- Search
| Ann Rehabil Med > Volume 48(2); 2024 > Article |
|
Abstract
Objective
To explore the relationship between pulmonary function, physical activity, and health-related quality of life (QoL) in resected lung cancer patients based on the International Classification of Functioning, Disability, and Health (ICF) framework developed by the World Health Organization to describe health and health-related states.
Methods
A quantitative study was designed with postoperative lung cancer survivors to assess personal characteristics. We also assessed functional impairment related to the lung using forced vital capacity (FVC) and forced expiratory volume at 1 second (FEV1), activity limitations using maximal oxygen consumption (VO2max), anaerobic threshold (AT) and 6-minute walking distance (6MWD), and participation restriction using the 36-item Short Form Health Survey V1 (SF-36). Data analyses were conducted using the multivariate method and SmartPLS to examine path coefficient among the measures.
Results
Forty-one patients were enrolled in this study. FVC and FEV1 were poorly correlated with QoL, and 6MWD, AT, or VO2max were positively associated with QoL. AT or VO2max showed a significant (p<0.01) direct path with SF-36 in the ICF model. Although age and body mass index were not strongly correlated with QoL, these personal factors had a medium to large effect on perceived QoL.
Conclusion
Disability is a complex in patients with lung resection, and physical activity plays an important role in enabling participation. Improving VO2max and AT is needed to improve the QoL of resected lung cancer patients. We should also pay more attention to contextual factors that have a significant impact on social participation.
Much progress has been made in the diagnosis and treatment of non-small cell lung cancer in recent years, and prognosis has gradually improved correspondingly. For a significant number of patients, surgical resection is the preferred treatment. While the survival rate after an operation is not satisfactory, more and more patients want to obtain prolonged postoperative survival [1] and a better quality of life (QoL) [2]. Therefore, exploring the factors that affect QoL in these patients is of great importance.
Lung resection has a significant short- and long-term impact on pulmonary function and oxygenation [3], and physical activity, measured by 6-minute walking distance (6MWD), has also been reported to decline after surgery [4]. And many symptoms, including dyspnea, emotions, pain, and side effects of treatment, may occur after lung resection. Lung resection is so invasive that it lowers QoL, especially in the early stages of surgical treatment [5]. Improving the QoL after surgery is one of the main goals of comprehensive treatment. Interestingly, many evidences showed that many aspects are involved to the QoL in various types of diseases. For instance, the previous study showed that peak oxygen uptake, 6MWD, and anxiety remained independent factors for QoL in patients with pulmonary arterial hypertension [6]. Engberg et al. [7] found that cardiorespiratory fitness (CRF) was positively associated with health-related QoL in females at risk for gestational diabetes. And Ha et al. [8] reported that exercise capacity was independently associated with QoL for lung cancer patients after postcurative intent treatment. Unfortunately, although a poor correlation between QoL and forced expiratory volume at 1 second (FEV1) has been explored by Brunelli et al. [9], a limited number of studies have examined whether direct or indirect effects of pulmonary function and physical activity on QoL in patients after lung resection.
Because great number of factors affect patient’s health comprehensively including structural impairments, functional limitations, participation restrictions and contextual factors, it is crucial to identify risk factors that may deteriorate a patient’s health status. The World Health Organization’s International Classification of Functioning, Disability and Health (WHO ICF) model provides a coherent view of different aspects of health from biological, individual and social perspectives [10], as shown in Fig. 1. As an analysis framework, the interplay between these factors in the ICF model is important for characterizing the disability and providing rehabilitation [11]. To our knowledge, the association between patients’ physical activities and QoL according to the ICF model has not been studied.
Various factors influence QoL in patients with lung cancer, including malnutrition [12], social support [13], psychosocial factors [14], and physical activity [15]. Data indicate that lung cancer patients experience compromised QoL. Therefore, understanding the factors that determine QoL for patients after lung resection is crucial in enhancing prevention programs and treatment strategies. In this study, we propose an ICF-based model, illustrated in Fig. 2, to explore the associations between pulmonary function, physical activity, personal factors, and QoL using the ICF model and to assess their impact on QoL of patients after lung resection.
Ethical approval has been obtained from the Ethical Committee of Guangdong Provincial People’s Hospital (2012124H(R2)). The clinical trial had been registered in the Chinese Clinical Trials Registry (ChiCTR-TRC-13003400). This study was conducted in accordance with the declaration of Helsinki ethical principles for human experimentation and all patients gave their informed consent to participate in the study.
A quantitative study was designed and Fig. 3 presents the flowchart of the study. Patients who underwent lobectomy were recruited according to criteria for non-small cell lung cancer staged T1, T2, and T3a without chronic obstructive pulmonary disease. Exclusion factors included: Stage T3b and T4 non-small cell lung cancer, patients with serious chronic diseases (i.e., coronary artery disease, heart failure, atrial fibrillation, hypertension, osteoporosis, infections), refused to participate in this study. Each patient had a routine full clinical assessment prior to inclusion, and all patients included in this study provided written informed consent before data collection.
Data including age, sex, and body mass index (BMI) were recorded, and assessments including forced vital capacity (FVC), FEV1, 6MWD, anaerobic threshold (AT), maximal oxygen consumption (VO2max), and the 36-item Short Form Health Survey V1 (SF-36) were performed one month after lung resection. Data were collected from January 2014 to December 2017. The same therapists conducted all evaluations throughout duration of the study. Data collection and analysis were not carried out by the same persons who completed the assessment.
According to the results of preliminary experiment, with power of 0.9, alpha of 0.05, ρ0=0, and ρ=0.5. Sample size was calculated using a formula for correlation study with PASS20.0 software (NCSS, LLC), and the total sample size is 37. To compensate non-compliance among subjects, the sample size was increased (+10%) to 41 patients.
Pulmonary volumes including FVC and FEV1 were measured using a spirometer (Electgraph HI-101; CHEST), and corrected for temperature and barometric pressure, according to the American Thoracic Society recommendations [16]. Each patient performed at least three trials and the best results were used for analysis.
Physical activity was determined by 6MWD [17]. 6MWD was carried out under the same conditions. Patients were instructed to walk at their fastest pace to cover the longest possible distance over 6 minutes. The longest walk was taken to represent the value.
Before the cardiopulmonary exercise test, a physician examined the patients beforehand to ensure their suitability for the test. We assessed CRF by VO2max and AT in incremental (30 W/3 min) cycle ergometer exercise (METAMAX 3B; CORTEX) until patient fatigue or dyspnea by pointing to a score on Borg scale category ratio 10. VO2max was determined as the highest 1-minute average value and was normalized for body mass (mL/kg/min).
Health-related QoL was evaluated with SF-36 [18]. The survey is a valid and reliable 36-item questionnaire that is widely used to measure QoL. It yields two summary scores of physical (physical functioning, role-physical, bodily pain, and general health) and mental (vitality, social functioning, mental health, and role-emotional) health. Scales range from 0 to 100, with 0 indicating the worst situation and 100 indicating the best situation in each domain.
Data were expressed through descriptive and inferential statistical analysis. Firstly, we examined whether the variables were normally distributed with the Anderson-darling test, then we used Spearman’s correlation coefficients for non-normally distributed variables. For normally distributed variables, we used Pearson’s correlation coefficients. The dependent variables were SF-36 total score, and the independent variables were FEV1, FVC, 6MWD, VO2max, AT, and personal factors including age, sex, and BMI. The Statistical Package for Social Sciences (IBM SPSS 20.0; IBM Corp.) was used. Secondly, a structural model was estimated and structural equation modeling was used to examine the path coefficient between the measures, and the proposed hypotheses were confirmed. To test the proposed model, we adopt partial least squares structural equation modeling (PLS-SEM) using SmartPLS software (version 4) due to the small sample size. And the sample size of the PLS-SEM was determined in accordance with the principle that the sample size should be a minimum of 10 times the greater of: (1) the largest number of formative indicators employed to measure a single construct, or (2) the largest number of structural paths directed towards a specific construct within the structural model [19]. In our study, the largest number of structural paths directed towards a specific construct within the structural model were three, and the total sample size was at least 30. Hence, the designated sample size in this study was 41 which was sufficient to perform the PLS-SEM. When performing the confirmatory factor analysis, we ensured the original model of four factors and 8 items with factor loadings above 0.50, the composite reliability (CR) and convergent validity (average variance extracted, AVE) ranged from 0.6 to 1.00 and higher than 0.5, respectively [20]. In our study, we interrogated the robustness of the model using blindfolding to obtain cross-validated redundancy measures for each construct and using the bootstrapping procedure with 5,000 re-samples to determine the significance level of weights, factor loadings, and path coefficients [20]. A p-value of <0.05 was considered statistically significant.
Forty-one patients were enrolled in this study and the complete data were included in the analysis. Among these participants, the TNM classification of lung cancers was as follows: 26 stages 1, 11 stages 2, and 4 stages 3a. The types of lung cancer cells were as follows: 25 adenocarcinomas, 13 squamous carcinomas, and 3 others. The median age was 62 years (61.73±10.89 years), and 51.20% (21 out of 41) were male. The median BMI was 22. Table 1 summarized the characteristics, QoL, FVC, FEV1, 6MWD, AT, and VO2max of the patients.
In the study, the values of sex, BMI, 6MWD, VO2max, and SF-36 had normal distribution. In relation to the SF-36 total score, Table 2 showed a significant linear correlation was detected between 6MWD (r=0.317, p=0.044), AT (r=0.442, p=0.004), and VO2max (r=0.344, p=0.028). SF-36 total score was poorly correlated with FVC (r=0.144, p=0.370), FEV1 (r=0.251, p=0.114), BMI (r=0.187, p=0.242), age (r=0.216, p=0.176), and sex (r=-0.054, p=0.739).
A reflective modeling approach was employed to test the hypotheses. CR and the AVE were used to assess the convergence of observed variables. As shown in Fig. 4, all items exceeded the 0.62 loading threshold, with CR ranging from 0.6 to 1.0 and higher than 0.5 with AVE. To establish discriminant validity, we selected the heterotrait-monotrait ratio, with all values in this study below 0.597 (Table 3), meeting the recommended cut-off of 0.85 [20]. In addition, collinearity was examined to ensure unbiased regression results, and the variance inflation factors (VIFs) for inner model paths were evaluated. The results revealed that VIF values ranged from 1.0 to 1.15, well below the recommended threshold of 5. With respect to model fit, the standardized root mean residual and normed fit index had values of 0.057 and 0.933, respectively, which were both within the recommended range. These data indicated that the constructs met the required standards for the present study, allowing us to adequately test the research hypotheses (Table 3).
As shown in Table 4, the path linking personal factors and physical activities to perceived SF-36 was positive and statistically significant, and the path linking FVC, and FEV1 to SF-36 was not positive and statistically insignificant. The R2 value for SF-36 is 0.360 which means that 36.0% of the changes in QoL were due to pulmonary function, physical activity, and personal factors in the model (Fig. 4). In general, the effect of a latent predictor variable is small at the structural level if f2 is 0.02, medium if f2 is 0.15, and large if f2 is 0.35 [20]. We found that physical activity (f2=0.292) and personal factors (f2=0.197) had medium to large effect sizes on perceived QoL, while pulmonary function had no effect sizes on perceived QoL in patients with lung resection (Table 5).
This study examined the relationship between FEV1, FVC, 6MWD, personal factors, and health-related QoL in patients with lung resection. Our results showed that FVC and FEV1 were poorly correlated with QoL, and 6MWD, AT, or VO2max were positively associated with QoL. Our findings also showed that pulmonary function, physical activity, age, and BMI took charge of 36.0% of changes in perceived QoL in the ICF model. Although age and BMI were not strongly correlated with QoL, the personal factors had a medium to large effect on perceived QoL.
Many pieces of evidence showed that lung resection had a significant impact on respiratory function, and the deficits may reduce the patients’ QoL [3,5]. However, Brunelli et al. [9] found that QoL had a poor correlation with FEV1 and carbon monoxide lung diffusion capacity. In this study, we also showed that FVC and FEV1 were not related to QoL. These results indicated that FVC and FEV1 affected only a few functioning scales and could not be taken as surrogate for QOL evaluation [9]. Because few direct effects of FVC and FEV1 on QoL were observed in our study, pulmonary function-enhancing intervention may play a limited role in improving QoL in resected lung cancer patients.
Lung cancer survivors always experience QoL impairments, and engagement in physical activity is associated with better QoL. Also, physical activity was independently associated with QoL in lung cancer patients with postcurative-intent treatment [8]. We also found that 6MWD was associated with QoL, but the significance level was p=0.045. However, 6MWD recovery in elderly patients after lung cancer surgery was not related to their health-related QOL recoveries [4]. One possible reason for inconsistent results is that the effect of 6MWD on QoL is indirect. CRF is primarily determined by aerobic physical activity, and is strongly associated with the physical dimensions of health-related QoL. In our study, CRF (6MWD, AT, and VO2max) was positively associated with QoL, and AT or VO2max were also highlighted as predictors. The results indicated that physical activity had a significant impact on improving QoL in patients with lung resection.
In the clinic, QoL in resected lung cancer patients was poor. Poor QoL means difficulty for these types of patients dealing with a range of deficits or limitations related to cognitive, psychosocial, physical, sensory functioning, and other aspects of performance [21]. From a statistical point of view, in relation to the disability process, contextual factors can act as independent factors, confounding factors, moderating factors, and mediating factors [22]. We found that personal factors (age and BMI) had a direct effect on QoL in this study. Noting that only 36.0% of perceived QoL changes were associated with pulmonary function, physical activity, age, and BMI. Thus, the improving QoL program for lung resection patients focuses not only on how to improve physical activity, but also on other impact factors such as environmental factors and personal factors.
With regard to the limitations of this study, it was a single-center study. Meanwhile, some other factors that could affect QoL in resected lung cancer patients were not included in our structural equation modeling, such as family support, economic level, and environmental impact. In the future, large-scale observational studies involving sufficient patients and effect factors are needed.
In conclusion, disability is a complex in patients with lung resection and encompasses a prominent role of physical activity in predicting participation. Improving VO2max is needed to improve the QoL of resected lung cancer patients. We should also pay more attention to contextual factors that have a significant impact on social participation.
FUNDING INFORMATION
This work was supported by National Natural Science Foundation of China (No. 81972142) and Guangdong Medical Science and Technology Research Foundation (No. A2022512).
AUTHOR CONTRIBUTION
Conceptualization: Li X, Zhang M. Methodology: Chen Y, Liu S. Formal analysis: Li X, Chen Y, Liu S. Funding acquisition: Li X. Project administration: Li X, Zhang M. Supervision: Zhang M. Writing – original draft: Li X. Writing – review and editing: Li X, Zhang M. Approval of final manuscript: all authors.
Fig. 1.
International Classification of Functioning, Disability and Health categorization of outcome measures used in this study.
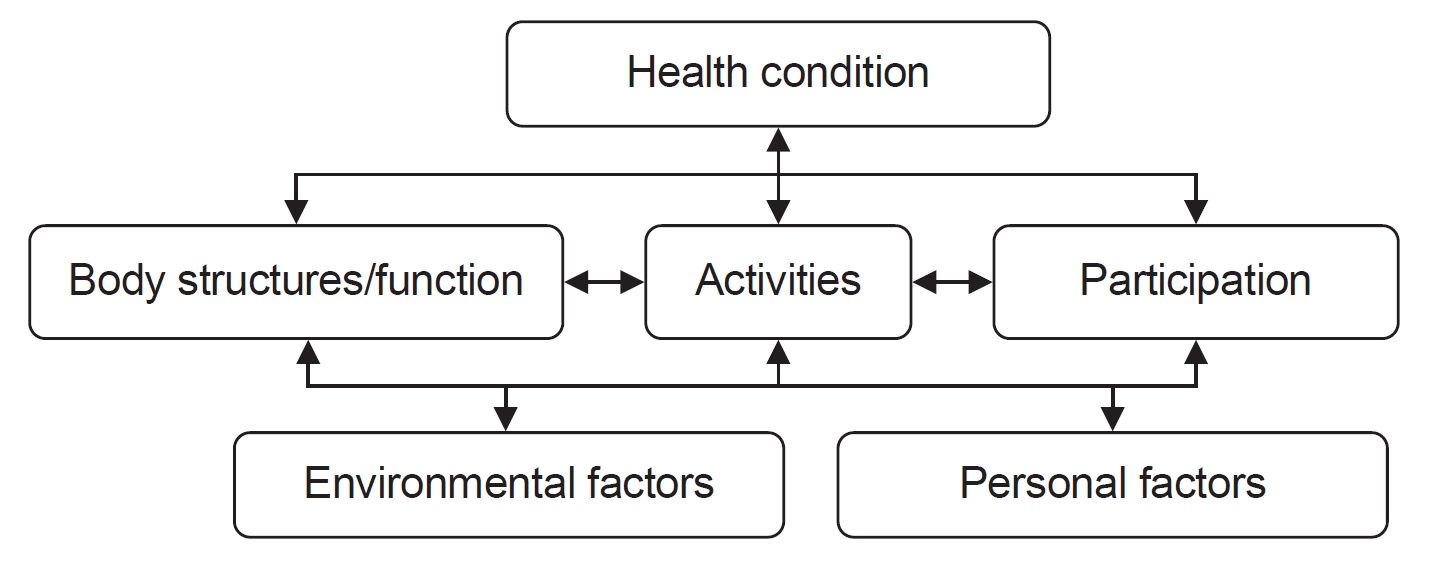
Fig. 2.
The hypothetical model based on International Classification of Functioning, Disability and Health framework. FVC, forced vital capacity; FEV1, forced expiratory volume at 1 second; 6MWD, 6-minute walking distance; AT, anaerobic threshold; VO2max, maximal oxygen consumption; SF-36, the 36-item Short Form Health Survey V1; BMI, body mass index.
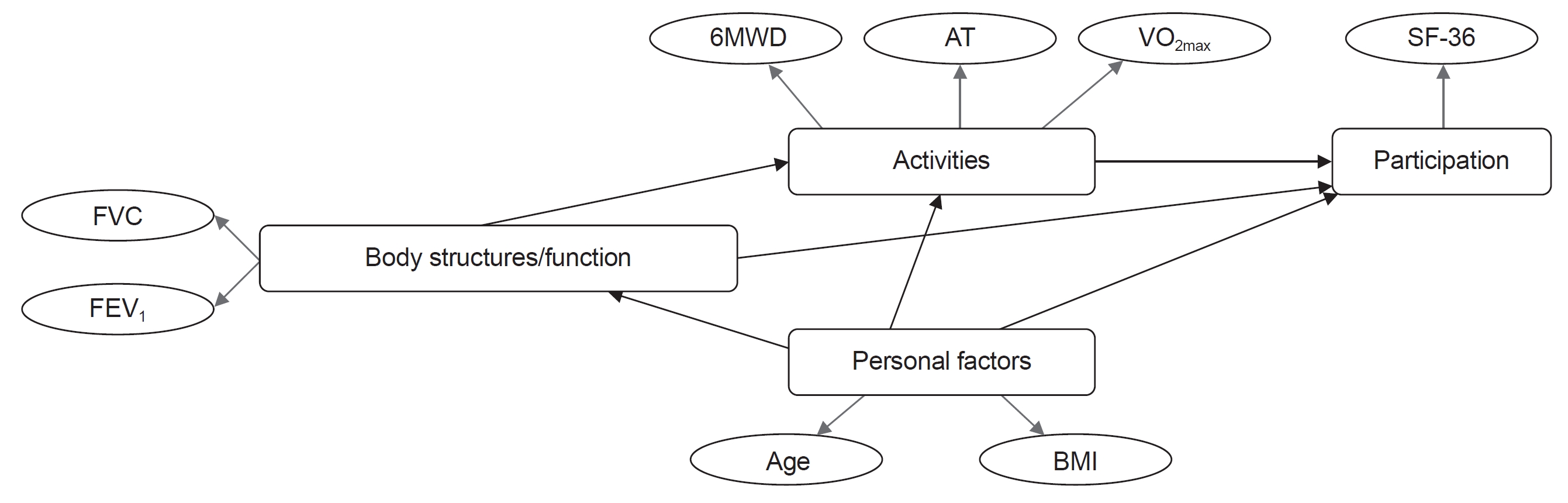
Fig. 3.
The summary of workflow in this study. SF-36, the 36-item Short Form Health Survey V1; PLS-SEM, partial least squares structural equation modeling.

Fig. 4.
Structural equation model exploring the basic paths of the International Classification of Functioning, Disability and Health model for patients with lung resection. FVC, forced vital capacity; FEV1, forced expiratory volume at 1 second; 6MWD, 6-minute walking distance; AT, anaerobic threshold; VO2max, maximal oxygen consumption; SF-36, the 36-item Short Form Health Survey V1; BMI, body mass index.
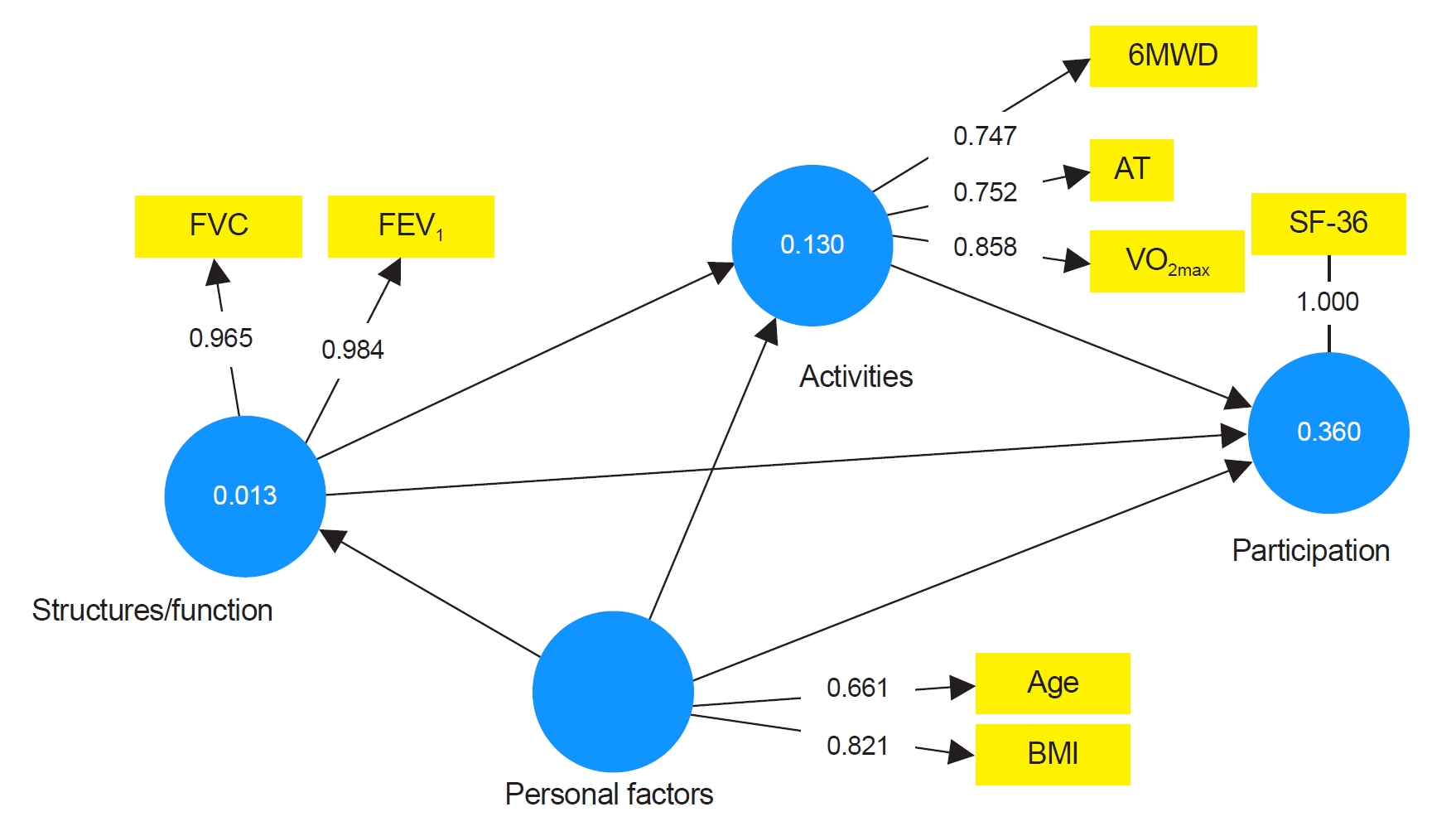
Table 1.
The patients’ clinical characteristics and functional variables in patients with lung cancer resection
Table 2.
Correlation coefficients of sex, BMI, age, FEV1, FVC, AT, VO2max, and 6MWD with health-related quality of life (SF-36)
Table 3.
Convergent validity, discriminant validity, and collinearity statistics
Table 4.
Summary of estimates for hypothesized structural model
Table 5.
Results of effect size f2 analysis
REFERENCES
2. Chen HL, Liu K, You QS. Self-efficacy, cancer-related fatigue, and quality of life in patients with resected lung cancer. Eur J Cancer Care (Engl) 2018;27:e12934.



3. Brocki BC, Westerdahl E, Langer D, Souza DSR, Andreasen JJ. Decrease in pulmonary function and oxygenation after lung resection. ERJ Open Res 2018;4:00055-2017.



4. Saito H, Shiraishi A, Nomori H, Matsui H, Yoshida K, Matsue Y, et al. Impact of age on the recovery of six-minute walking distance after lung cancer surgery: a retrospective cohort study. Gen Thorac Cardiovasc Surg 2020;68:150-7.



5. Szeliga E, Czenczek-Lewandowska E, Kontek A, Wolan-Nieroda A, Guzik A, Walicka-Cupryś K. Evaluation of the quality of life after surgical removal of lung cancer. Adv Respir Med 2019;87:14-9.


6. Halank M, Einsle F, Lehman S, Bremer H, Ewert R, Wilkens H, et al. Exercise capacity affects quality of life in patients with pulmonary hypertension. Lung 2013;191:337-43.



7. Engberg E, Tikkanen HO, Koponen A, Hägglund H, Kukkonen-Harjula K, Tiitinen A, et al. Cardiorespiratory fitness and health-related quality of life in women at risk for gestational diabetes. Scand J Med Sci Sports 2018;28:203-11.



8. Ha D, Ries AL, Mazzone PJ, Lippman SM, Fuster MM. Exercise capacity and cancer-specific quality of life following curative intent treatment of stage I-IIIA lung cancer. Support Care Cancer 2018;26:2459-69.




9. Brunelli A, Socci L, Refai M, Salati M, Xiumé F, Sabbatini A. Quality of life before and after major lung resection for lung cancer: a prospective follow-up analysis. Ann Thorac Surg 2007;84:410-6.


10. Leonardi M. Measuring health and disability: supporting policy development. The European MHADIE project. Disabil Rehabil 2010;32 Suppl 1:S1-8.

11. Moulton E, Wilson R, Deluzio K. Movement and mobility: a concept analysis. ANS Adv Nurs Sci 2019;42:E11-23.


12. Polański J, Jankowska-Polańska B, Mazur G. Relationship between nutritional status and quality of life in patients with lung cancer. Cancer Manag Res 2021;13:1407-16.



13. Luszczynska A, Pawlowska I, Cieslak R, Knoll N, Scholz U. Social support and quality of life among lung cancer patients: a systematic review. Psychooncology 2013;22:2160-8.



14. Pearman T. Psychosocial factors in lung cancer: quality of life, economic impact, and survivorship implications. J Psychosoc Oncol 2008;26:69-80.


15. Bade BC, Gan G, Li F, Lu L, Tanoue L, Silvestri GA, et al. Randomized trial of physical activity on quality of life and lung cancer biomarkers in patients with advanced stage lung cancer: a pilot study. BMC Cancer 2021;21:352.




16. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J 2005;26:319-38.


17. Mänttäri A, Suni J, Sievänen H, Husu P, Vähä-Ypyä H, Valkeinen H, et al. Six-minute walk test: a tool for predicting maximal aerobic power (VO2 max) in healthy adults. Clin Physiol Funct Imaging 2018;38:1038-45.

18. Ware JE Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 1998;51:903-12.


19. Hair JF, Ringle CM, Sarstedt M. PLS-SEM: indeed a silver bullet. J Mark Theory Pract 2011;19:139-52.

20. Hair JF, Risher JJ, Sarstedt M, Ringle CM. When to use and how to report the results of PLS-SEM. Eur Bus Rev 2019;31:2-24.

- TOOLS








