merians AS, Jack D, Boian R, Tremaine M, Burdea GC, Adamovich SV, et al. Virtual reality-augmented rehabilitation for patients following stroke. Phys Ther 2002;82:898-915. PMID: 12201804.


36. Jack D, Boian R, Merians AS, Tremaine M, Burdea GC, Adamovich SV, et al. Virtual reality-enhanced stroke rehabilitation. IEEE Trans Neural Syst Rehabil Eng 2001;9:308-318. PMID: 11561668.


37. Adams JA, Goetz ET, Marshall PH. Response feedback and motor learning. J Exp Psychol 1972;92:391-397. PMID: 5060708.



Fig. 1
Newly adopted device is orthosis with straps that fixed the remote control onto the hemiparetic forearm on the patients who could not grip remote controller.

Table 1
Baseline demographic characteristics of the participants
Values are presented as mean±standard deviation or number.
FMA-UL, upper limb score in the Fugl-Meyer Assessment; MFT, manual function test; BBT, box and block test; GS, grip strength; A-CPT, auditory continuous performance test; V-CPT, visual continuous performance test; K-MMSE, Korean version of the Mini-Mental State Examination; K-MBI, Korean version of the Modified Barthel Index.
Table 4
Cognitive function and ADL before and after treatment
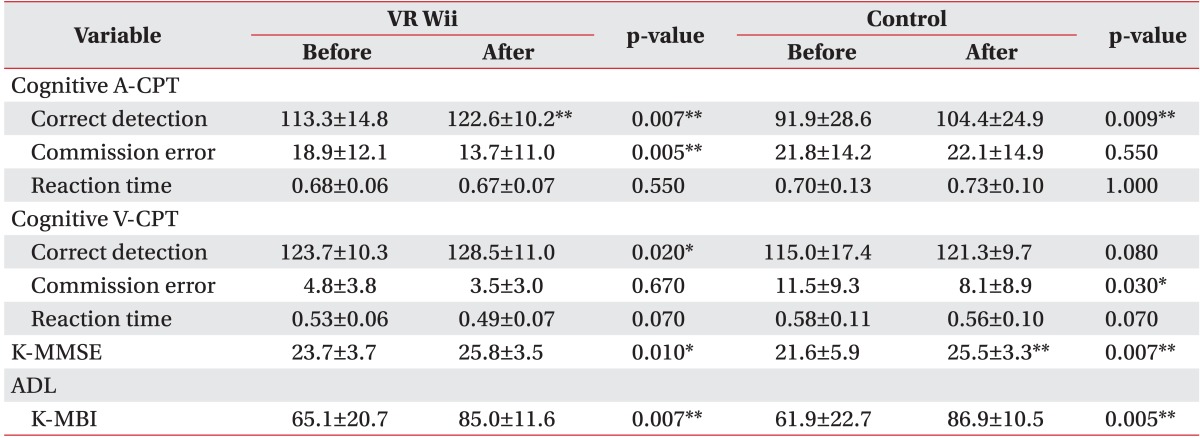
Values are presented as mean±standard deviation.
ADL, activities of daily living; A-CPT, auditory continuous performance test; V-CPT, visual continuous performance test; K-MMSE, Korean version of the Mini-Mental State Examination; K-MBI, Korean version of the Modified Barthel Index.
*p<0.05, **p<0.01.