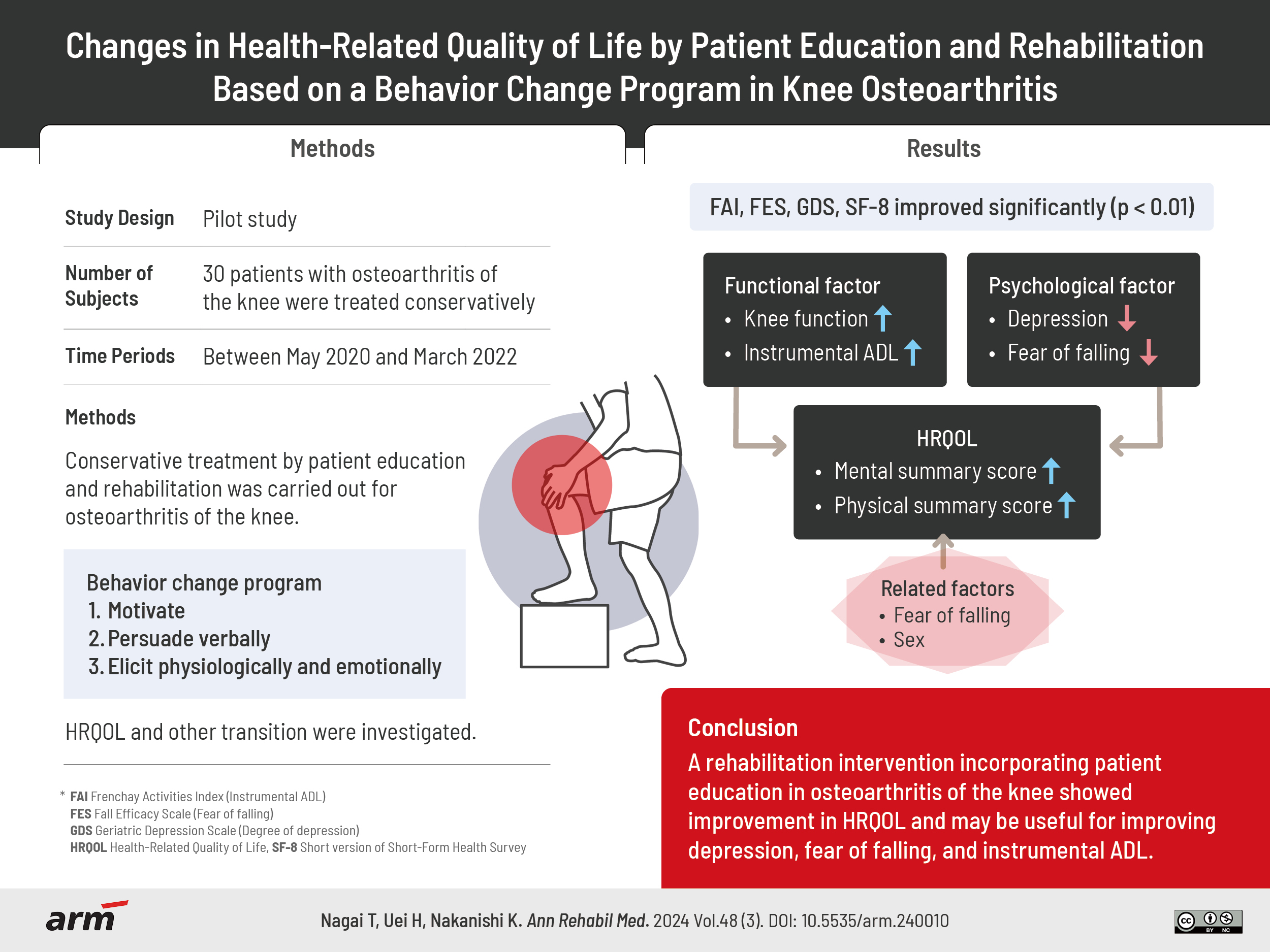
Changes in Health-Related Quality of Life by Patient Education and Rehabilitation Based on a Behavior Change Program in Knee Osteoarthritis
Article information
Abstract
Objective
The purpose of this study was to examine how rehabilitation and patient education for knee osteoarthritis improves health-related quality of life (HRQOL) and to identify factors influencing HRQOL.
Methods
Between May 2020 and March 2022, 30 patients with osteoarthritis of the knee were treated conservatively and rehabilitated with a patient education program. The patient education program was based on the health belief model by Sedlak et al., and patient education using pamphlets was provided during the rehabilitation intervention. The survey items were patient basic information, instrumental activities of daily living (ADL) (FAI), fear of falling (FES), degree of depression (GDS), HRQOL (SF-8), knee function assessment (JOA score), and X-ray classification (K-L classification), and the survey method was a self-administered questionnaire at the start of rehabilitation, 1 month after the intervention, and at the end of the rehabilitation intervention. We examined factors affecting the physical component summary (PCS) and mental component summary (MCS) of HRQOL scores.
Results
JOA score, FES, FAI, GDS, and SF-8 improved significantly (p<0.01). MCS was also negatively correlated with FES and age (r=-0.486, -0.368). Sex was extracted as a factor for PCS as a factor affecting HRQOL (p<0.01). MCS was extracted with FES as a factor (p=0.046).
Conclusion
A rehabilitation intervention incorporating patient education in osteoarthritis of the knee showed improvement in HRQOL and may be useful for improving depression, fear of falling, and instrumental ADL.
INTRODUCTION
Knee osteoarthritis is one of the representative motor disorders in the elderly [1]. The number of patients with knee osteoarthritis in Japan is estimated to be 25.3 million, and the need for medical intervention as a common disease is inevitably increasing [2]. It can also be a risk of locomotive syndrome, which limits daily activities and increases the risk of nursing care [3]. There is also a risk that pain from knee osteoarthritis reduces exercise opportunities, leading to decreased activity and quality of life. Park et al. [4] suggest that knee osteoarthritis is significantly associated with decreased mental health and health-related quality of life (HRQOL). We verified and informed the time-dependent change of HRQOL by the rehabilitation intervention on 62 cases of old osteoarthritis patients treated conservatively [5]. As a result, knee function, fear of falling, and instrumental activities of daily living (ADL) was significantly improved from the start of rehabilitation to 3 months after the intervention. However, there was no improvement in depression and HRQOL scores, physical component score and mental component score. It is necessary to establish treatment measures based on psychological factors such as depression caused by chronic pain in knee osteoarthritis. Meeus et al. [6] reported on the effects of patient education, which improved psychological factors related to pain. Snyder and Engström [7] reported on the effectiveness of oral and pamphlet teaching as a method of patient education and described its effectiveness.
Therefore, for patients with knee osteoarthritis, the introduction of patient education aimed at improving chronic pain and psychological factors as part of rehabilitation may be effective for the reduction of pain and psychological factors such as depression and anxiety, and may prevent the decrease of activity and the decrease of HRQOL. However, there have been no reports that have examined the effects and trends of rehabilitation incorporating patient education for knee osteoarthritis on psychological factors such as pain, depression, and fear of falling, as well as HRQOL. Furthermore, there have been no reports examining the time course of HRQOL in patients with knee osteoarthritis using patient education and rehabilitation intervention based on behavior change.
The purpose of this study was to examine the effect of combined patient education and conservative rehabilitation on pain, psychological factors, and change of HRQOL in patients with knee osteoarthritis.
METHODS
Subjects
The object patients were 30 patients over 65 years old who were diagnosed as osteoarthritis of the knee and underwent conservative treatment and rehabilitation from May 2020 to March 2022. Conservative treatment refers to the use of external preparations, oral medications, braces, or intra-articular injections according to symptoms. Surgical treatments were excluded. Patients were also included if they had other motor disorders and were diagnosed with knee pain and osteoarthritis on radiography.
This study was a pilot study with 30 subjects. We prospectively investigated the change over time in patient education effect in the osteoarthritis conservative treatment example.
In consideration of ethical issues, after sufficient informed consent to participate in the study, the subject’s voluntary consent form was obtained. This study was approved by the Institutional Review Board of the Nihon University Hospital (IRB No. 20200403), and informed consent was obtained from each patient.
Methods
Method of patient education
The behavior change program using the pamphlet as educational tool was carried out.
The contents of patient guidance included questionnaires, individual guidance using educational tools, and goal setting. Present a questionnaire to help you discover what you want to ask. In addition, information on items related to health status and HRQOL was extracted. In the individual guidance using the education tool, the pamphlet which described the gist of the content in the patient education was used. The pamphlet in which the description on the gonarthrosis which Japanese Orthopaedic Association (JOA) announced was described was used for the method of the patient education [8]. The pamphlets describe the causes of knee osteoarthritis, the characteristics of the symptoms, the classification of the degree of progression on X-ray, and the treatment. The symptoms described include pain in the knees and difficulty walking up and down stairs, difficulty squatting or sitting upright, and stiff knees when standing up. Causes and characteristics: The causes of knee osteoarthritis can be either primary, for which the cause cannot be clearly determined, or secondary, for which an injury or disease around the knee joint affects.
Previous injuries, such as meniscus and ligament injuries, sprains and fractures, and diseases such as rheumatoid arthritis and pseudogout are classified as secondary, but most cases are primary knee osteoarthritis for which the cause cannot be determined. It is explained that the grade in the X-ray is classified from 1 to 4 according to the size of the gap of the joint. For treatment, conservative treatment such as injection and internal use, rehabilitation, and operative treatment are explained.
On the basis of this pamphlet, the knowledge on purpose, on the disease state, the guidance was carried out on prevention method, range of motion training and muscle strengthening practice, walking practice, activity of daily living practice and home exercise program according to the individual condition. The home program included a stepwise walking program, range of motion training for bathing, and locomo training was performed at home three times a day. Locomo training consists of standing on each leg for 1 minute and squatting 5 to 6 times [9]. Patient education was provided at the start of rehabilitation, 1 month after the start of rehabilitation, and at the end of rehabilitation intervention.
Practice of behavior change programs
The behavior change program was based on the health belief model by Sedlak et al. [10]. It consists of the following; I. motivate, II. persuade verbally, and III. elicit physiologically and emotionally.
I. Motivate
The risk caused by osteoarthritis of the knee is explained. The risks of pain, restricted walking, and decreased ability to live were discussed in the pamphlet published by the JOA.
II. Persuade verbally
Goal level decisions were verbal persuasion based on achievement. Exercise therapy consisted of one-to-one gait correction, muscular strength and endurance training, and range of motion training, depending on the individual’s level.
III. Elicit physiologically and emotionally
Attention should be paid to improvements in knee function and pain as a result of exercise therapy.
As a method to confirm whether the patient understood the contents of the instruction, the degree of understanding was confirmed by interviewing the patient to confirm whether the patient understood the contents of the instruction and having the patient explain it verbally at the time of patient follow-up. The period of instruction was 5 months.
Rehabilitation methods
The physical therapist intervened in the rehabilitation. The rehabilitation menu included range-of-motion exercises, muscle strengthening exercises mainly for the quadriceps femoris, gait training, and balance training [11]. For patients with knee pain, we administered drugs and intra ‐ articular injection of hyaluronic acid to control pain and implemented an education program. The frequency of rehabilitation was once every 2 weeks for 40 minutes. For patients with knee pain, we administered drugs and intra‐articular injection of hyaluronic acid to control pain and implemented an education program. The rehabilitation period was 5 months.
Evaluation of measurement index
Evaluations were performed at three time points: before exercise therapy intervention,
1 month into intervention, at the end of the intervention. The items investigated were as follows: (1) knee osteoarthritis severity, (2) knee osteoarthritis staging, (3) fear of falling, (4) instrumental ADL, (5) degree of depression, and (6) HRQOL. Fear of falling, instrumental ADL, degree of depression, and HRQOL were determined using a self-administered questionnaire directly to subjects, which they returned completed following their medical examination.
The degree of progression of knee osteoarthritis was classified using the Kellgren-Lawrence (K-L) grading system [12]. The K-L system consists of five grades from 0–4: 0 is no osteoarthritis; 1 is doubtful narrowing of the joint space and/or possible osteophytes; 2 is definite osteophytes and possible narrowing of the joint space; 3 is multiple osteophytes, definite narrowing of the joint space, and some sclerosis and deformity of the bone ends; and 4 is large osteophytes, marked narrowing of the joint space, severe sclerosis, and definite deformity of bone ends. Also, knee osteoarthritis severity, Fear of falling, Instrumental ADL, Degree of depression, and HRQOL were assessed at the beginning and end of rehabilitation.
(1) Knee osteoarthritis severity
Knee osteoarthritis severity was measured using the patient’s JOA score [13]. It is a measure to evaluate the degree of functional impairment. Rate pain, walking ability, stair climbing, flexion angle, and swelling on a scale of 1 to 100. The higher the score, the higher the knee joint function.
(2) Fear of falling
Fear of falling was evaluated using the Fall Efficacy Scale (FES) was advocated for Tinetti et al. [14]. The FES is a tool that measures the degree of confidence of a person to perform 10 different ADL without falling on a four-point scale. Scores are expressed from 10 to 40 points, and a lower score indicates less fear of falling.
(3) Instrumental ADL
Instrumental ADL was evaluated using the Frenchay Activities Index (FAI) developed by Holbrook and Skilbeck [15]. It was evaluated 15 applied ADL and social life items on a four-point scale from 0–3 points. The maximum score is 45 points, and a higher score indicates greater instrumental ADL ability and independent applied ADL.
(4) Degree of depression
Degree of depression was evaluated using the Geriatric Depression Scale (GDS). The GDS was developed to measure depression, and a higher score means a higher degree of depression [16-18].
(5) HRQOL
The evaluation of HRQOL used Short Form-8 (SF-8) which was short version of Short-Form Health Survey (SF-36) [19]. SF-8 can be evaluated efficiently with a minimum number of items, and consists of the following eight items (subscales): general health (GH), physical functioning (PF), role physical (RP), bodily pain (BP), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). A higher score indicates higher QOL. Physical component summary (PCS) and mental component summary (MCS) scores are also calculated using regression equations based on the weighting of each item. Use of the SF-8 in this study was registered with the Institute for Health Outcomes & Process Evaluation Research to obtain a license. For fear of falling, instrumental ADL, depression, and HRQOL, questionnaires were given to the patients at the beginning and one month after the rehabilitation intervention and at the end of the intervention, and the questionnaires were collected after the patients answered the questionnaire contents. Correlations and associations were statistically verified for each score.
Statistical analysis
The controlled analysis included outcomes of PCS and MCS, HRQOL scores, and tested for influencing factors. For the validation method, the dependent variables were PCS and MCS, and the independent variables were age, sex, FES, FAI, and GDS, with a significance probability of 0.05%. In addition, factors correlated with PCS and MCS scores were verified by correlation coefficients. The statistical analyses were performed using IBM SPSS Statistics version 23 (IBM Corp.). Normally distributed variables were expressed as the mean±standard deviation and variables with a skewed distribution as the median and interquartile range. The chi-square test, unpaired t-test, Mann–Whitney U-test, χ2 test, and the Fisher exact test were used, as appropriate, to compare variables between the groups.
RESULTS
The baseline characteristics of the subjects are presented in Table 1.
Changes in JOA score are shown in Fig. 1. The JOA score was significantly improved 1 month after the patient education intervention compared to before the intervention (p<0.01). There was no significant difference in the presence or absence of painkillers or intra-articular injections in each period. Results of PCS and MCS scores for SF-8 items are shown (Fig. 2). MCS score ranged from 47.9 before the intervention to 48.6 at the end of the intervention. The PCS score ranged from 40.8 before the intervention to 48.4 at the end of the intervention. PCS score was significantly improved 1 month after the patient education intervention compared to the start (p<0.01). There were no significant differences in MCS scores between the time periods.
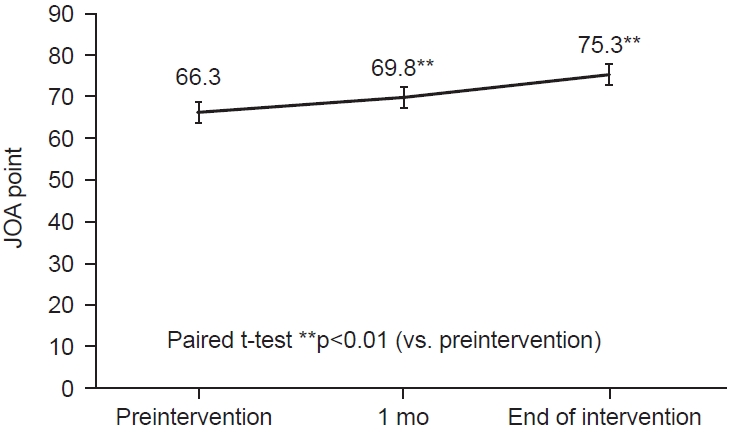
Change in average Japanese Orthopaedic Association (JOA) score. JOA scores at 1 month after the intervention and at the end of the intervention were significantly improved from those at the beginning of the intervention (**p<0.01). Knee joint function was significantly improved.
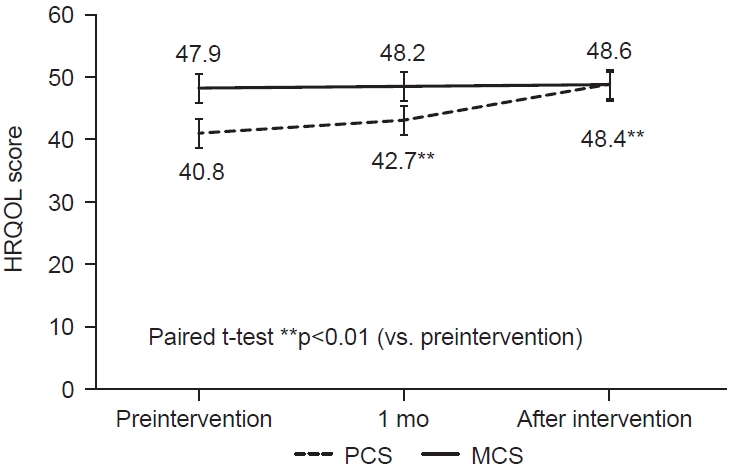
Change in average health-related quality of life (HRQOL) score. The physical component summary improved significantly with rehabilitation and patient education (**p<0.01), but the mental component summary showed no apparent improvement. PCS, physical component summary; MCS, mental component summary.
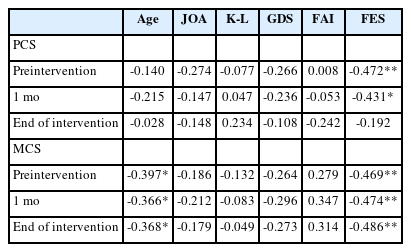
Changes in FES and FAI are shown in Figs. 3, 4. At the end of the patient education intervention, it was significantly lower than at the start (p<0.01). GDS score is shown in Fig. 5. GDS score was significantly improved 1 month after the patient education intervention compared to the start (p<0.01). Table 2 shows the correlation between PCS score, MCS score, and measurement items at each time period. PCS score was negatively correlated with FES before and 1 month after the patient education intervention (p<0.01, p<0.05). MCS score was negatively correlated with Age and FES (p<0.05, p<0.01).
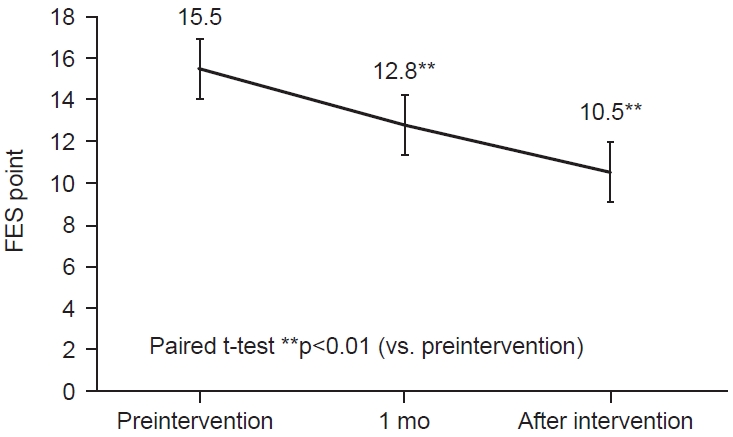
Change in average Fall Efficacy Scale (FES). The FES was significantly improved 1 month after the intervention by the intervention of rehabilitation and patient education (**p<0.01).
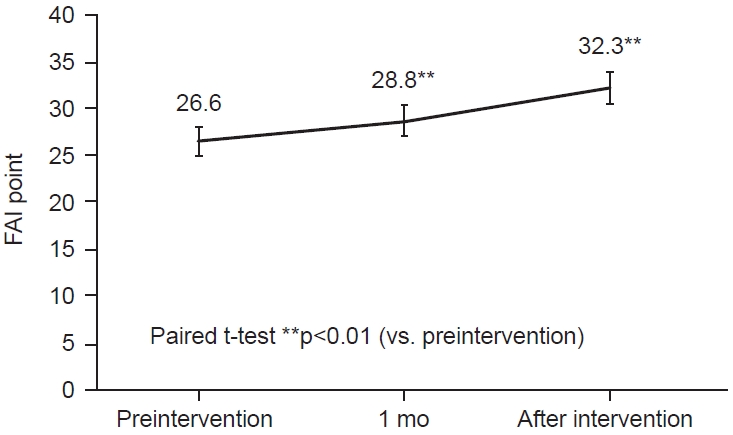
Change in average Frenchay Activities Index (FAI). The FAI was significantly improved 1 month after the intervention by the intervention of rehabilitation and patient education (**p<0.01).
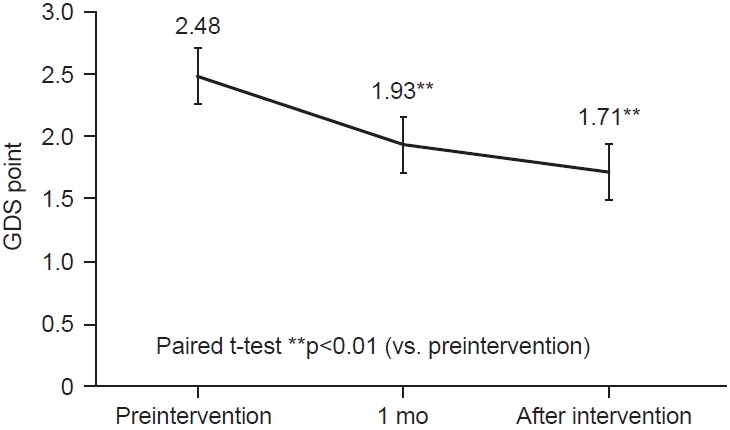
Change in average Geriatric Depression Scale (GDS). The GDS was significantly improved 1 month after the intervention by the intervention of rehabilitation and patient education (**p<0.01).
Results of multiple regression analysis with PCS and MCS scores at final follow-up as dependent variables and age, sex, FES, FAI and GDS as independent variables are shown in Table 3. Sex was extracted as an influencing factor for PCS scores (p<0.01). FES was also extracted as an influencing factor of MCS score (p=0.046).
DISCUSSION
A prospective cohort study of patient education interventions for osteoarthritis of the knee shows two major finds. First, the patient education intervention improved PCS score but not MCS score. Second, age was found to be an influencing factor for PCS score, and fair of falling was found to be an influencing factor for MCS score.
Muraki et al. [20] describes HRQOL in knee osteoarthritis, revealed that in severe cases, the PCS score decreases and correlated with pain. The PCS score also correlated with pain and grip strength. On the other hand, the MCS is not related to the severity of knee osteoarthritis, and a variety of factors were involved. In our previous studies have examined changes in HRQOL when knee osteoarthritis is treated with rehabilitation without patient education. As a result, JOA scores, fear of falling, and instrumental ADL improved significantly from the start of rehabilitation to three months after the intervention. However, depression and mental and PCS score did not significantly improve. In the current study with patient education, depression and PCS score were significantly better than before patient education, indicating that patient education may be effective for depression and physical HRQOL. To improve MCS, it is necessary to review the contents of the current education program and verify the education program for cases with severe psychosomatic elements.
The association between MCS and PCS scores tended to correlate with fear of falling, indicating that taking a fall prevention approach may improve HRQOL.
Second, age was found to be an influencing factor for PCS score, and fear of falling was extracted as a factor influencing MCS score at the end of patient education. FES showed a negative correlation with MCS score. The results suggest that fear of falling affects MCS more than PCS score. Therefore, educational guidance and functional training to reduce fear of falling were considered necessary to improve MCS score.
For fear of falling and HRQOL, Stanghelle et al. [21] examined whether balance training in vertebral fractures affects fear of falling and HRQOL. Balance training reduced the fear of falling and showed improvements in muscle strength and balance ability. However, they noted that balance training did not improve HRQOL. We have verified and reported the transition of HRQOL in osteoarthritis of the knee by rehabilitation intervention [5]. As with the results of Stanghelle et al. [21], there was no improvement in HRQOL with the exercise intervention, but there was a significant improvement in fear of falling.
In this study, we investigated the effects of a rehabilitation intervention incorporating patient education on HRQOL, psychological factors and motor function in patients with knee osteoarthritis. As a result, improvements in PCS score were observed in osteoarthritis of the knee by the patient education program. The patient program we implemented introduced the behavior change program proposed by Sedlak et al. [10]. As to reasons for the lack of improvement in MCS score, it is possible that the behavior change program proposed by Sedlak et al. [10] consisted of I. motivate, II. persuade verbally, and III. elicit physiologically and emotionally, which had an improving effect on the physical approach but not enough intervention on the psychological approach. It is necessary to strengthen the approach to mental health, role emotional and social functioning which are the items of MCS score.
Fear of falling was also identified as an influencing factor of HRQOL in the multivariate analysis. The reason for this was thought to be that when the fear of falling is high, the mental health may be affected by the decreased opportunity to go out and the decreased social function caused by the fear of falling. It is possible that rehabilitation approaches that reduce the fear of falling, such as strengthening gait stability, trunk balance, and lower limb muscle strength, may be effective in improving HRQOL. Regarding the relationship between fear of falling and HRQOL, Stanghelle et al. [21] examined the effects of a resistance and balance exercise program on physical fitness, HRQOL and fear of falling in osteoporotic vertebral compression fractures. The results showed that there was no significant improvement in HRQOL, although there were two weeks of a supervised multicomponent resistance and balance exercise program improved muscle strength and balance and reduced fear of falling. Our validation with the exercise therapy intervention also showed no improvement in HRQOL. Exercise therapy interventions for motor disorders, which are common among the elderly, did not improve HRQOL, and an approach to life anxiety associated with old age, such as senile depression and fear of falling, is necessary to improve HRQOL. Taglietti et al. [22] also reported on the association between knee osteoarthritis and fearing of falling, stating that sensory instability is related to fearing of falling in knee osteoarthritis. In order to improve the fearing of falling in knee osteoarthritis, it is necessary to enhance trunk stability. Simsek et al. [23] also reported that fear of falling is higher among older females over 80, especially if they live alone. In order to reduce the fear of falling in the elderly, not only an exercise therapy approach, but also the enhancement of social support and support for the elderly living alone would lead to a decrease in the fear of falling and further improve HRQOL.
In our study, we introduced risk guidance for knee pain and an approach to anxiety, self-directed training guidance, and a patient education program for osteoarthritis of the knee, and examined the effects of improving HRQOL. They found improvement in PCS score, but not in MCS score. No research has examined the transition of HRQOL due to the introduction of a patient education program in patients with knee osteoarthritis, and it is necessary to improve and verify the education program considering the MCS score items of mental health, role emotional and social functioning. In addition, considering the social background, it is expected that in elderly people living alone, not only the approach of an exercise therapy but also the support for the enhancement of social support will reduce the fair of falling and lead to the improvement of HRQOL.
Furthermore, multivariate analysis extracted sex as an influential factor in PCS score. This may be because osteoarthritis of the knee is reported to be more likely to be severe in postmenopausal females [24], and as a result, sex may have been extracted as an influential factor in PCS score.
One of the limitations of this study is that, first, because of the exploratory study, we were able to verify changes and transitions over time in the same subjects through the intervention of the patient education program, but the validation of the effectiveness of the validation patient education program was insufficient. Since this study is a single arm design study, it is considered to be a limitation that it cannot be compared with a control group. It is considered that the verification g compared with the control group is necessary in future. Second, there was insufficient verification of the relationship between the patients’ backgrounds, such as the presence or absence of mental illness, the presence or absence of a history of psychiatric visits, and the use of psychotropic drugs. It is necessary to examine the influence of psychiatric disorders on knee osteoarthritis in the future.
As a result of patient education that included motivate, persuade verbally, elicit physiologically and emotionally as a behavior change program, PCS score of HRQOL items improved, but MCS score did not. In the following, it is necessary to verify patient education programs focusing on mental health, role emotional and social functioning as a treatment approach to improve HRQOL of knee osteoarthritis. The results also indicate that an educational approach to fear of falling may improve anxiety and that functional training may be effective in improving HRQOL in knee osteoarthritis.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING INFORMATION
None.
AUTHOR CONTRIBUTION
Conceptualization: Nagai T. Methodology: Nagai T, Uei H. Formal analysis: Nagai T, Uei H. Project administration: Nagai T, Nakanishi K. Visualization: Nagai T, Uei H. Writing – original draft: Nagai T, Uei H. Writing – review and editing: Nagai T, Nakanishi K. Approval of final manuscript: all authors.
Acknowledgements
The authors sincerely thank their study subjects and also gratefully acknowledge the Nihon University Hospital. I would also like to thank H.Wakabayashi for his advice. Finally, we are grateful to the referees for useful comments.