1. Gombatto SP, Brock T, DeLork A, Jones G, Madden E, Rinere C. Lumbar spine kinematics during walking in people with and people without low back pain. Gait Posture 2015;42:539-544. PMID:
26380913.


2. Lamoth CJ, Meijer OG, Daffertshofer A, Wuisman PI, Beek PJ. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: changes in motor control. Eur Spine J 2006;15:23-40. PMID:
15864670.


3. Lamoth CJ, Meijer OG, Wuisman PI, van Dieen JH, Levin MF, Beek PJ. Pelvis-thorax coordination in the transverse plane during walking in persons with nonspecific low back pain. Spine (Phila Pa 1976) 2002;27:E92-E99. PMID:
11840116.


4. Savigny P, Watson P, Underwood M. Guideline Development Group. Early management of persistent non-specific low back pain: summary of NICE guidance. BMJ 2009;338:b1805. PMID:
19502217.


5. Steele J, Bruce-Low S, Smith D, Jessop D, Osborne N. Lumbar kinematic variability during gait in chronic low back pain and associations with pain, disability and isolated lumbar extension strength. Clin Biomech (Bristol, Avon) 2014;29:1131-1138.


6. Steele J, Bruce-Low S, Smith D, Jessop D, Osborne N. A randomized controlled trial of limited range of motion lumbar extension exercise in chronic low back pain. Spine (Phila Pa 1976) 2013;38:1245-1252. PMID:
23514876.


7. van den Hoorn W, Bruijn SM, Meijer OG, Hodges PW, van Dieen JH. Mechanical coupling between transverse plane pelvis and thorax rotations during gait is higher in people with low back pain. J Biomech 2012;45:342-347. PMID:
22078275.


8. Vogt L, Pfeifer K, Portscher M, Banzer W. Influences of nonspecific low back pain on three-dimensional lumbar spine kinematics in locomotion. Spine (Phila Pa 1976) 2001;26:1910-1919. PMID:
11568705.


9. Kim T, Chai E. Trunk and pelvic coordination at various walking speeds during an anterior load carriage task in subjects with and without chronic low back pain. J Phys Ther Sci 2015;27:2353-2356. PMID:
26311982.



10. McGinley JL, Baker R, Wolfe R, Morris ME. The reliability of three-dimensional kinematic gait measurements: a systematic review. Gait Posture 2009;29:360-369. PMID:
19013070.


11. Andersson EI, Lin CC, Smeets RJ. Performance tests in people with chronic low back pain: responsiveness and minimal clinically important change. Spine (Phila Pa 1976) 2010;35:E1559-E1563. PMID:
20634779.


12. Malliou P, Gioftsidou A, Beneka A, Godolias G. Measurements and evaluations in low back pain patients. Scand J Med Sci Sports 2006;16:219-230. PMID:
16895526.


13. Baker R. Measuring walking: a handbook of clinical gait analysis. London: Mac Keith Press; 2013.
14. Mieritz RM, Bronfort G, Kawchuk G, Breen A, Hartvigsen J. Reliability and measurement error of 3-dimensional regional lumbar motion measures: a systematic review. J Manipulative Physiol Ther 2012;35:645-656. PMID:
23158469.


15. Niknam H, Esteki A, Salavati M, Kahrizi S. Reliability of Zebris motion analysis system in healthy athletes and athletes with anterior cruciate ligament reconstruction. Asian J Sports Med 2017;8:e42040.

16. McDermott A, Bolger C, Keating L, McEvoy L, Meldrum D. Reliability of three-dimensional gait analysis in cervical spondylotic myelopathy. Gait Posture 2010;32:552-558. PMID:
20832318.


17. de Vet HC, Terwee CB, Ostelo RW, Beckerman H, Knol DL, Bouter LM. Minimal changes in health status questionnaires: distinction between minimally detectable change and minimally important change. Health Qual Life Outcomes 2006;4:54PMID:
16925807.



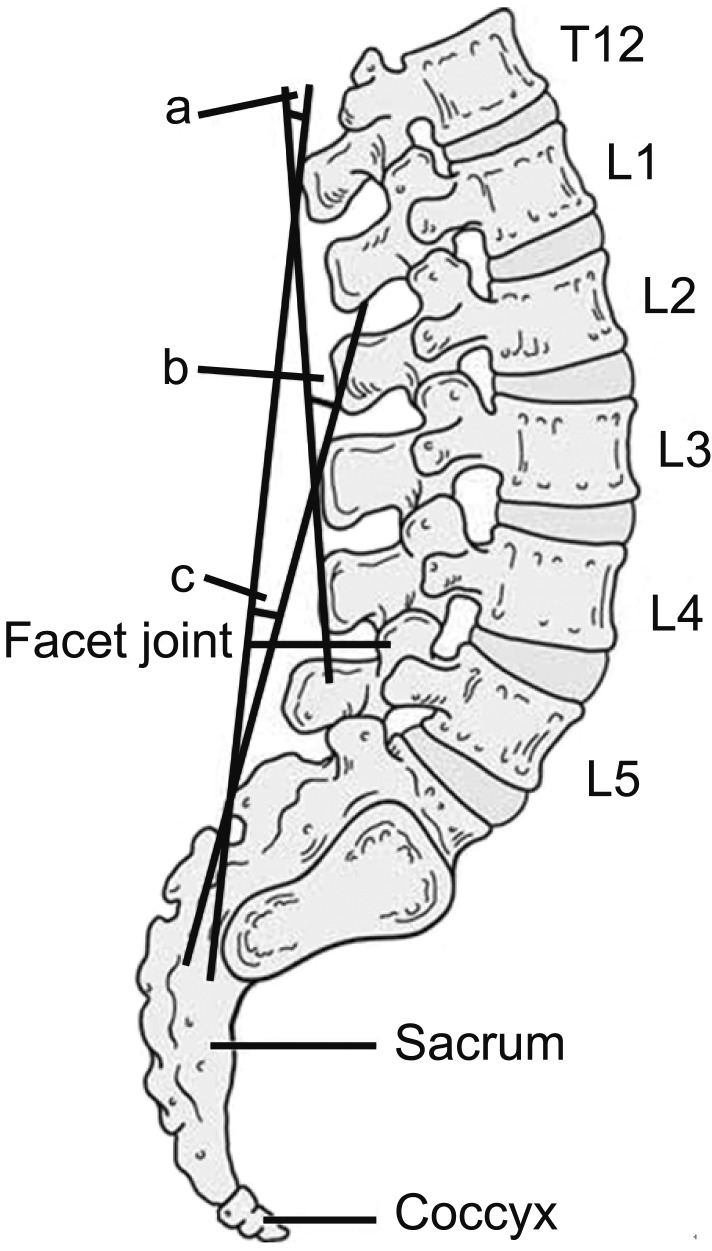
18. Parkinson S, Campbell A, Dankaerts W, Burnett A, O'Sullivan P. Upper and lower lumbar segments move differently during sit-to-stand. Man Ther 2013;18:390-394. PMID:
23473753.


20. Dvorak J, Vajda EG, Grob D, Panjabi MM. Normal motion of the lumbar spine as related to age and gender. Eur Spine J 1995;4:18-23. PMID:
7749901.


21. Hidalgo B, Gilliaux M, Poncin W, Detrembleur C. Reliability and validity of a kinematic spine model during active trunk movement in healthy subjects and patients with chronic non-specific low back pain. J Rehabil Med 2012;44:756-763. PMID:
22847223.


23. Mieritz RM, Bronfort G, Jakobsen MD, Aagaard P, Hartvigsen J. Reliability and measurement error of sagittal spinal motion parameters in 220 patients with chronic low back pain using a three-dimensional measurement device. Spine J 2014;14:1835-1843. PMID:
24216400.


24. Fernandes R, Armada-da-Silva P, Pool-Goudzwaard AL, Moniz-Pereira V, Veloso AP. Three dimensional multi-segmental trunk kinematics and kinetics during gait: Test-retest reliability and minimal detectable change. Gait Posture 2016;46:18-25. PMID:
27131171.


25. Fernandes R, Armada-da-Silva P, Pool-Goudzwaard AL, Moniz-Pereira V, Veloso AP. Test-retest reliability and minimal detectable change of three-dimensional gait analysis in chronic low back pain patients. Gait Posture 2015;42:491-497. PMID:
26349524.


26. Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. Oxford: Oxford University Press; 2015.
27. Haghdoost AA, Mirzazadeh A, Alikhani S. Secular trend of height variations in Iranian population born between 1940 and 1984. Iran J Public Health 2008;37:1-7.
28. Drake R, Vogl AW, Mitchell AW. Gray's anatomy for students. 2nd ed. Philadelphia: Churchill Livingstone; 2009.
29. Whittle MW, Levine D. Measurement of lumbar lordosis as a component of clinical gait analysis. Gait Posture 1997;5:101-107.

30. Wagner JM, Rhodes JA, Patten C. Reproducibility and minimal detectable change of three-dimensional kinematic analysis of reaching tasks in people with hemiparesis after stroke. Phys Ther 2008;88:652-663. PMID:
18326055.



31. Akhbari B, Salavati M, Mohammadi F, Safavi-Farokhi Z. Intra- and inter-session reliability of static and dynamic postural control in participants with and without patellofemoral pain syndrome. Physiother Can 2015;67:248-253. PMID:
26839452.



32. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155-163. PMID:
27330520.



33. Mason DL, Preece SJ, Bramah CA, Herrington LC. Reproducibility of kinematic measures of the thoracic spine, lumbar spine and pelvis during fast running. Gait Posture 2016;43:96-100. PMID:
26546409.


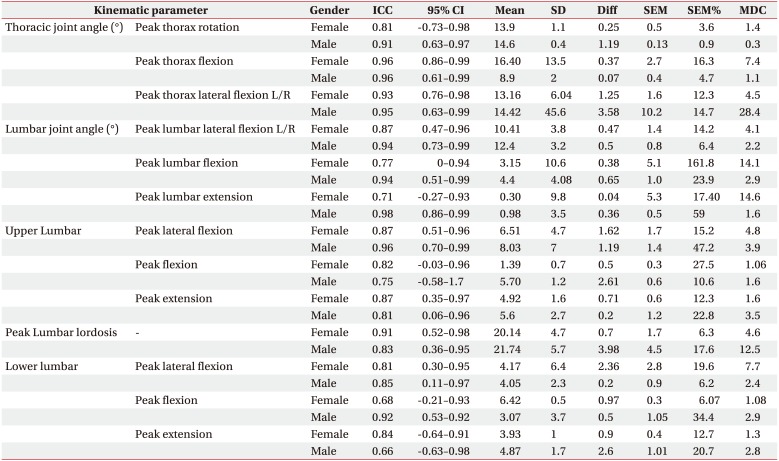
 is used to account for variance in the two measurement sessions [21].
is used to account for variance in the two measurement sessions [21]. method [21] was used for SEM. SEMs for most trunk and lumbar movements generally remained constant in both gender groups. It seems that there is a difference in SEM between men and women for deviation. Generally, females had higher SEMs relative to males in most trunk and lumbar movements except for lower lumbar sagittal plane movements. However, most of these observed error values could be due to higher SDs and higher between-day movement variability in this group (female) of patients [10] caused by gait disturbance due to CLBP. It has been reported that females have higher values of SDs of mean in most trunk and lumbar movements due to movement variability [18,22,23,32]. SEMs obtained in our study were lower than around 5° for both gender groups. These results are reasonable according to previous studies [10,33]. However, when the measurement error is higher than 2°, this may require consideration during data interpretation [10]. This means that the difference between two measurements is small and these parameters are useful. They are particularly appropriate for detecting changes in these participants.
method [21] was used for SEM. SEMs for most trunk and lumbar movements generally remained constant in both gender groups. It seems that there is a difference in SEM between men and women for deviation. Generally, females had higher SEMs relative to males in most trunk and lumbar movements except for lower lumbar sagittal plane movements. However, most of these observed error values could be due to higher SDs and higher between-day movement variability in this group (female) of patients [10] caused by gait disturbance due to CLBP. It has been reported that females have higher values of SDs of mean in most trunk and lumbar movements due to movement variability [18,22,23,32]. SEMs obtained in our study were lower than around 5° for both gender groups. These results are reasonable according to previous studies [10,33]. However, when the measurement error is higher than 2°, this may require consideration during data interpretation [10]. This means that the difference between two measurements is small and these parameters are useful. They are particularly appropriate for detecting changes in these participants.