- Search
| Ann Rehabil Med > Volume 36(3); 2012 > Article |
Abstract
Stump neuroma is a common cause of pain from disorganized proliferation of nerve fascicles occurring after limb amputation. Ultrasound guided alcohol injection in painful stump neuroma has been tried as a new treatment approach. Herein, we report 2 male patients, who had traumatic amputation and claimed severe and diffuse burning pain in the stump area. Neuroma at the distal end of an amputated nerve was clearly identified on sonography. The patients gradually developed increasing severe pain that could not be managed with conservative care. They were treated with neurolysis using alcohol solution. Using ultrasonographical guidance, 1.2 ml of 100% dehydrated alcohol was injected into the nerves proximal to neuroma. No complications occurred. The patients were initially pain free. After a few months, however, their stump pain recurred slightly. Repeat neurolysis was performed using 0.3 ml of 100% dehydrated alcohol. During the three months follow-up period, mild stump pain occurred but the patients did not require any analgesics.
Chronic residual limb pain following amputation is a major problem for many patients. The most common causes are complex regional pain syndrome (CRPS) type II, phantom limb pain or stump neuroma.1 Stump neuroma is a disorganized proliferation of nerve fascicles developing after limb amputation. Surgical intervention is commonly used for the treatment of painful neuroma. However, surgery-related complications, such as wound infection or dehiscence, persistent erythema, hypertrophic scar and local recurrence, have been reported.2 Recently, local injection therapy using steroid, alcohol, phenol or glycerol has been introduced for the treatment of neuroma.3 Ultrasonography has become the preferred technique for visualization and localization of the lesion. Under ultrasonographic examination, biopsy or fine needle aspiration for more accurate positive diagnosis was also available.2 Since alcohol neurolysis has many advantages compared to surgery, such as no systemic side effects, relatively long-term effectiveness and allowing for early ambulation, it is currently becoming a promising treatment for Morton's neuroma.4-6 However, there are few reports of stump neuroma treated by alcohol injection under sonographic guide. Herein, we report with a literature review, two cases of painful stump neuroma after limb amputation, which were successfully treated by ultrasonographically guided alcohol neurolysis.
A 57-year-old male had received left below-knee amputation and autogenous skin graft in another hospital, due to an accident which occurred on March 24 2007, when he slid into a de-icing machine. The patient was transferred to the Department of Physical Medicine and Rehabilitation at our hospital 2 weeks after the accident. The patient was on anti-hypertensive medication, but did not suffer from other underlying diseases, such as diabetes or vascular diseases. Application of the prosthesis was performed after muscle strengthening exercise and knee joint stretching exercise, massage over the distal stump and desensitization training. As the partial thickness wound and pain caused by attaching the prosthesis posed difficulty to rehabilitation training, we tried to adjust the prosthesis many times, but the symptoms were not improved. Stump revision was performed once at the Department of Orthopedic Surgery of our hospital, to manage stump wound which persistently occurred for more than 5 months after the accident. Subsequently, the wound was healed. After the amputation stump matured and scar was formed, the prosthesis of lower extremities was replaced with a new custom prosthesis. However, the stump pain has persisted since then and did not respond to various analgesics, including acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), tramadol hydrochloride and oxycodone hydrochloride. When the prosthesis was fitted, persistent and unbearably excruciating pain at the stump site precluded the patient from doing rehabilitation program, including gait training.
During physical examination performed on May 16 2008, mild skin scraping and erythema, but no edema or adhesion were observed at the amputation site, within the prosthetic socket. The range of motion (ROM) during knee flexion and extension above the amputation site was normal. Manual muscle testing found that the muscle strength of flexors and extensors of the left hip and knee was decreased by 20%, compared to those of the right hip and knee. A small, palpable, movable mass was observed in the lateral side of the amputation stump, near the amputation site of fibula. Hyperalgesia and hyperpathia developed in response to light palpation. The level of produced pain evaluated on the visual analog scale (VAS) pain rating was 10.
Neurological examination revealed no abnormal findings and the patient did not complain of phantom limb pain. The prosthesis was well adjusted to fit the patient's amputation stump, but the patient developed a gingerly gait and circumduction gait, in order to reduce the weight load which caused pain on the affected side.
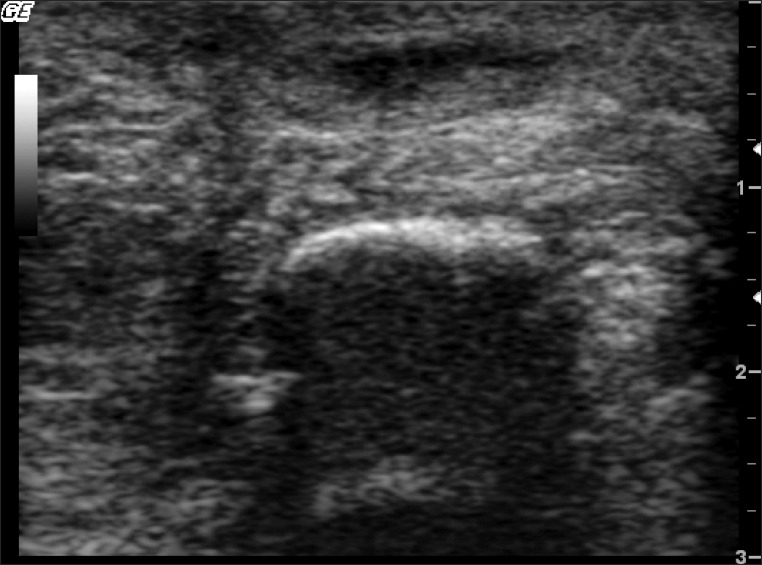
Radiological examination found that the left tibia and fibula were amputated, the length of remaining tibia from the knee joint was 14.4 cm, and there was spur formation. Ultrasonography LOGIQ 5 PRO (GE Healthcare Korea, Seoul, Korea) revealed discrete hypoechoic mass (1.55├Ś0.67├Ś0.35 cm3) in the distal stump, directly continuous to the common peroneal nerve (Fig. 1), which was consistent with ultrasonographic findings of neuroma. When the neuroma was pressed using a linear transducer (10 MHz), extreme pain was produced again.
The patient received an information packet providing him with the risks and benefits of the procedure. We gave him plenty of time to ask any questions. After describing the procedure to the patient, we obtained written informed consent.
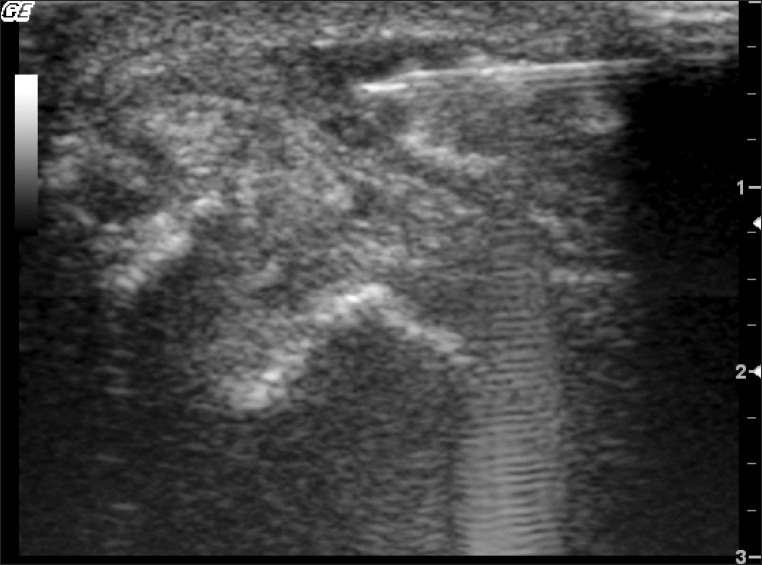
We performed the ultrasound-guided injection of dehydrate alcohol into the stump neuroma. The patient was placed in supine position, the region of injection site was sterilized with betadine and alcohol and reconfirming the location of neuroma using ultrasound guidance. A 22-gauge, 3.2-cm, short beveled needle was advanced into the neuroma under real-time control and used to inject 1.2 ml of 100% alcohol solution 100% dehydrated alcohol (Daihan Pharmacy, Seoul, Korea). Following injection, we observed the spread of alcohol within the lesion on sonography (Fig. 2). The pain significantly reduced immediately after injection and the patient complained of numbness around the injection site, but there were no specific side effects. During the outpatient follow-up observation, the patient complained of moderate reoccurring pain. The visual analogue scale was 7 points. Over 50 days after the first neurolysis, a second alcohol neurolysis was conducted using a smaller amount (0.3 ml) of alcohol, and subsequently the patient's VAS pain rating was reduced to 3 point. Thereafter, the patient has not experienced much pain or has encountered much difficulty in leading a normal life and walking with prosthesis. There were no side effects.
A 81-year-old male had received a left above-knee amputation in another hospital due to shrapnel wounds which occurred about 60 years ago when he fought in the Korean War. The patient was admitted to the Department of Physical Medicine and Rehabilitation of our hospital on August 27, 2010. The patient had a history of diabetes mellitus, asthma and benign prostate hypertrophy. Since about ten years ago, the patient has gradually developed increasingly severe pain that could not be managed with various analgesics, including acetaminophen, NSAIDs, tramadol hydrochloride and oxycodone hydrochloride. The patient received an orientation and reported sharp, stabbing, excruciating pain rated between 8 and 9 on the VAS pain rating at the stump site, when the stump end was touched.
At physical examination, the stump showed good healing of the incision, with no evidence of erythema, ecchymosis, edema or skin breakdown. The ROM of the hip above the amputation site was normal. Manual muscle testing found that the muscle strength of flexors, extensors, abductor, adductor, internal and external rotator of the left hip were decreased by about 20%, compared to those of the right hip. Hyperalgesia and hyperpathia developed in response to light palpation.
Neurological examination revealed no abnormal findings. Although he had some evidence of phantom limb pain, it was insignificant compared to the localized stump pain.
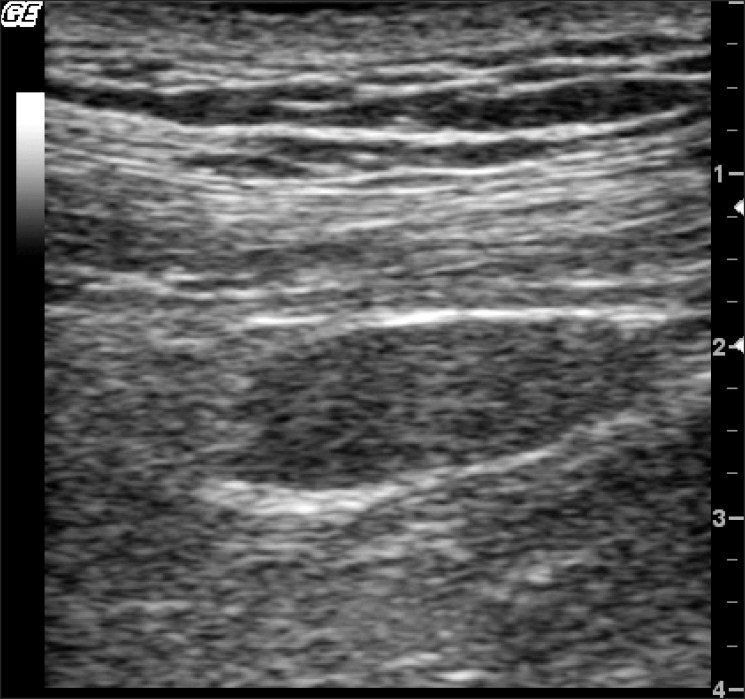
Radiological examination found that the left femur shaft was amputated, the length of remaining femur from the hip joint was 26.6 cm and there was spur formation. Ultrasonography revealed discrete hypoechoic mass (2.76├Ś2.74├Ś0.95 cm3) in the distal stump, directly continuous to the sciatic nerve (Fig. 3), which was con sistent with ultrasonographic findings of neuroma. When the neuroma was pressed using a linear transducer (10 MHz), extreme pain was produced again.
On the basis of the history and physical examination, we felt that the sciatic nerve block at the distal end of the transected sciatic nerve would be the best way to treat the neuroma pain. After describing the procedure to the patient, we obtained written informed consent.
We performed the ultrasound-guided injection of dehydrate alcohol into the stump neuroma. The patient was placed in prone position. After identifying the nerve at the mid-thigh level, we followed it distally until it disappeared about 5 cm from the end of the stump. The region of injection site was sterilized with betadine and alcohol and the location of neuroma was reconfirmed using ultrasound guidance. A 23-gauge 5-cm, short-beveled needle was advanced into the neuroma under real-time control, and used to inject 1.2 ml of 100% alcohol solution 100% dehydrated alcohol (Daihan Pharmacy, Seoul, Korea). Following injection, we observed the spread of alcohol within the lesion on sonography (Fig. 4). The pain significantly reduced immediately after injection and the VAS pain rating decreased to 4 points. There were no specific side effects. During the outpatient follow-up observation, the patient claimed that his pain had recurred, although it only reached a severity of 7 on the VAS pain rating. Over 100 days after the first neurolysis, a second alcohol neurolysis was conducted using a smaller amount (0.3 ml) of alcohol, and subsequently the patient's VAS pain rating was reduced to 3 points. Thereafter, the patient has not experienced much pain and there were no side effects.
Post-amputation pain is a significant clinical problem that interferes with the rehabilitation of amputees. Neuroma forming at the cut end of the nerve is one of major causes of stump pain.2 There are many medical or surgical options for the treatment of stump neuromas. Medication combined with nerve block on the distal portion of neuroma is one of the most useful conservative treatment options. Surgery is also a well-established treatment. However, there is high likelihood of surgery-related morbidities or recurrence.7,8
Injection of local anesthetics or steroid into symptomatic Morton's neuroma has been used for many years. Injection of local steroids has also been used to treat stump pain; however, its long term effectiveness does not seem to be convincing. Furthermore, repeated steroid injections have associated complications, such as atrophy of skin and/or subcutaneous fat or hyperpigmentation.2,5 Chemical neurolysis using alcohol, which is also known as alcohol sclerotherapy, has been widely used to treat Morton's neuroma. Ethanol injected around the nerve pro duces chemical neurolysis through dehydration, necrosis and precipitation of protoplasm. In addition, alcohol inhibits the function of neurotransmitter receptor and the ATP-gated ion channel interacting with a small hydrophobic pocket on the receptor protein.4-6 Ultrasonographically guided injection using steroids, phenol or norepinephrine has also recently been tried in patients with stump neuroma.2,3,9
Under ultrasonographic examination, the normal nerve appears to have a linear fascicular structure, whereas neuroma is readily identifiable as a hypoechoic mass arising from the terminal nerve, which is also well distinguished from the adjacent hyperechoic scar tissue.10 When ultrasonographic findings are not diagnostic, application of fine needle aspiration, biopsy or the pressure triggering test using a transducer is also available to confirm the diagnosis. Under real time ultrasonographic control, it is possible to appropriately position the tip of the injection needle in the neuroma, as well as to assess for leak of alcohol outside the lesion. Therefore, ultrasonographic guidance assists in performing an accurate procedure and minimizes the injection-related complications.
Previous studies reported that repeated injection (up to 4 times) using low concentration alcohol (20-30%) showed good clinical outcomes in patients with Morton's neuroma.5 In our patient, we injected two times using 100% alcohol, and the patient's symptom was remarkably improved, without any complication. Thus, we consider that US-guided injection therapy using high concentration alcohol could be a successful therapeutic option for the treatment of stump neuroma.
References
1. Fischler AH, Gross JB. Ultrasound-guided sciatic neuroma block for treatment of intractable stump pain. J Clin Anesth 2007;19:626-628. PMID: 18083479.


2. Ernberg LA, Adler RS, Lane J. Ultrasound in the detection and treatment of a painful stump neuroma. Skeletal Radiol 2003;32:306-309. PMID: 12719933.


3. Gruber H, Kovacs P, Peer S, Frischhut B, Bodner G. Sonographically guided phenol injection in painful stump neuroma. AJR 2004;182:952-954. PMID: 15039170.


4. Fanucci E, Masala S, Fabiano S, Perugia D, Squillaci E, Varrucciu V, Simonetti G. Treatment of intermetatarsal Morton's neuroma with alcohol injection under US guide: 10-month follow-up. Eur Radiol 2004;14:514-518. PMID: 14531002.


5. Hughes RJ, Ali K, Jones H, Kendall S, Connell DA. Treatment of Morton's neuroma with alcohol injection under sonographic guidance: follow-up of 101 cases. AJR 2007;188:1535-1539. PMID: 17515373.


6. Hyer CF, Mehl LR, Block AJ, Vancourt RB. Treatment of recalcitrant intermetatarsal neuroma with 4% sclerosing alcohol injection: a pilot study. J Foot Ankle Surg 2005;44:287-291. PMID: 16012436.


7. Lewin-Kowalik J, Marcol W, Kotulska K, Mandera M, Klimczak A. Prevention and management of painful neuroma. Neurol Med Chir (Tokyo) 2006;46:62-67. PMID: 16498214.


8. Thomas AJ, Bull MJ, Howard AC, Saleh M. Peri operative ultrasound guided needle localisation of amputation stump neuroma. Injury 1999;30:689-691. PMID: 10707244.


9. Lin EE, Horasek S, Agarwal S, Wu CL, Raja SN. Local administration of norepinephrine in the stump evokes dose-dependent pain in amputees. Clin J Pain 2006;22:482-486. PMID: 16772803.