- Search
| Ann Rehabil Med > Volume 47(4); 2023 > Article |
|
I carefully studied the proposal from Lee et al. [1] describing a nerve conduction study (NCS) algorithm for grading the severity of diabetic distal symmetric sensorimotor polyneuropathy (DSPN). Despite the articleŌĆÖs brevity, it was evident that the authors put substantial effort into research and contemplation on the topic. Henceforth, I will refer to this diagnostic NCS algorithm as ŌĆ£LeeŌĆÖs Severity SystemŌĆØ or ŌĆ£LeeŌĆÖs algorithm.ŌĆØ
In 2020, the estimated prevalence of diabetes mellitus among Korean adults was 16.7% [2]. Diabetic neuropathy, which affects approximately one-third of the patients with type 1 or type 2 diabetes, increases the risk of painless foot ulcers leading to amputations [3]. Although the NCS is the most comprehensive and accurate diagnostic tool for DSPN, it is not routinely integrated into standard clinical care for diabetic patients. This reluctance is understandable; without concrete evidence that NCS enhances clinical outcomes, the associated costs, time commitments, and potential patient discomfort might deter clinicians.
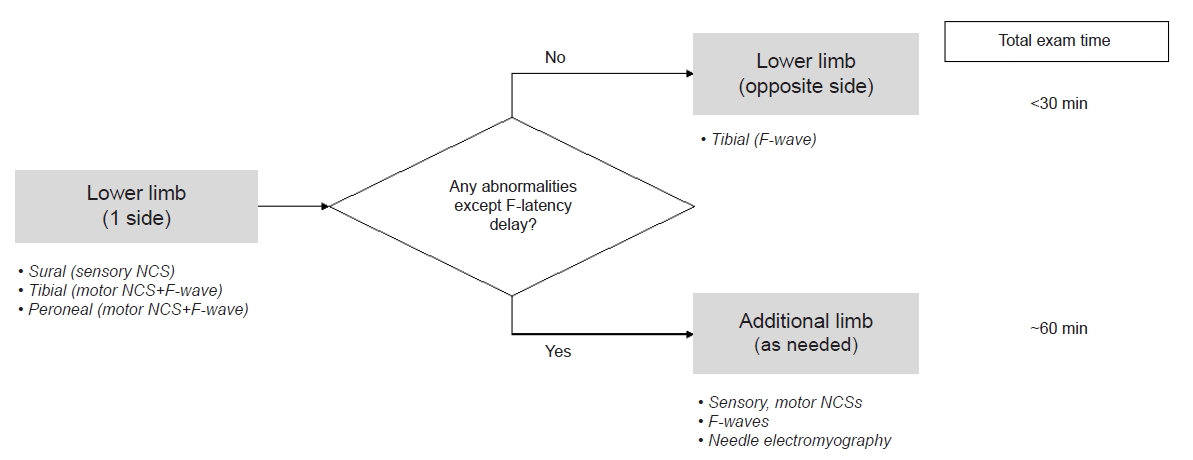
In this regard, LeeŌĆÖs algorithm is primarily efficient, offering several advantages. Using this algorithm, NCS of the lower extremities that are more vulnerable at an earlier stage of DSPN can be first performed. If these results are within normal limits, the examination can be completed with only a tibial F-wave study in the contralateral lower limb. In addition, LeeŌĆÖs algorithm suggests that the contralateral lower extremity or non-dominant upper extremity can be examined only when there is an additional need. Taken together, LeeŌĆÖs Severity System has the potential to significantly reduce the NCS examination time, especially in patients with early-stage to mild DSPN. Applying these streamlined algorithms will minimize the time, cost, and discomfort associated with NCS, allowing its application to most patients with diabetes. The NCS is more sensitive than the Semmes-Weinstein monofilament test and can comprehensively assess the entire sensory and motor systems. It would greatly benefit if the NCS could be completed in as little as 30 minutes.
LeeŌĆÖs Severity System employs an ordinal scale that classifies DSPN severity into five stages based on NCS outcomes. This framework offers significant clinical utility, presenting a nuanced understanding of disease severity rather than a simple binary diagnosis of the presence or absence of DSPN. Furthermore, it identifies ŌĆ£early stageŌĆØ DSPN, potentially a pivotal therapeutic juncture. Baba et al. introduced a comparable DSPN severity scale [4]. The mild, moderate, and severe grades in LeeŌĆÖs Severity System mirror grades 2, 3, and 4 of BabaŌĆÖs classification, diagnostic criteria essentially aligning. However, disparities arise in the early-stage criteria. While BabaŌĆÖs proposal encompassed a range of tests, LeeŌĆÖs strategy streamlined the criteria by focusing on F-waves. This condensation enhances practicality, particularly because F-wave studies share electrode montages with motor NCS, enabling seamless and consecutive assessments. The projected NCS test flowchart suggests potential completion within 30 minutes for mild cases, suggesting proactive interventions for early-stage patients (Fig. 1). In essence, LeeŌĆÖs algorithm refines and optimizes BabaŌĆÖs classification, offering a new system for expedited evaluation.
However, some areas in Lee's Severity System could benefit from further exploration. Electrodiagnostic laboratories use a variety of reference standards. Future adaptations might consider universal criteria such as ŌĆ£age-adjusted mean-2SDŌĆØ or ŌĆ£age-adjusted mean-extended uncertaintyŌĆØ instead of specific numbers such as ŌĆ£5 mV.ŌĆØ
According to a study published by Kim et al. [5] on ARM in 2022, the lower limit or reference range of tibial compound muscle action potential amplitude in healthy Korean men and women in their 50s is 9.1 and 8.3 mV, respectively. This is significantly higher than the step criteria of 5 and 2 mV suggested by LeeŌĆÖs algorithm. Similarly, the cut-off value for the base-to-peak sensory nerve action potential amplitude of the sural nerve was 9.8 and 10.4 ┬ĄV for men and women, respectively. Both BabaŌĆÖs and LeeŌĆÖs Severity System possess discernible grey areas. Refining LeeŌĆÖs approach to accommodate age-based reference range variations is of paramount importance. Further investigations on the ramifications of early detection and proactive intervention for health outcomes are warranted.
CONFLICTS OF INTEREST
Byung-Mo Oh is the Editor-in-Chief of Annals of Rehabilitation Medicine. The author did not engage in any part of the review and decision-making process for this manuscript. Otherwise, no potential conflict of interest relevant to this article was reported.
REFERENCES
1. Lee HJ, Kim DH, Kim KH. Diabetic distal symmetric sensorimotor polyneuropathy: a proposal of new electrodiagnostic evaluation. Ann Rehabil Med 2023;47:231-3.

2. Bae JH, Han KD, Ko SH, Yang YS, Choi JH, Choi KM, et al. Diabetes fact sheet in Korea 2021. Diabetes Metab J 2022;46:417-26.



3. Vinik AI. Clinical practice. Diabetic sensory and motor neuropathy. N Engl J Med 2016;374:1455-64. Erratum in: N Engl J Med 2016;374:1797. Erratum in: N Engl J Med 2016;375:1402.

- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 1,337 View
- 40 Download
- Related articles in ARM
-
The Objective Diagnostic Study for Diabetic Neuropathy1988 December;12(2)