- Search
| Ann Rehabil Med > Volume 47(5); 2023 > Article |
|
Abstract
Objective
To translate the 22-item Longer-term Unmet Needs after Stroke (LUNS) questionnaire, validate it in the Korean stroke population, and assess the reliability of face-to-face and telephone surveys.
Methods
Sixty-six adult patients with stroke from Seoul National University Bundang Hospital and Kangwon National University Hospital were involved in the validation. Participants were interviewed twice using the LUNS Korean version: first, a face-to-face survey for validation, and second, a telephone survey for test-retest reliability. Participants completed the Frenchay Activities Index (FAI) and Short Form 12 (SF-12) Mental and Physical Component Summary (MCS and PCS) scores at the first interview. For concurrent validity, the differences in health status (FAI, SF-12 MCS and PCS) between the groups that reported unmet needs and those that did not were analyzed for each item. Cohen’s kappa and percentage of agreement between the first and second administrations were calculated for each item to determine the test-retest reliability.
Results
The average age of the participants was 61.2±12.8 years and 74.2% were male. Fifty-seven patients were involved in the second interview. Depending on the unmet needs, SF-12 MCS, PCS, and FAI were significantly different in 12 of 22 items. In the test-retest reliability test, 12 items had a kappa of 0.6 or higher, and two had a kappa of <0.4.
Stroke is one of the leading causes of disability worldwide, including in Korea, resulting in a significant socioeconomic burden [1,2]. Stroke mortality rates have decreased dramatically with advancements in the emergency medical system and acute care after stroke. However, the stroke incidence rates have decreased less steeply, suggesting that more stroke survivors will live with disabilities [1]. Although early and intensive rehabilitation after stroke is prioritized in many countries [3,4], many stroke survivors eventually experience long-term disabilities, even years after the onset of stroke [5]. A multicenter cohort study in Korea revealed that 38% of stroke survivors had at least one functional dependence, estimated using a functional independence measure 6 months after stroke [6]. During long-term follow-up after stroke in Korea, patients with stroke experience worsening problems in various domains (i.e., communication, cognition, pain, and mood), leading to lower health-related quality of life [7]. Consequently, many patients with stroke have long-term care needs. However, these needs have not been adequately met in several cases. In a recent systematic review of Longer-term Unmet Needs after Stroke (LUNS), approximately 73% of stroke survivors had at least one unmet need [8], which is associated with a low quality of life for stroke survivors or their caregivers [9-11].
Therefore, systematical identification of the current status of unmet needs in various domains using a validated tool is crucial for formulating a policy to adequately and efficiently address unmet needs. A LUNS monitoring tool consists of 22 items for various needs in multiple domains including information, service, social/emotional consequences, and health-related problems of stroke survivors, and it comprises dichotomous (yes/no) responses for each item. LUNS was developed based on previous literature and semi-structured interviews with stroke survivors [12,13]. In an original validation study among 850 British stroke survivors, LUNS showed good acceptability (average completion time of 6 minutes and low missing item rate) [12]. Test-retest reliability analysis revealed high agreement, ranging from 78%–99% for item responses, and a kappa coefficient ranging from 0.45–0.67. Additionally, the validity of the LUNS was corroborated by the identification of unmet needs that consistently correlated with poorer health, as measured by the Short Form 12 (SF-12) questionnaire and Frenchay Activities Index (FAI). However, the LUNS has not been widely translated and validated in languages other than Dutch [14]. The unmet needs of stroke survivors can be influenced by various health and social factors and different coping strategies are required depending on cultural backgrounds. Thus, using the same standardized and validated tool to evaluate unmet needs after stroke in various languages will allow for more inclusion of minority groups in multiethnic countries and enable global comparisons of unmet needs after stroke.
This study had two main objectives: the translation of the 22-item LUNS questionnaire into Korean and the evaluation of its validity among stroke patients in Korea. In addition, we analyzed the reliability between the face-to-face (first test) and telephonic (second test) surveys, to determine the reliability of follow-up telephonic surveys using the LUNS instrument. The successful implementation of this approach provides a valuable opportunity to include a larger cohort of stroke survivors in future research.
The translation of the LUNS instrument was conducted with permission from the authors of the original LUNS study for the use of the questionnaire. This study was structured into three distinct components. The first part involved the translation and cross-cultural adaptation of the original English version of the LUNS instrument into Korean (LUNS-K). The second part focused on the validation of the LUNS-K. Finally, we assessed the reliability between the face-to-face (first test) and the telephonic (second test) surveys. The translation and cross-cultural adaptation of the LUNS to Korean was based on the 10 steps described in the International Society for Pharmacoeconomics and Outcomes Research Patient-Reported Outcomes Translation and Linguistic Validation Task Force guidelines [15]. The Institutional Review Boards (IRBs) of Seoul National University Bundang Hospital (IRB No. B-2006-616-307) and Kangwon National University Hospital (IRB No. KNUH-2020-05-005-004) approved the study protocol. All participants provided written informed consent after receiving detailed information about the study.
The original version of the LUNS was initially translated from English to Korean. The translations were independently performed by three translators who were Korean native speakers. Two of the translators had no medical background, whereas the third translator was part of the medical team that participated in the study. The three translated versions were reviewed, and a few discrepancies were reconciled by consensus. A synthetic version was created. The reconciled Korean version was back-translated into English by two Korean-American native English speakers who were fluent in Korean (one medical personnel and one non-medical personnel), and blinded to the original English version. An expert committee comprising health professionals, translators, and linguists reviewed the synthesized and back-translated versions for inconsistencies before modifying them to reflect the most accurate meaning in Korean. An expert committee reviewed the linguistic and cultural qualities of the modified version.
This pre-final version was field-tested on six Korean patients with chronic stroke (n=3 males; mean age, 65.8±23.5 years) at Seoul National University Bundang Hospital for the cognitive debriefing phase. The patients underwent qualitative semi-structured interviews investigating the questionnaire and their understanding of the questions. The interviewees were patients who visited our outpatient clinic because of chronic stroke. We measured the questionnaire completion time for four of the six patients. The semi-structured interviews were based on eight questions. All questions were answered on a visual analog scale of 100 mm where “0” represented “not useable at all” and “100” represented “very useable” [16]. After cognitive debriefing, ambiguous expressions were modified through discussion. An expert committee reviewed the final LUNS-K.
The validation and reliability analysis of the LUNS-K involved a total of 66 post-stroke patients who attended the outpatient clinics of the Department of Rehabilitation Medicine at Seoul National University Bundang Hospital and Kangwon National University Hospital between July 2020 and February 2021. The study included adult stroke patients aged 18 years or older, who were outpatients and had experienced a stroke at least 6 months prior. Participants were required to have the communication and cognitive abilities necessary to independently complete the questionnaire. We included patients who reside at home and have surpassed a minimum of 3 months since stroke onset. Those unable to answer the questionnaire due to cognitive decline were excluded from the study.
During the initial face-to-face interview, participants provided information regarding their age, sex, education level, residence (home or facility), type of stroke (cerebral infarction, cerebral hemorrhage, or unknown), stroke stage (subacute, <6 months; early chronic, 6–18 months; late chronic, >18 months) [17], and modified Rankin Scale (mRS) were investigated (0=no symptoms; 1=no significant disability despite symptoms; 2=slight disability; 3=moderate disability; 4=moderately severe disability; and 5=severe disability) [18]. Two weeks after the first interview, a telephonic survey was conducted to verify the reliability of the LUNS-K for respondents who consented.
To evaluate the validity of the LUNS-K questionnaire, a survey was conducted using the FAI and the SF-12 to assess the quality of life. The FAI is a specific index developed to assess disability and handicap in stroke patients. It consists of 15 items that capture various activities related to the household, work or leisure, and outdoor life. Participants rated each item on a four-category scale ranging from “never” (1) to “most of the time” (4). The total FAI score ranges from 15 (lower activity) to 60 (higher activity). This index provides insight into activities that reflect a greater level of independence and social functioning. The Korean version of the FAI was translated and demonstrated satisfactory reliability, with a Cronbach’s α coefficient of 0.796 [19].
We used the Korean version of the SF-12 v2 [20], a short-form health survey with 12 items obtained directly from the SF-36 v2. The SF-12 v2 consists of the following eight scales: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. We used scales of 0–100 based on the scoring manual. Two summary measures were derived from the 12 items (Physical Component Summary [PCS] and Mental Component Summary [MCS]).
The median and interquartile range (minimum-maximum) of values on the FAI, SF-12 MCS, and SF-12 PCS were calculated for patients with and without unmet needs per item. The Mann–Whitney U-test was used to determine the statistical significance of the difference in FAI, SF-12 MCS, and SF-12 PCS scores between those with and without unmet needs.
To evaluate the level of agreement between the face-to-face and the telephonic surveys, Cohen’s kappa coefficient (κ), which ranges from -1 to +1, was measured. A κ-value of 0 indicates the level of agreement that would be expected by chance alone, while a value of 1 signifies a perfect agreement between the raters [21]. Additionally, the percentage agreement was calculated and ranged from 0 to 100 where 0 denotes no agreement and 100 represents perfect agreement.
During the reconciliation of the forward-translated versions into a single forward translation in the cognitive debriefing phase, six patients were requested to complete the LUNS-K and a questionnaire assessing their understanding of the questions. During the field testing of the prefinal LUNS-K version, the questionnaire completion time was <5 minutes on average. Furthermore, patients rated the length, readability, and clarity of the LUNS-K and reported that the questionnaire had a good layout and was organized in a clear manner (Table 1). Overall, 22 items were translated and validated (Supplementary Table S1).
In total, 66 patients with stroke participated in the initial evaluation, with 49 of those recruited from Hospital A and 17 from Hospital B. Five participants opted out of the re-evaluation process and four patients who initially agreed to the second evaluation did not respond to phone calls. Ultimately, 57 participants (86.4% of the original sample) completed the second (telephonic) survey. Table 2 shows the baseline characteristics of the 66 patients who participated in the first evaluation. Forty-nine of the 66 patients (74.2%) were male (mean age, 61.2±12.8 years). For the educational level, three patients did not respond and most responders were high school graduates (n=20, 31.7%). Most participants (98.5%) lived at home. For stroke type, ischemic, hemorrhagic, and unknown stroke types comprised 51.5%, 43.9%, and 4.5%, respectively. The proportion of participants with a period of 3–6 months, 6–18 months, and >18 months after stroke onset were 9.1%, 22.7%, and 68.2%, respectively. The disability level was assessed using the mRS, and moderate disability (mRS=3) was the most frequent disability (28.8%). The SF-12 MCS, SF-12 PCS, and FAI total scores were 41.5±13.8, 36.7±8.4, and 31.2±11.9, respectively.
The concurrent validity findings for the 66 participants are summarized in Table 3. Among the 21 items, individuals without unmet needs exhibited a higher level of daily activity and quality of life than those with unmet needs except one item (item #1), where individuals with unmet needs reported a higher daily activity and quality of life, although the difference was not statistically significant. Notably, significant differences were observed in the SF-12 MCS, SF-12 PCS, and FAI scores for 12 items.
Among the 21 items, individuals without unmet needs demonstrated significantly higher FAI scores in areas related to levels of independence and social functioning, such as the need for aids or adaptations inside, assistance with concentration or memory, support for mood, advice on daily occupations, and information on holidays. Similarly, the SF-12 PCS scores in individuals without unmet needs were significantly higher for pain, difficulties walking, need for aids or adaptations inside, need for aids or adaptations outside, help with personal care, advice on daily occupations, and information on holidays. Regarding the SF-12 MCS, individuals without unmet needs had significantly higher scores for fear of falling, information on public transportation, help in the household, help with concentration or memory, help with mood, advice on daily occupations, and information on holidays.
Table 4 shows the results of the reliability evaluation conducted using 57 patients. One item had an almost perfect agreement (κ >0.80), 11 items demonstrated substantial agreement (κ, 0.61–0.80), eight items showed moderate agreement (κ, 0.41–0.60), and two items showed fair agreement (κ, 0.21–0.40), with the percentage of agreement ranging from 73.7% (pain) to 93.0% (help with bladder or bowel problems).
Common unmet needs (>50%) reported by participants during the face-to-face (T1) interview included information on stroke (80%), fear of falling (65%), help with applying for benefits (55%), pain (52%), and help with mood (52%). Less common unmet needs (<30%) during T1 interviews included advice on physical relationships (9%), help with bladder or bowel problems (15%), need for aid or adaptations outside (17%), information on moving to another home (21%), information on employment (24%), and help in the household (24%; Fig. 1).
In this study, we translated and cross-culturally adapted the LUNS questionnaire to Korean and assessed its validity and test-retest reliability in stroke survivors. Our findings show that the LUNS-K is a reliable and valid instrument for measuring unmet needs in Korean patients with stroke. Field testing is a comprehensive and feasible method. In a larger group, field testing showed high agreement between the face-to-face and telephone tests and yielded a few missing items. For 12 of 22 items, those with unmet needs had significantly lower scores on one or more instruments for activities and quality of life, demonstrating their validity.
In terms of concurrent validity, the results of the original validation study conducted by the LoTS care LUNS study team showed that 21 items were significantly associated with lower scores on the FAI or the SF-12. In our study, however, only 12 items showed significant associations. This difference in concurrent validity findings could be attributed to several factors. First, our study had a smaller sample size, which might have lowered the statistical power and limited the ability to detect significant associations. Second, the higher percentage of unmet needs per item in our study population might have contributed to the reduced number of significant associations. Lastly, the longer timeframe in our study, including stroke survivors at various stages of recovery, could have influenced the concurrent validity results compared to the original study, which focused on participants within the 3–6 months post-stroke period.
In this study, we compared the results of the first survey conducted in person with the second survey conducted via telephone. Of 22 items, 20 showed a moderate reliability or better, while two items (items #7 and #18) showed a marginally fair reliability (κ=0.394 and 0.397, respectively). Considering that the two surveys were conducted using different methods, the reliability of the LUNS-K is believed to be acceptable for clinical usage [22].
The unmet need for aids or adaptation outside only showed marginal reliability between the surveys, with 16.7% of the participants providing a “yes” response to the question. The LUNS-K questionnaire included examples of outside adaptations such as “ramp” or “rail” as in the original LUNS. However, these modifications of the outside environment can be unfamiliar in a Korean setting, as Korean people tend to live in apartments. This lack of familiarity with outside adaptations may have made the question vague for the participants. Thus, a more detailed example or description of the item would increase the reliability of the LUNS-K.
Only 9% of the participants reported that they had an unmet need for “advice on physical relationships.” The very low rate of this unmet need may be associated with its low test-retest reliability (κ<0.4). A previous study including Korean female patients with cervical cancer reported a low response rate for obtaining sexuality-related information [23]. They reported that participants who did not respond to sexuality-related items showed significantly different characteristics from those who responded; they were more likely to be older, unmarried, less educated, unemployed, earning a lower income, and at an advanced stage of the disease. In this study, participants did not avoid responding to sex-related items. However, considering the avoidance of sexual questions among older Koreans, they might have avoided providing an accurate response by expressing no unmet needs. Therefore, we cannot rule out the possibility that they selected “no unmet need” rather than avoid answering because the first survey was conducted face-to-face. Moreover, the question regarding help with voiding/defecation difficulty, which patients may also tend to avoid had a low prevalence (15.2%) but showed substantial reliability (κ=0.709). As such, the causal relationship between low prevalence and low reliability remains unclear. Therefore, the results of sex-related needs in future surveys on unmet needs should be interpreted with caution, due to the older age of stroke survivors and the potential cultural influences affecting their responses.
Identification of unmet needs after stroke is crucial to inform health and social service provision. In addition, understanding the specific needs of stroke survivors is vital for providing patient-centered health and social care. The prevalence of unmet long-term needs is high among survivors of stroke [8]. Patients with stroke who participated in this study most frequently reported a need for information on stroke, followed by concerns about falls, pain, and depression/anger/anxiety. Our findings are corroborated by results from a study on a Dutch stroke population [14] that reported the highest unmet needs in the stroke information domain, suggesting that clinicians should assess the need and provide sufficient information to patients with chronic stroke.
The use of different survey methods is a notable characteristic of the study. We conducted the second survey via telephone, and the response rate was 86.4%. The telephone survey method reportedly has several advantages compared with the postal survey method, including a higher response rate, reduced responder selection bias, and higher retest reliability [24]. Additionally, administering questionnaires via telephone to non-responders of postal surveys resulted in higher response rates (>80%) [25]. Telephone surveys are particularly suitable for stroke patients with physical disabilities and limited mobility. Additionally, with the increasing adoption of social distancing procedures and telecommunication, as seen during the coronavirus disease 2019 pandemic, face-to-face and group meetings have significantly declined. As a result, non-face-to-face survey methods, including telephonic surveys, are now preferred over in-person surveys. Also, conducting in-person interviews requires substantial resources and is impractical for large community populations. Therefore, we anticipate that telephonic surveys will be increasingly employed in future studies.
Our study had a few limitations. First, the inclusion of participants at different stroke stages resulted in various post-stroke periods. Patients with stroke can be classified into different stages, including acute (<3 weeks), subacute (3 weeks–6 months), early chronic (6–18 months), and late chronic (>18 months) [17]. The possibility of changes in unmet needs between the two tests (initical and second surveys) in subacute post-stroke patients could not be excluded. However, the majority of our participants were in the late chronic stage (68.2%), implying that the test was performed in a stable population. Further research should investigate and analyze unmet needs based on the specific stages of chronicity in stroke patients. Second, we did not conduct a test-retest of the face-to-face survey. Instead, the second survey was conducted via telephone. The difference in survey methods may have affected the reliability assessment of the questionnaire, particularly because people tend to respond more easily to sensitive questions via telephone than face-to-face [26,27]. Nonetheless, the advantages of administering telephonic surveys were considerable; the response rate of the second survey was >80%. Moreover, assessing the LUNS-K using both face-to-face and telephone interviews confirmed the validity and reliability of this instrument, as well as its feasibility in clinical settings using different survey methods. Finally, the participants in this study comprised post-stroke patients with the cognitive ability to understand and answer the LUNS-K. This means that the prevalence and validity of the LUNS-K in patients with severe cognitive impairment remains uninvestigated. To address this issue, further studies should include patients with stroke who have severe cognitive impairments by including these patients’ caregivers as needed.
In conclusion, the LUNS-K is a reliable and valid instrument for assessing unmet health needs in Korean patients with stroke. Unmet needs and low health questionnaire values (FAI, MCS, and PCS) were confirmed for 12 items when the validity of the LUNS-K was analyzed. Although the agreement is lower in some parts of the Korean version compared to the original English version, the reliability of the LUNS-K is still acceptable. In addition, this instrument can be reliably applied telephonically as well.
FUNDING INFORMATION
This study was supported by the Korean National Institute of Health Research Project (project No. 2020ER630602).
AUTHOR CONTRIBUTION
Conceptualization: Baek S, Kim WS, Paik NJ. Methodology: Baek S, Kim WS, Jung YS, Chang WK, Paik NJ. Formal analysis: Baek S, Jung YS, Chang WK, Kim G. Funding acquisition: Paik NJ. Project administration: Baek S, Kim WS, Park YH, Jung YS, Chang WK, Kim G, Paik NJ. Visualization: Baek S, Kim WS, Jung YS, Chang WK. Writing – original draft: Baek S. Writing – review and editing: Baek S, Kim WS, Jung YS, Chang WK, Kim G, Paik NJ. Approval of final manuscript: all authors.
ACKNOWLEDGMENTS
We would like to express our sincere appreciation to Professor Anne Forster for her invaluable assistance in translating the original LUNS into the Korean version. The original development of the LUNS was funded by UK National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (Grant Reference Number RP-PG-0606-1128). We would also like to thank Hee Sung Kim for interviewing participants for data acquisition and Ha Won Park for translating the LUNS English version to Korean.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.5535/arm.23044.
Supplementary Table S1.
The Korean version of the Longer-term Unmet Needs after Stroke (LUNS) (Korean)
Fig. 1.
The percentage of stroke survivors reporting unmet needs for each item of the Longer-term Unmet Needs after Stroke instrument into Korean during face-to-face (T1, n=66) and telephonic (T2, n=57) interviews.
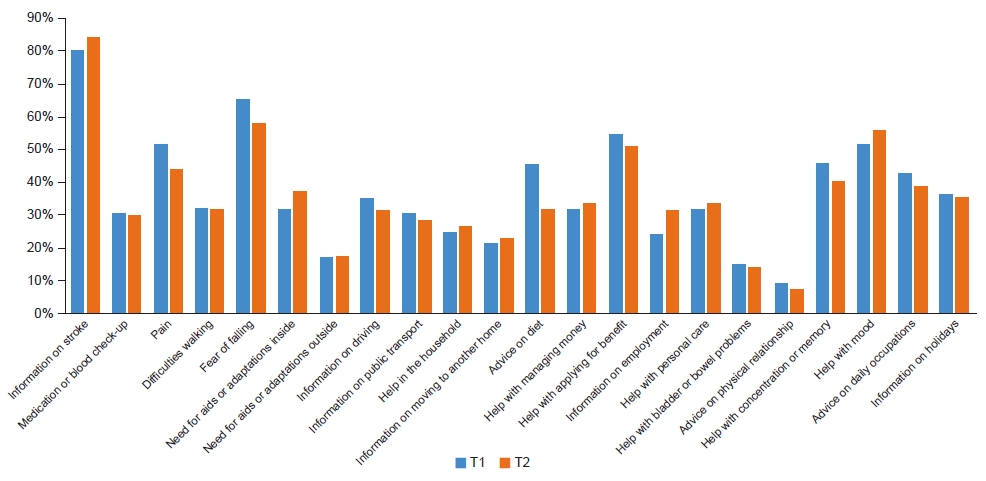
Table 1.
The usability of the Longer-term Unmet Needs after Stroke instrument into Korean (n=6)
Table 2.
Socio-demographic characteristics of participants
| Characteristics | Value (n=66) |
|---|---|
| Sex (male) | 49 (74.2) |
| Age (yr) | 61.2±12.8 (range, 34–87) |
| Educationa) | |
| Middle school or lower | 18 (28.6) |
| High school | 20 (31.7) |
| College or university | 18 (28.6) |
| Graduate school | 7 (11.1) |
| Current residence (home) | 65 (98.5) |
| Stroke types | |
| Ischemic | 34 (51.5) |
| Hemorrhagic | 29 (43.9) |
| Unknown | 3 (4.5) |
| Stroke stage | |
| Subacute (3–6 mo) | 6 (9.1) |
| Early chronic (6–18 mo) | 15 (22.7) |
| Late chronic (>18 mo) | 45 (68.2) |
| Modified Rankin Scale | |
| 0 | 1 (1.5) |
| 1 | 14 (21.2) |
| 2 | 17 (25.8) |
| 3 | 19 (28.8) |
| 4 | 10 (15.2) |
| 5 | 5 (7.6) |
| SF-12 Mental Component Summary score | 41.5±13.8 (16.6–65.8) |
| SF-12 Physical Component Summary score | 36.7±8.4 (20.2–58.7) |
| Frenchay Activities Index total score | 31.2±11.9 (15–57) |
Table 3.
Concurrent validity of the LUNS questionnaire using the FAI, SF-12 PCS, and SF-12 MCS scores (n=66)
| LUNS items (no. of unmet need, %) |
FAI score |
SF-12 PCS score |
SF-12 MCS score |
||||||
|---|---|---|---|---|---|---|---|---|---|
| No unmet need | Unmet need | p-value | No unmet need | Unmet need | p-value | No unmet need | Unmet need | p-value | |
| 1. Information on stroke (n=53, 80.3) | 23 (19–31) | 32 (23–41) | 0.074 | 33.1 (29.8–40.4) | 36.4 (30.4–42.3) | 0.802 | 36.8 (24.7–51.5) | 41 (31.5–54.8) | 0.306 |
| 2. Medication or blood check-up (n=20, 30.3) | 31 (22.3–39.8) | 30.5 (18.5–39.0) | 0.498 | 36.7 (30.7–42.8) | 35.9 (30.0–39.6) | 0.339 | 45.5 (30.7–54.7) | 37 (29.7–47.8) | 0.174 |
| 3. Pain (n=34, 51.5) | 32 (23.3–39.8) | 30.5 (19.0–38.8) | 0.453 | 39.9 (34.9–43.1) | 33.3 (29.1–36.3)* | 0.080 | 45.8 (32.3–55.2) | 37 (30.1–51.2) | 0.257 |
| 4. Difficulties walking (n=21, 31.8) | 32 (23–43) | 25 (19.0–36.0) | 0.046 | 39.9 (31.7–44.6) | 33.5 (29.8–36.0)** | 0.007 | 46.4 (32.5–55.5) | 32 (25.2–43.5) | 0.060 |
| 5. Fear of falling (n=43, 65.2) | 32 (25.5–44.0) | 30 (19.0–38.5) | 0.170 | 39.5 (31.5–47.1) | 35.7 (29.6–40.5) | 0.041 | 51.6 (42.8–59.7) | 34.8 (28.4–46.8)** | 0.001 |
| 6. Need for aids or adaptations inside (n=21, 31.8) | 36 (26–43) | 22 (17–28)** | <0.001 | 39.9 (32.7–44.0) | 32.3 (27.8–34.6)** | <0.001 | 44.7 (31.4–54.8) | 34.8 (29.9–46.8) | 0.391 |
| 7. Need for aids or adaptations outside (n=11, 16.7) | 31 (20.5–40.5) | 25 (21.0–34.5) | 0.278 | 36.5 (31.2–42.7) | 32.3 (28.6–34.9)* | 0.057 | 43.5 (30.9–54.8) | 34.8 (30.9–44.5) | 0.665 |
| 8. Information on driving (n=23, 34.8) | 31 (23.0–40.5) | 26 (19.5–38.0) | 0.400 | 36 (30.0–42.3) | 36.3 (32–42) | 0.859 | 41 (31.5–54.6) | 40.8 (26.7–51.9) | 0.421 |
| 9. Information on public transportation (n=20, 30.3) | 31.5 (23.0–40.8) | 24.5 (19.0–36.3) | 0.114 | 38.4 (30.4–42.8) | 34.4 (30.6–37.1) | 0.230 | 46.6 (31.7–55.4) | 33.4 (28.5–43.8)* | 0.028 |
| 10. Help in the household (n=16, 24.2) | 31 (21.5–39.8) | 27.5 (19–39) | 0.480 | 36.3 (29.9–42.8) | 35.4 (32.9–41.5) | 0.749 | 45.9 (32.1–54.8) | 30.7 (24.5–37.5)* | 0.013 |
| 11. Information on moving to another home (n=14, 21.2) | 30 (19.0–39.3) | 34.5 (24.5–38.8) | 0.731 | 36.3 (30.4–42.5) | 34.8 (31.5–41.0) | 0.485 | 44.1 (30.4–55.0) | 37 (31.4–45.0) | 0.313 |
| 12. Advice on the diet (n=30, 45.5) | 32 (22.0–39.5) | 28.5 (20.3–39.0) | 0.541 | 39.3 (31.1–43.1) | 34.2 (29.3–40.2) | 0.150 | 43.5 (34.6–52.4) | 33.6 (30.1–55.0) | 0.519 |
| 13. Help with managing money (n=21, 31.8) | 32 (19–41) | 26 (22–39) | 0.237 | 39.6 (30.4–43.8) | 35 (30.3–36.3) | 0.139 | 41 (31.4–54.3) | 40.6 (29.9–54.8) | 0.845 |
| 14. Help with applying for benefits (n=36, 54.5) | 36 (20.8–41.8) | 26.5 (20.5–37.5) | 0.265 | 40.5 (29.9–44.5) | 34.2 (30.4–37.6) | 0.203 | 43.5 (32–54) | 35.9 (30.4–54.8) | 0.618 |
| 15. Information on employment (n=16, 24.2) | 32 (20.3–40.5) | 27 (21.3–37.5) | 0.480 | 36.4 (30.2–42.8) | 34.3 (30.4–39.1) | 0.427 | 44.1 (31.5–55.0) | 33.6 (25.0–45.7) | 0.057 |
| 16. Help with personal care (n=21, 31.8) | 33 (23–42) | 24 (19–33) | 0.029 | 39.9 (31.4–44.6) | 33.7 (30.3–36.0)* | 0.010 | 43.4 (31.7–54.8) | 34.8 (28.7–52.2) | 0.278 |
| 17. Help with bladder or bowel problems (n=10, 15.2) | 32 (22.8–40.3) | 22 (19–26) | 0.049 | 36.4 (31.3–42.5) | 31.6 (29.2–34.4) | 0.110 | 44.1 (31.1–55.0) | 34.8 (29.4–36.6) | 0.106 |
| 18. Advice on the physical relationship (n=6, 9.1) | 31.5 (19.8–40.3) | 24 (21.5–28.8) | 0.249 | 36.3 (30.9–42.5) | 30.6 (28.1–35.3) | 0.074 | 42.2 (30.4–54.4) | 35.8 (33.0–50.5) | 0.710 |
| 19. Help with concentration or memory (n=30, 45.5) | 36.5 (25.8–46.0) | 24.5 (18.3–32.8)** | 0.003 | 38 (31.3–45.1) | 35.5 (30.3–39.8) | 0.059 | 49.6 (39.8–57.4) | 31.8 (24.6–40.9)** | <0.001 |
| 20. Help with mood (n=34, 51.5) | 36.5 (25–46) | 26 (19–36)* | 0.006 | 36.8 (31.6–44.7) | 35.5 (30.3–41.6) | 0.247 | 54.5 (43.8–59.1) | 31.8 (24.6–40.0)** | <0.001 |
| 21. Advice on daily occupations (n=28, 42.4) | 36 (24.3–43.5) | 25.5 (19–33)* | 0.019 | 39.9 (31.6–44.9) | 33.6 (30.4–37.6)* | 0.032 | 47.9 (37.2–56.4) | 33.3 (27.4–44.0)** | 0.002 |
| 22. Information on holidays (n=24, 36.4) | 36 (25.0–43.5) | 23.5 (19–33)* | 0.014 | 39.6 (31.6–44.5) | 33.3 (30.2–36.1)* | 0.024 | 47.9 (35.7–55.7) | 31.8 (24.7–38.2)** | 0.001 |
Table 4.
Reliability between the face-to-face and telephonic LUNS-K surveys (n=57)
| LUNS items | Kappa statistic (95% CI) | Percentage agreement (%) |
|---|---|---|
| 1. Information on stroke | 0.637** (0.372–0.902) | 89.5 |
| 2. Medication or blood check-up | 0.446** (0.191–0.701) | 77.2 |
| 3. Pain | 0.477** (0.253–0.701) | 73.7 |
| 4. Difficulties walking | 0.414** (0.158–0.670) | 75.4 |
| 5. Fear of falling | 0.632** (0.427–0.836) | 82.5 |
| 6. Need for aids or adaptations inside | 0.806** (0.644–0.967) | 91.2 |
| 7. Need for aids or adaptations outside | 0.394** (0.086–0.701) | 82.5 |
| 8. Information on driving | 0.763** (0.586–0.941) | 89.5 |
| 9. Information on public transportation | 0.531** (0.288–0.774) | 80.7 |
| 10. Help in households | 0.662** (0.433–0.890) | 87.7 |
| 11. Information on moving to another home | 0.579** (0.318–0.839) | 86.0 |
| 12. Advice on diet | 0.565** (0.356–0.774) | 78.9 |
| 13. Help with managing money | 0.630** (0.412–0.848) | 84.2 |
| 14. Help with applying for the benefit | 0.649** (0.451–0.846) | 82.5 |
| 15. Information on employment | 0.532** (0.292–0.773) | 80.7 |
| 16. Help with personal care | 0.605** (0.385–0.825) | 82.5 |
| 17. Help with bladder or bowel problems | 0.709** (0.441–0.977) | 93.0 |
| 18. Advice on the physical relationship | 0.397** (-0.029–0.824) | 91.2 |
| 19. Help with concentration or memory | 0.679** (0.487–0.870) | 84.2 |
| 20. Help with the mood | 0.573** (0.358–0.787) | 78.9 |
| 21. Advice on daily occupation | 0.709** (0.522–0.895) | 86.0 |
| 22. Information on holidays | 0.692** (0.495–0.889) | 86.0 |
REFERENCES
1. GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18:439-58.


2. Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke 2019;21:42-59.



3. Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016;47:e98-169. Erratum in: Stroke 2017;48:e78. Erratum in: Stroke 2017;48:e369.

4. Kim DY, Kim YH, Lee J, Chang WH, Kim MW, Pyun SB, et al. Clinical practice guideline for stroke rehabilitation in Korea 2016. Brain Neurorehabil 2017;10(Suppl 1): e11.
5. Murray J, Ashworth R, Forster A, Young J. Developing a primary care-based stroke service: a review of the qualitative literature. Br J Gen Pract 2003;53:137-42.


6. Chang WH, Sohn MK, Lee J, Kim DY, Lee SG, Shin YI, et al. Predictors of functional level and quality of life at 6 months after a first-ever stroke: the KOSCO study. J Neurol 2016;263:1166-77.



7. Im HW, Kim WS, Kim S, Paik NJ. Prevalence of worsening problems using post-stroke checklist and associations with quality of life in patients with stroke. J Stroke Cerebrovasc Dis 2020;29:105406.


8. Chen T, Zhang B, Deng Y, Fan JC, Zhang L, Song F. Long-term unmet needs after stroke: systematic review of evidence from survey studies. BMJ Open 2019;9:e028137.



9. Andrew NE, Kilkenny MF, Lannin NA, Cadilhac DA. Is health-related quality of life between 90 and 180 days following stroke associated with long-term unmet needs? Qual Life Res 2016;25:2053-62.



10. Andrew NE, Kilkenny MF, Naylor R, Purvis T, Cadilhac DA. The relationship between caregiver impacts and the unmet needs of survivors of stroke. Patient Prefer Adherence 2015;9:1065-73.



11. Kim KT, Chang WK, Jung YS, Jee S, Sohn MK, Ko SH, et al. Unmet needs for rehabilitative management in common health-related problems negatively impact the quality of life of community-dwelling stroke survivors. Front Neurol 2021;12:758536.



12. LoTS care LUNS study team. Validation of the longer-term unmet needs after stroke (LUNS) monitoring tool: a multicentre study. Clin Rehabil 2013;27:1020-8.



13. Murray J, Young J, Forster A, Ashworth R. Developing a primary care-based stroke model: the prevalence of longer-term problems experienced by patients and carers. Br J Gen Pract 2003;53:803-7.


14. Groeneveld IF, Arwert HJ, Goossens PH, Vliet Vlieland TPM. The Longer-term Unmet Needs after Stroke Questionnaire: cross-cultural adaptation, reliability, and concurrent validity in a Dutch population. J Stroke Cerebrovasc Dis 2018;27:267-75.


15. Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for Translation and Cultural Adaptation. Value Health 2005;8:94-104.


16. Timmerman H, Wolff AP, Schreyer T, Outermans J, Evers AW, Freynhagen R, et al. Cross-cultural adaptation to the Dutch language of the PainDETECT-Questionnaire. Pain Pract 2013;13:206-14.


17. Ballester BR, Maier M, Duff A, Cameirão M, Bermúdez S, Duarte E, et al. A critical time window for recovery extends beyond one-year post-stroke. J Neurophysiol 2019;122:350-7.



18. Wilson JT, Hareendran A, Grant M, Baird T, Schulz UG, Muir KW, et al. Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale. Stroke 2002;33:2243-6.


19. Han CW, Lee EJ, Kohzuki M. Validity and reliability of the Frenchay Activities Index for community-dwelling elderly in South Korea. Tohoku J Exp Med 2009;217:163-8.


20. Kim SH, Jo MW, Ahn J, Ock M, Shin S, Park J. Assessment of psychometric properties of the Korean SF-12 v2 in the general population. BMC Public Health 2014;14:1086.




22. Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther 2005;85:257-68.



23. Shin DW, Choi JE, Miyashita M, Choi JY, Kang J, Baik YJ, et al. Cross-cultural application of the Korean version of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 15-Palliative Care. J Pain Symptom Manage 2011;41:478-84.


24. Duncan P, Reker D, Kwon S, Lai SM, Studenski S, Perera S, et al. Measuring stroke impact with the stroke impact scale: telephone versus mail administration in veterans with stroke. Med Care 2005;43:507-15.


25. Sibbald B, Addington-Hall J, Brenneman D, Freeling P. Telephone versus postal surveys of general practitioners: methodological considerations. Br J Gen Pract 1994;44:297-300.


- TOOLS







