- Search
| Ann Rehabil Med > Volume 38(1); 2014 > Article |
Abstract
Objective
To compare fluid thickeners composed of starch polysaccharide (STA), guar gum-based polysaccharide (GUA), and xanthan gum-based polysaccharide (XAN) with the use of a viscometer and a line spread test (LST) under various measurement conditions.
Methods
The viscosity of thickened fluid with various concentrations (range, GUA 1%-4%, XAN 1%-6%, STA 1%-7%, at intervals of 1%) was measured with a rotational viscometer with various shear rates (1.29 s-1, 5.16 s-1, 51.6 s-1, and 103 s-1) at a temperature of 35в„ғ, representing body temperature. The viscosity of STA showed time dependent alteration. So STA was excluded. Viscosities of GUA and XAN (range of concentration, GUA 1%-3%, XAN 1%-6%, at intervals of 1%) were measured at a room temperature of 20в„ғ. LST was conducted to compare GUA and XAN (concentration, 1.5%, 2.0%, and 3.0%) at temperatures of 20в„ғ and 35в„ғ.
Results
The viscosities of 1% GUA and XAN were similar. However, viscosity differences between GUA and XAN were gradually larger as concentration increased. The shear thinning effect, the inverse relationship between the viscosity and the shear rate, was more predominant in XAN than in GUA. The results of LST were not substantially different from GUA and XAN, in spite of the difference in viscosity. However manufacturers' instructions do not demonstrate the rheological properties of thickeners.
Conclusion
The viscosities of thickened fluid were different when the measurement conditions changed. Any single measurement might not be sufficient to determine comparable viscosity with different thickeners. Clinical decision for the use of a specific thickener seems to necessitate cautious consideration of results from a viscometer, LST, and an expert's opinion.
Dysphagia, or swallowing disorder, is caused by many neurologic or structural diseases affecting oral, pharyngeal, and esophageal structures [1]. The prevalence of dysphagia is known to be 15% for older adults [2], 30% for older adults in hospital admission [3], and 35%-64% in patients following stroke [4-6]. The complications of dysphagia, such as aspiration pneumonia [7,8], dehydration, and malnutrition [9], increased the length of hospital stay and mortality [10].
Diet modification is widely administered in dysphagia patients for safe and adequate nutrition [11,12]. The thickened fluid is known to reduce the risk of aspiration [13,14]. However, pudding-like ultrathick fluid could increase pharyngeal retention [13]. Furthermore dysphagia patients who consume thickened fluid have a risk of dehydration [15]. Therefore it is important to achieve the adequate viscosity of a thickened fluid. The National Dysphagia Diet Task Force (NDDTF) proposed to classify thickened fluids to 4 classes by viscosity at a shear rate of 50 s-1 and a temperature of 25в„ғ: thin (1-50 mPaВ·s), nectar-like (51-350 mPaВ·s), honey-like (351-1,750 mPaВ·s), and spoon-thick (>1,751 mPaВ·s) [16]. Paik et al. [17] also presented 4 levels of dysphagia diets according to line spread test (LST) and viscosity: water (LST, >4.0 cm; 1-9 mPaВ·s), fluid-type yogurt (LST, 3.0-3.9 cm; 10-99 mPaВ·s), honey (LST, 1.1-2.9 cm; 100-9,999 mPaВ·s), and pudding (LST, 0-1.0 cm; >10,000 mPaВ·s).
The available fluid thickeners are mainly composed of starch polysaccharide, Guar gum-based polysaccharide, and Xanthan gum-based polysaccharide. The rheological characteristics of these fluid thickeners are different [18-20]. Viscosity of fluid changes as the measuring conditions, including temperature and shear rate, are altered. The amount of viscosity change between various measuring conditions is different in these fluid thickeners. Thus, the aim of this study is to investigate the comparability of fluid thickeners made of different gum-based and starch-based substances by viscosity and LST under various measurement conditions.
This study was the preliminary study to determine the equal dose of thickeners for a clinical trial which was conducted to compare the influence of thickeners on the swallowing function. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital.
Three powdered commercial thickeners were used: guar gum-based thickener (GUA: Toromi-Up; Nisshin OilliO Group Ltd., Yokohama, Japan), xanthan gum-based thickener (XAN: Neo-hightoromeal 3; Food Care Inc., Kanagawa, Japan), and starch-based thickener (STA: Thick & Easy; American Institutional Products Inc., Lancaster, PA, USA). Thickeners were mixed in water for 5 minutes before testing.
Viscosity was obtained by a rotational viscometer (Physica, standard measuring drive system SM-LM; Physica Messtechnik GmbH, Stuttgart, Germany) (Fig. 1A) under various conditions. The rotational viscometer evaluates the viscosity by measuring the torque needed to maintain a constant rotational speed [21]. The viscosity can be determined at a predefined temperature and at a predefined shear rate. The unit of viscosity was chosen to be millipascal-second (mPaВ·s). First, three thickeners of various concentrations (range, GUA 1%-4%, XAN 1%-6%, STA 1%-7%, at intervals of 1%) were examined with various shear rates (1.29 s-1, 5.16 s-1, 51.6 s-1, and 103 s-1) at 35в„ғ, representing body temperature. The viscosity of STA changed predominantly as time passed after mixing. So we excluded STA due to inability to maintain equal viscosity during the experiment. Second, viscosity was measured at different concentrations (range, GUA 1%-3%, XAN 1%-6%, at intervals of 1%), with various shear rates (1.29 s-1, 5.16 s-1, 51.6 s-1, and 103 s-1), at room temperature of 20в„ғ.
LST (Fig. 1B) was performed to compare GUA and XAN at various concentrations (1.5%, 2.0%, and 3.0%) with two different temperatures (20в„ғ and 35в„ғ) [22]. LST was conducted using a flat template on which premeasured concentric rings were drawn. The thickener was placed in an open ended tube. The tube was lifted and the thickener was allowed to flow for 1 minute. The distance of the thickener which dispersed was measured with 90В° increments.
The viscosities of three thickeners at 35в„ғ measured by rotational viscometer with various shear rates are presented in Fig. 2. At a shear rate of 1.29 s-1 (Fig. 2A), the viscosities of the two gum-based thickeners were similar at a concentration of 2% (GUA 9,560 mPaВ·s; XAN 9,160 mPaВ·s) and the viscosity of 3% GUA (27,600 mPaВ·s) was similar to 5% XAN (25,000 mPaВ·s). As shear rate increased, the viscosities of the three thickeners decreased. At a shear rate of 51.6 s-1, assumed for normal swallowing [16] (Fig. 2C), the viscosities were similar to 3% GUA (2,030 mPaВ·s), 6% XAN (1,880 mPaВ·s), and 7% STA (1,820 mPaВ·s). The viscosity of 1% XAN was bigger than that of 1% GUA at shear rates of 1.29 s-1 and 5.16 s-1. However the viscosity of 1% XAN was smaller at shear rates of 51.6 s-1 and 103 s-1.
Fig. 3 shows the viscosities of GUA and XAN measured at 20в„ғ. The viscosity of GUA was decreasing as temperature decreased. XAN showed higher viscosity at 20в„ғ than that at 35в„ғ. At a shear rate of 51.6 s-1, the viscosity of 3% GUA (1,660 mPaВ·s) was similar to that of 5% XAN (1,620 mPaВ·s). The viscosity of 1% XAN was bigger than that of 1% GUA at shear rates of 1.29 s-1, 5.16 s-1, and 51.6 s-1. However the viscosity of 1% XAN was smaller at a shear rate of 103 s-1.
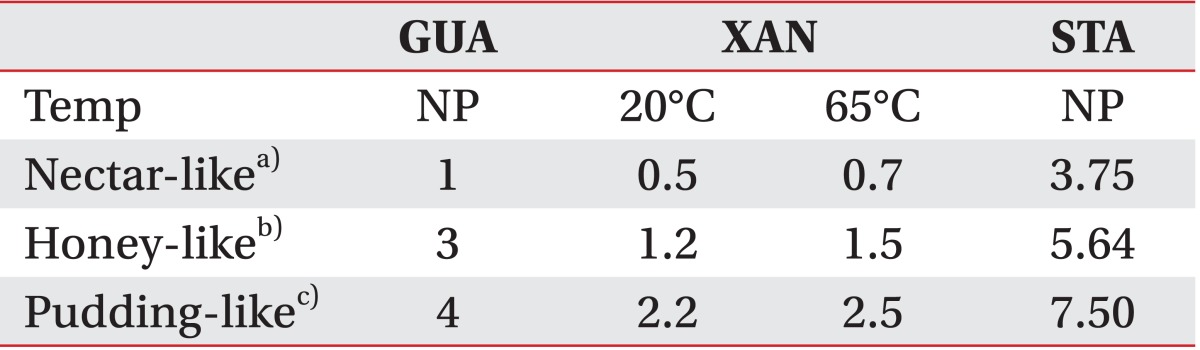
The result of LST is presented in Table 1. There was no substantial difference between GUA and XAN. With 3% concentration, both thickener recorded less than 1 cm. With 1.5% of concentration, GUA showed longer distance of dispersion than XAN. The extent of flow with 2% concentration was larger at 35в„ғ than that at 20в„ғ.
In this study, we evaluate the viscosities of three thickeners under various conditions. The viscosity of thickened fluid changed substantially as the measurement conditions changed. Thus, NDDTF suggested the range of viscosity to categorize the thickened fluid measured under constant condition to be a shear rate of 50 s-1 and a temperature of 25в„ғ [16]. Furthermore, the viscosity of STA showed time-dependent alteration. The time-dependent characteristics of STA correspond with the results of an earlier study which reported that the viscosity of STA exhibited a decrease followed by an increase [23]. Consequently STA has a limitation to maintain constant thickness. Viscosity differences between GUA and XAN became greater as the concentration increased.
The viscosity of the fluid represents an inverse relationship to temperature [20]. Results of the present study are consistent with previous studies, except in the viscosity of GUA. In this study, the viscosity of GUA was slightly lower at 20в„ғ than that at 35в„ғ. Casas et al. [24] reported that the viscosity of GUA decreased as temperature increased. It is presumed that the dissolution temperature and time for mixing affected GUA solubility. Casas et al. [24] stirred GUA for 1 hour at 300 rpm. Thereafter, undissolved GUA was separated using a centrifuge. However, thickeners were mixed for 5 minutes. So the viscosity was higher at 35в„ғ because undissolved GUA might be dissolved as the temperature increased. Insoluble GUA at a lower temperature would dissolve after a temperature increase up to 60в„ғ due to the dissolved polymer fraction [24]. Additionally, it is known that cold temperature reduces the pharyngeal transit time of dysphagia patients due to stroke [25].
The viscosities of the three thickened fluids decreased as shear rate increased. These results are known as "shear-thinning," which is the characteristic of non-Newtonian fluids [16] and is in agreement with previous studies [18,26]. The shear-thinning was more prominent in XAN than in GUA. This rheological feature is due to chemical properties including high molecular weight and a rigid rod-like conformation of XAN [18].
Normal shear rate of swallowing was estimated from 1 s-1 to 1,000 s-1 [27]. As previously mentioned, NDDTF adopted a constant shear rate of 50 s-1 as a national standard for comparing the products [16]. However, the normal shear rate of swallowing is controversial and changes during swallowing process [16,28]. Additionally, the shear rate of dysphagia patients is not well-known and might depend on pathophysiology. For instance, the shear rate would be low in patients who have difficulty in propelling the food [28]. Therefore it would be inappropriate in some patients to prescribe thickened fluid due to a criteria measuring at a shear rate 50 s-1.
LST is a simple and economic test to determine the viscosity of a fluid [22]. However, in this study LST results of GUA and XAN were similar in spite of the difference between the viscosities of 3% GUA (1,660 mPaВ·s at 20в„ғ and 2,030 mPaВ·s at 35в„ғ at a shear rate of 51.6 s-1) and 3% XAN (945 mPaВ·s at 20в„ғ and 765 mPaВ·s at 35в„ғ at a shear rate of 51.6 s-1). Furthermore, the results of LST are consistent with a previous study that stated LST did not correctly reflect the change of viscosity due to temperature [29]. Adeleye and Rachal [29] described that the results of LST were not significantly different although the viscosities measured by a viscometer at 10в„ғ and 20в„ғ were different. Nicosia and Robbins [30] reported that LST could differentiate a broad category of fluids but could not compare different types of fluids. It is proposed that results of LST reflect not only viscosity but also surface tension and density [30].
The summary of manufacturers' instructions to thicken fluids is summarized in Table 2. Instructions have limited information of fluid thickeners. There is no information about temperature except for that of XAN. Additionally, the standardization of the nomenclature of fluid thickeners is needed because the instruction of XAN uses terminologies, such as "French dressing-like," "sauce of pork cutlets-like," and "ketchup-like" which are different from other thickeners. It is probably due to the absence of national guidelines for fluid thickeners in Korea. Therefore it is needed to establish guidelines for fluid thickeners considering the rheological properties of thickeners.
This study has some limitations. First, measurement conditions did not cover a wide range of temperatures. We measured viscosity at 20в„ғ and 35в„ғ, representing room and body temperature. However, some fluids, such as a cold beverage or a soup, could be over the range. Second, we did not evaluate the viscosity with thickener mixed with a substance other than water, such as soup or milk. Rheological properties of thickened soup or milk would be different.
In conclusion, we evaluated the viscosity of various thickeners at various conditions. Viscosities of thickened fluids changed as measurement conditions changed. The viscosity of STA was hard to maintain due to time dependent alteration. The viscosities of GUA and XAN were similar at a concentration of 1%. The viscosities of GUA were higher than those of XAN as concentration increased. Additionally, shear-thinning was notable in XAN. The results of LST were not suitable to compare fluid thickeners made of different components. Rheological properties of various thickeners were different. However, there was limited information in the manufacturer's instruction. Therefore, further research is needed to develop the diet modification guidelines for dysphagia patients.
References
1. Braddom RL, Chan L, Harrast MA, Kowalske KJ, Matthews DJ, Ragnarsson KT, et al. Physical medicine and rehabilitation. 4th ed. Philadelphia, PA: Saunders; 2011.
2. Barczi SR, Sullivan PA, Robbins J. How should dysphagia care of older adults differ? Establishing optimal practice patterns. Semin Speech Lang 2000;21:347-361. PMID: 11085258.



3. Lee A, Sitoh YY, Lieu PK, Phua SY, Chin JJ. Swallowing impairment and feeding dependency in the hospitalised elderly. Ann Acad Med Singapore 1999;28:371-376. PMID: 10575521.

4. Mann G, Hankey GJ, Cameron D. Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis 2000;10:380-386. PMID: 10971024.


5. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke 1999;30:744-748. PMID: 10187872.


6. Paciaroni M, Mazzotta G, Corea F, Caso V, Venti M, Milia P, et al. Dysphagia following stroke. Eur Neurol 2004;51:162-167. PMID: 15073441.


7. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging 2012;7:287-298. PMID: 22956864.


8. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2005;36:2756-2763. PMID: 16269630.


9. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke: does dysphagia matter? Stroke 1996;27:1200-1204. PMID: 8685928.


10. Altman KW, Yu GP, Schaefer SD. Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg 2010;136:784-789. PMID: 20713754.


11. Curran J, Groher ME. Development and dissemination of an aspiration risk reduction diet. Dysphagia 1990;5:6-12. PMID: 2202558.


13. Kuhlemeier KV, Palmer JB, Rosenberg D. Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia 2001;16:119-122. PMID: 11305221.


14. Diniz PB, Vanin G, Xavier R, Parente MA. Reduced incidence of aspiration with spoon-thick consistency in stroke patients. Nutr Clin Pract 2009;24:414-418. PMID: 19483070.


15. Whelan K. Inadequate fluid intakes in dysphagic acute stroke. Clin Nutr 2001;20:423-428. PMID: 11534937.


16. National Dysphagia Diet Task Force. National dysphagia diet: standardization for optimal care. Chicago, IL: American Dietetic Association; 2002.
17. Paik NJ, Han TR, Park JW, Lee EK, Park MS, Hwang IK. Categorization of dysphagia diets with the line spread test. Arch Phys Med Rehabil 2004;85:857-861. PMID: 15129413.


18. Seo CW, Yoo B. Steady and dynamic shear rheological properties of gum-based food thickeners used for diet modification of patients with dysphagia: effect of concentration. Dysphagia 2013;28:205-211. PMID: 23179025.


19. Garcia JM, Chambers E 4th, Matta Z, Clark M. Viscosity measurements of nectar- and honey-thick liquids: product, liquid, and time comparisons. Dysphagia 2005;20:325-335. PMID: 16633878.


20. Garcia JM, Chambers E 4th, Matta Z, Clark M. Serving temperature viscosity measurements of nectar- and honey-thick liquids. Dysphagia 2008;23:65-75. PMID: 17602262.


21. Rosencranz R, Bogen SA. Clinical laboratory measurement of serum, plasma, and blood viscosity. Am J Clin Pathol 2006;125(Suppl): S78-S86. PMID: 16830959.



22. Mann LL, Wong K. Development of an objective method for assessing viscosity of formulated foods and beverages for the dysphagic diet. J Am Diet Assoc 1996;96:585-588. PMID: 8655906.


23. Dewar RJ, Joyce MJ. Time-dependent rheology of starch thickeners and the clinical implications for dysphagia therapy. Dysphagia 2006;21:264-269. PMID: 17216389.


24. Casas JA, Mohedano AF, Garcia-Ochoa F. Viscosity of guar gum and xanthan/guar gum mixture solutions. J Sci Food Agric 2000;80:1722-1727.

25. Cola PC, Gatto AR, Silva RG, Spadotto AA, Schelp AO, Henry MA. The influence of sour taste and cold temperature in pharyngeal transit duration in patients with stroke. Arq Gastroenterol 2010;47:18-21. PMID: 20520970.



26. O'Leary M, Hanson B, Smith C. Viscosity and non-Newtonian features of thickened fluids used for dysphagia therapy. J Food Sci 2010;75:E330-E338. PMID: 20722917.


27. Shama F, Sherman P. Identification of stimuli controlling the sensory evaluation of viscosity: II. Oral methods. J Texture Stud 1973;4:111-118.

28. Cichero JA, Jackson O, Halley PJ, Murdoch BE. How thick is thick? Multicenter study of the rheological and material property characteristics of mealtime fluids and videofluoroscopy fluids. Dysphagia 2000;15:188-200. PMID: 11014881.


29. Adeleye B, Rachal C. Comparison of the rheological properties of ready-to-serve and powdered instant food-thickened beverages at different temperatures for dysphagic patients. J Am Diet Assoc 2007;107:1176-1182. PMID: 17604748.


30. Nicosia MA, Robbins J. The usefulness of the line spread test as a measure of liquid consistency. Dysphagia 2007;22:306-311. PMID: 17581694.


Fig.В 1
Measurement of viscosity. (A) Schematic diagram of rotational viscometer. (B) Line spread test.

Fig.В 2
Viscosities of thickeners based on guar gum, xanthan gum, and starch measured at 35в„ғ. Viscosities at various shear rates: (A) 1.29 s-1, (B) 5.16 s-1, (C) 51.6 s-1, and (D) 103 s-1. GUA, guar gum-based thickener; XAN, xanthan gum-based thickener; STA, starch-based thickener.

Fig.В 3
Viscosities of thickeners based on guar gum and xanthan gum measured at 20в„ғ. Viscosities at various shear rates: (A) 1.29 s-1, (B) 5.16 s-1, (C) 51.6 s-1, and (D) 103 s-1. GUA, guar gum-based thickener; XAN, xanthan gum-based thickener.