- Search
| Ann Rehabil Med > Volume 47(1); 2023 > Article |
|
Abstract
Objective
To determine the efficacy of concentric vs. eccentric exercise in improving shoulder function, pain, and tendon characteristics for patients with rheumatoid arthritis and rotator cuff tendinopathy.
Methods
Forty patients with rheumatoid arthritis and rotator cuff tendinopathy were divided into either concentric or eccentric exercise groups, with 20 patients in each group. Patients received 12 sessions at a pace of 3 sessions per week. Shoulder Pain and Disability Index (SPADI), the visual analogue scale (VAS), supraspinatus and subscapularis thickness, echo pixels, and the Disease Activity Score-28-erythrocyte sedimentation rate (DAS-28-ESR) were assessed at baseline and post-treatment.
Rheumatoid arthritis (RA) is a chronic systemic inflammatory autoimmune disease that affects 0.5% of the general population and causes bone and cartilage destruction [1,2]. RA can affect tendon sheaths and the synovial membrane [3]. Hypervascularized synovitis is a hallmark of RA. Further, it may result in bony erosion, cartilage damage, joint destruction, bone marrow edema, and bursitis [4]. According to murine models, tendon involvement could be the first sign of inflammatory arthritis in the early stages of RA [5].
The shoulder joint is a common site of musculoskeletal pain in the general population, which was reported to affect between 7% and 27% of the population [6]. Rotator cuff disorders are pervasive and are the leading cause of shoulder disability. They account for approximately 30% to 70% of shoulder pain-related conditions [7]. The hazard ratio for rotator cuff tendinopathy was 1.56 in patients with RA compared to a matched control [8].
Patients with RA face the added risk of impaired shoulder function due to inflammation. Synovitis, bursitis, and tendinitis can cause decreased muscle strength, persistent pain, decreased range of motion, and joint destruction, resulting in functional loss and difficulties with daily activities [9]. Shoulder involvement in patients with RA includes synovitis, bursitis, and tendinopathy. Further progression may lead to the destruction of rotator cuff tendons and superior subluxation of the humeral head, thus, leading to the narrowing of the subacromial space [10,11].
Resistance training is commonly utilized to increase muscular strength, thus improving athletic performance, preventing injuries, and maintaining a healthy lifestyle [12]. Furthermore, exercise effectively improved pain and function in patients with RA, with no adverse effects reported [13]. Exercise is a crucial component of treating shoulder tendinopathy. Furthermore, both concentric and eccentric exercises were used to treat rotator cuff tendinopathy, yet evidence could not determine which was superior [14]. To the author’s knowledge, no randomized trial has compared concentric vs. eccentric exercises in patients with RA.
Consequently, this randomized comparative study aimed to determine the efficacy of concentric vs. eccentric exercise in improving shoulder function, pain, and tendon characteristics for rotator cuff tendinopathy in patients with RA.
This randomized comparative study was carried out between September 2021 and August 2022. This study was approved by the Institutional Review Board of the Faculty of Physical Therapy, Cairo University (P.T.REC/012/003375). Informed consent to publish this study was obtained from the patients. In addition, this study was registered at the National Institutes of Health (clinicaltrials.gov) with a registration number of NCT05054920.
Fifty-eight adult patients with RA based on the 2010 American College of Rheumatology/European League Against Rheumatism classification criteria were screened [15]. Patients were included in the study if they were diagnosed with rotator cuff tendinopathy based on clinical examination and further confirmed with musculoskeletal ultrasound (MSUS). Patients were excluded if they were scheduled for rotator cuff surgery, had a rotator cuff full-thickness tear, or had a shoulder fracture, dislocation, or surgery history. Patients with diabetes mellitus were also excluded from the study. Forty-four patients matched the inclusion and exclusion criteria. In addition, four patients refused to participate in the study due to a lack of interest. Forty patients agreed to participate in the study (Fig. 1). Patients were randomized into either concentric or eccentric exercise groups, with 20 patients in each group, using computer-generated random numbers.
Tendinopathy was graded as follows [16]:
Grade 0=normal tendon with average thickness and preserved fibrillar pattern.
Grade 1=reactive tendinopathy; the tendon is focally or diffusely swollen with diffuse hypoechogenicity.
Grade 2=tendon disrepair, with the same findings in grade 1 in addition to focal areas of hypoechogenicity and a lost fibrillar pattern.
Grade 3=degenerative tendinopathy, the same as grade 2 with more extensive lesions.
The sample size was calculated using G*Power 3.1 (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), assuming α (two-sided)=0.05 and 1-β=0.80, as observed in a previous study. The sample size was determined to be 34. We added six more to account for any dropouts that may occur. As a result, the study’s total sample size was 40 patients [17].
It is a self-reported questionnaire that assesses shoulder function. It is divided into two domains. The first domain assesses pain, while the second assesses shoulder disability. The patient answered each question by selecting a number from 0 to 10, with 0 indicating no pain or difficulty and 10 indicating the worst pain or so difficult that requires help. The total score was computed and divided by 130 to obtain a percentage. Therefore, Shoulder Pain and Disability Index (SPADI) is a valid and reliable tool for evaluating patients with rotator cuff tears and RA. The minimal clinically important difference (MCID) ranges between 8 and 13. Furthermore, it is validated in Arabic [18,19].
The visual analogue scale (VAS) was used to assess current pain. It consists of a 10 cm line labeled “0” at one end, indicating no pain, and a maximum of “10” at the other, indicating the worst pain. VAS is a valid and reliable method for chronic pain assessment. The MCID for rotator cuff pathology is 1.4 cm [20,21].
Shoulder MSUS was used to assess the supraspinatus tendon (in the modified Crass position) using a LOGIQ-P6 machine (GE Healthcare, Chicago, IL, USA) equipped with a high-frequency broadband linear array transducer at 10–13 MHz. MSUS was carried out by one operator who was blind to the physiotherapy protocol. The supraspinatus tendon thickness was measured in short axis view at 10, 15, and 20 mm lateral to the biceps tendon. The mean tendon thickness of the three measurements was calculated. The tendon echogenicity was determined by grayscale analysis of stored images using the standard histogram function in Adobe Photoshop (Adobe, San Jose, CA, USA). A region of interest of the entire tendon was defined using the freehand selection option to ensure that the overlying subacromial subdeltoid bursa, underlying cartilage, and bone were not involved [22,23]. Ultrasound is believed to be accurate, with sensitivity ranging from 92.4% to 96.0% and specificity ranging from 93.0% to 94.4% for diagnosing a full-thickness tear, and sensitivity ranging from 66.7% to 84.0% and specificity ranging from 89.0% to 93.5% for diagnosing a partial-thickness tear [24]. In addition, MSUS has shown moderate intra-rater reliability (Φ>0.50) [25].
(1) Subscapularis tendon thickness and echo pixels
The same operator operated the LOGIQ-P6 machine mentioned above to measure the subscapularis tendon in the long-axis view to the attachment at the lesser tuberosity. Again, the tendon echo pixels were calculated similarly to the supraspinatus [22,23].
(2) Disease Activity Score-28-erythrocyte sedimentation rate
A single physician, blind to the physiotherapy protocol, calculated the Disease Activity Score-28-erythrocyte sedimentation rate (DAS-28-ESR) score for all patients. It is an index based on the number of tenders, swollen joints, and ESR. It is a valid and reliable method for assessing disease activity in patients with RA [26].
A single therapist carried out the physiotherapy protocol for the two groups. A single physician, blind to all interventions and patient groupings, carried out the MSUS examination and calculated the DAS-28-ESR. The study’s goal and procedures were discussed with the patients. Patients were asked to sign an informed consent form if they agreed to participate in the study. Patients received 12 sessions at a pace of three sessions per week. All outcome measures were measured at baseline and after 12 sessions.
Both groups performed the pectoralis minor stretch using an active corner stretch with the patient in a standing position [27]. Moreover, the posterior capsule was also stretched using the sleeper stretch technique. Each stretching set was held for 30 seconds and repeated three times [28].
All exercises were performed with the patient standing. Elastic resistance bands were used for the exercises, with the level of resistance based on the patient’s tolerance. Furthermore, each patient completed three sets of each exercise. Each set was composed of 10 repetitions of each exercise.
(1) Internal and external rotation exercises
Elastic resistance was attached to the wall bar, and the patient was instructed to move her forearm towards or away from her body (Fig. 2) [29].
(2) Abductor strengthening
(1) Internal and external rotation exercises
Patients were positioned at the end of the internal or external rotation range with elastic resistance in tension. The patient was instructed to gradually control the relaxation of the elastic resistance while slowly returning to the neutral position [29].
(2) Abductor strengthening
The patient’s arm was passively elevated to 90° in the scapular plane, and the patient was instructed to gradually control the relaxation of the elastic resistance while gradually lowering the arm to the 0° position [30].
Data were coded using the IBM SPSS Statistics version 28 (IBM Corp., Armonk, NY, USA). Data were summarized in the form of mean and standard deviation for quantitative variables. For categorical variables, frequencies (number of cases) and relative frequencies (percentages) were used.
Comparisons between groups were performed using unpaired t-tests for normally distributed quantitative variables. On the other hand, a non-parametric Mann–Whitney U-test was used for non-normally distributed quantitative variables. Comparing pre- and post-treatment in each group was conducted using paired t-tests in normally distributed quantitative variables. In contrast, the non-parametric Wilcoxon signed-rank test was used for nonnormally distributed quantitative variables. p-values less than 0.05 were considered statistically significant.
Forty adult patients with RA and rotator cuff tendinopathy were enrolled in the study and completed baseline and follow-up assessments. Each group consisted of 20 patients. Group 1 received concentric exercise sessions. At the same time, group 2 received eccentric exercise sessions.
Patients had a mean age of 44.43±5.39 years and a mean RA disease duration of 5.83±3.86 years. There was no statistically significant difference between the two groups regarding age, sex, disease duration, tendinopathy stage, or disease activity (Table 1).
There was a statistically significant decrease in SPADI scores post-treatment in both groups compared to baseline assessment (p<0.001; Table 2). There was no statistically significant difference between the two groups in SPADI scores at the baseline. However, there was a significant difference between the two groups post-treatment (p=0.007) in favor of group 2 (Table 2).
There was a statistically significant decrease in VAS scores post-treatment in both groups compared to baseline assessment (p<0.001; Table 2). There was no statistically significant difference between VAS scores at the baseline between both groups. However, there was a statistically significant difference between the two groups post-treatment (p=0.025), with a lower value in group 2 (Table 2).
There was no statistically significant change in supraspinatus tendon thickness post-treatment in either group. There was no statistically significant difference between the two groups, either at baseline or post-treatment.
There was a statistically significant increase in echo pixels of the supraspinatus tendon in the eccentric group only post-treatment compared to baseline (p=0.020). However, there was no statistically significant difference between the two groups either at baseline or post-treatment (Table 2).
There was a statistically significant decrease in subscapularis tendon thickness in the concentric exercise group only post-treatment compared to baseline (p=0.027). However, there was no difference between the two groups either at baseline or post-treatment (Table 2).
There was a significant increase in echo pixels of the subscapularis tendon in the concentric group only post-treatment compared to baseline (p=0.027). However, there was no difference between the two groups either at baseline or post-treatment (Table 2).
There was a statistically significant decrease in DAS-28-ESR scores post-treatment in both groups compared to baseline assessment (p<0.001; Table 2). However, there was no difference between the two groups either at baseline or post-treatment.
Rheumatoid affections of the shoulder joints frequently occur in patients with RA [9]. Patients with elderly-onset RA have large joint involvement and shoulder symptoms more often than those with younger-onset RA [31]. This was observed in this study, where the mean age was 44.43±5.39 years. Performing exercises effectively improves shoulder function and pain without adverse effects [13]. This study aimed to compare the efficacy of concentric vs. eccentric exercises for rotator cuff tendinopathy in patients with RA. Shoulder function, pain, tendon characteristics, and RA disease activity were assessed at baseline and after 12 sessions.
Exercise has proven its efficacy in restoring function in patients with rotator cuff tendinopathy. Literature has shown progressive loading exercises’ effectiveness in treating rotator cuff tendinopathy patients. Among the exercises used in treating patients with rotator cuff tendinopathy are concentric and eccentric exercises [32].
In this study, shoulder function measured by the SPADI and pain measured by the VAS improved in both groups. Besides, the improvement was greater than the MCID. Moreover, there was a significant improvement in shoulder function and pain in the eccentric group compared to the concentric group. Furthermore, the difference between the two groups was greater than the MCID.
This was in agreement with the results of Chaconas et al. [17] in 2017, which concluded that pain and function improved following the eccentric exercise group compared to the concentric group; however, their study included subacromial impingement patients. In contrast to our results, Blume et al. [33] in 2015, reported improvement in both groups; however, no difference between eccentric and concentric exercise in treating patients with subacromial impingement. However, they excluded any patients with rheumatic diseases. This could explain the difference in results compared to this study [33].
To the best of author’s knowledge, this is the first randomized clinical trial to compare concentric vs. eccentric exercises in patients with RA. Exercise improved the pain and function of shoulder tendinopathy in patients with RA, with better outcomes in the eccentric group. This agrees with many studies on non-RA patients that found an eccentric exercise more beneficial than a concentric exercise in improving pain, insulin sensitivity, glycemic control, blood lipid profile, and physical fitness in healthy people [14,34]. Furthermore, eccentric exercises are believed to restore tendon blood flow and thickness. In addition, eccentric exercises reduce edema and reverse painful neovascularization within injured tendons [14,35].
MSUS was used to evaluate shoulder tendinopathy and the efficacy of the exercise regimen in this study. This study showed no difference between the two groups regarding supraspinatus tendon or subscapularis tendon thickness at baseline or post-treatment. Furthermore, only the concentric group showed a decrease in tendon thickness of the subscapularis tendon post-treatment compared to baseline.
Tendon thickening may be the first pathological manifestation of tendinopathy. The thicker tendon will occupy a larger space within the subacromial space, thus, leading to tendon compression [22]. Therefore, tendon thickness can be a good indicator of tendinopathy. An increase in supraspinatus tendon thickness could be due to chronic tendinopathy induced by age-related degeneration [36]. Grigg et al. [37] in 2009, reported a more significant decrease in Achilles tendon thickness in healthy adults immediately after an eccentric exercise compared to a concentric exercise. However, they reported a recovery time frame similar to concentric exercises.
Echo pixels analysis evaluates the pixel-intensity distribution in the tendons, where echo pixels are inversely proportional to tendon affection. Compared to normal tendons, decreased echo pixels were observed in tendinopathy [38]. In this study, there was no significant difference between the two groups regarding supraspinatus and subscapularis echo pixels. However, there was an improvement in supraspinatus echo pixels in the eccentric group and subscapularis thickness and echo pixels in the concentric group post-treatment compared to baseline. This indicates the effectiveness of both types of exercise in improving tendon characteristics in patients with RA. Thus, concentric and eccentric exercises complement each other in treating rotator cuff tendinopathy.
However, there was no difference between the two groups regarding any tendon characteristics. The concentric exercise was beneficial in improving subscapularis tendon characteristics. At the same time, eccentric exercise improved supraspinatus tendon characteristics. This may be due to the different anatomical backgrounds, physiology, and mechanisms of action. The subscapularis muscle is the only rotator cuff muscle inserted in the lesser tuberosity and acts as an internal shoulder rotator. Supraspinatus, infraspinatus, and teres minor are inserted into the greater tubercle and act as external rotators or abductors [39]. The different attachments and actions may cause different responses to different exercise types.
The DAS-28-ESR indicates RA disease activity, with a higher score indicating higher disease activity [26,40]. This study showed that the DAS-28-ESR score decreased in both groups. However, there was no difference between the groups. This could imply that exercise effectively improves disease activity in patients with RA, regardless of the type of exercise.
This study has some limitations, such as the lack of a control group and the possibility that a longer duration of treatment may be needed before changes in tendon characteristics can be compared. Moreover, muscle power was not assessed. Furthermore, we included patients with subscapularis and supraspinatus tendinopathies. However, this was the first study comparing eccentric and concentric exercises in patients with RA. We recommend further studies with an extended exercise program on a large scale of patients and research involving the response of different rotator cuff tendons to different exercises. Additionally, we suggest a study involving a control group.
This study has concluded that eccentric exercise is more effective than concentric exercise in improving pain and function in rotator cuff tendinopathy in patients with RA. However, there was no difference between the types of exercises related to any of the MSUS findings.
AUTHOR CONTRIBUTION
Conceptualization: Wahba MM, Abdelsalam MS, Hegazy MM. Methodology: Wahba MM, Abdelsalam MS, Elgohary R, Selim M. Formal analysis: Wahba MM, Elgohary R, Abdelsalam MS. Project administration: Abdelsalam MS, Selim M. Visualization: Wahba MM, Selim M, Elgohary R, Hegazy MM. Writing – original draft: Wahba MM, Selim M. Writing – review and editing: Wahba MM, Abdelsalam MS, Selim M, Hegazy MM. Approval of final manuscript: all authors.
Fig. 2.
Internal and external rotation exercise (A) starting position for external rotation, (B) end position of external rotation, (C) starting position for internal rotation, and (D) end position of internal rotation.

Fig. 3.
Abductor strengthening (A) starting position for abduction and (B) end position of abduction.
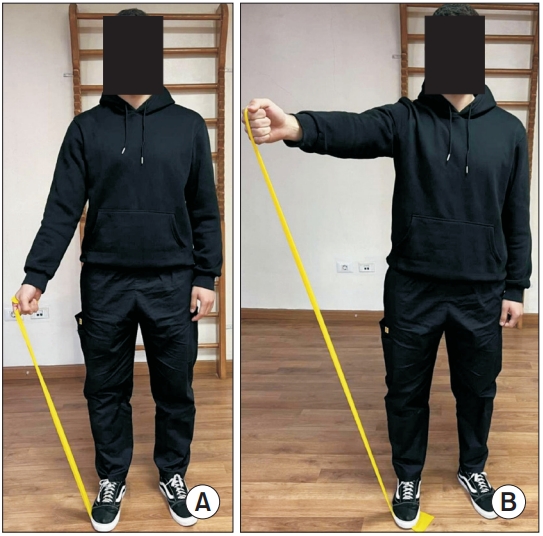
Table 1.
Patients characteristics
Table 2.
Comparison of SPADI, VAS, tendon characteristics, and DAS-28-ESR between and within groups
| Variable | Group | Baseline | Post | MD | p-value |
|---|---|---|---|---|---|
| SPADI (%) | Group 1 | 70.5±15.4 | 44.8±19.6 | 25.7 | <0.001*** |
| Group 2 | 63.2±17.0 | 28.5±16.6 | 34.7 | <0.001*** | |
| MD | 7.38 | 16.35 | - | - | |
| p-value | 0.159 | 0.007** | - | - | |
| VAS (cm) | Group 1 | 7.12±2.25 | 3.74±2.24 | 3.38 | <0.001*** |
| Group 2 | 6.61±2.20 | 2.30±1.61 | 4.31 | <0.001*** | |
| MD | 0.5 | 1.4 | - | - | |
| p-value | 0.159 | 0.025* | - | - | |
| Supraspinatus thickness (mm) | Group 1 | 4.79±1.08 | 4.99±1.27 | -0.195 | 0.215 |
| Group 2 | 4.46±0.86 | 4.52±0.96 | -0.060 | 0.648 | |
| MD | 0.33 | 0.46 | - | - | |
| p-value | 0.287 | 0.203 | - | - | |
| Supraspinatus echo pixels | Group 1 | 27,828.95±7,874.38 | 28,410.95±6,211.56 | -582.00 | 0.476 |
| Group 2 | 24,552.90±6,254.36 | 26,889.75±6,845.27 | -2,336.85 | 0.020* | |
| MD | 3,726.05 | 1,521.20 | - | - | |
| p-value | 0.153 | 0.466 | - | - | |
| Subscapularis thickness (mm) | Group 1 | 3.03±0.65 | 2.86±0.59 | 0.16 | 0.027* |
| Group 2 | 3.01±0.80 | 2.99±0.63 | 0.03 | 0.712 | |
| MD | 0.01 | -0.12 | - | - | |
| p-value | 0.966 | 0.532 | - | - | |
| Subscapularis echo pixels | Group 1 | 17,536.90±4,325.39 | 19,355.40±5,342.39 | -1,516.05 | 0.027* |
| Group 2 | 17,536.90±4,325.39 | 18,135.25±3,828.76 | -598.35 | 0.548 | |
| MD | 302.45 | 1,220.00 | - | - | |
| p-value | 0.838 | 0.412 | - | - | |
| DAS-28-ESR | Group 1 | 4.45±0.83 | 3.28±0.99 | 1.17 | <0.001*** |
| Group 2 | 4.88±0.77 | 3.38±1.00 | 1.49 | <0.001*** | |
| MD | -0.43 | -0.11 | - | - | |
| p-value | 0.099 | 0.736 | - | - |
REFERENCES
1. Zamanpoor M. The genetic pathogenesis, diagnosis and therapeutic insight of rheumatoid arthritis. Clin Genet 2019;95:547-57.



2. Hunter TM, Boytsov NN, Zhang X, Schroeder K, Michaud K, Araujo AB. Prevalence of rheumatoid arthritis in the United States adult population in healthcare claims databases, 2004-2014. Rheumatol Int 2017;37:1551-7.



3. Suzuki T, Ishihara K. Achilles paratendonitis as the initial manifestation of rheumatoid arthritis. Mod Rheumatol 2011;21:219-22.


4. Boutry N, Morel M, Flipo RM, Demondion X, Cotten A. Early rheumatoid arthritis: a review of MRI and sonographic findings. AJR Am J Roentgenol 2007;189:1502-9.


5. Hayer S, Redlich K, Korb A, Hermann S, Smolen J, Schett G. Tenosynovitis and osteoclast formation as the initial preclinical changes in a murine model of inflammatory arthritis. Arthritis Rheum 2007;56:79-88.


6. Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol 2004;33:73-81.


7. Rees JL. The pathogenesis and surgical treatment of tears of the rotator cuff. J Bone Joint Surg Br 2008;90:827-32.



8. Wang WT, Huang SW, Liou TH, Lin HW. Patients with rheumatoid arthritis were associated with a risk of rotator cuff diseases. J Clin Med 2019;8:129.



9. Bilberg A, Bremell T, Balogh I, Mannerkorpi K. Significantly impaired shoulder function in the first years of rheumatoid arthritis: a controlled study. Arthritis Res Ther 2015;17:261.



10. Lehtinen JT, Belt EA, Lybäck CO, Kauppi MJ, Kaarela K, Kautiainen HJ, et al. Subacromial space in the rheumatoid shoulder: a radiographic 15-year follow-up study of 148 shoulders. J Shoulder Elbow Surg 2000;9:183-7.


11. Chen AL, Joseph TN, Zuckerman JD. Rheumatoid arthritis of the shoulder. J Am Acad Orthop Surg 2003;11:12-24.


12. Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev 2009;2009:CD002759.



13. Lourenzi FM, Jones A, Pereira DF, Santos JHCAD, Furtado RNV, Natour J. Effectiveness of an overall progressive resistance strength program for improving the functional capacity of patients with rheumatoid arthritis: a randomized controlled trial. Clin Rehabil 2017;31:1482-91.



14. Larsson R, Bernhardsson S, Nordeman L. Effects of eccentric exercise in patients with subacromial impingement syndrome: a systematic review and meta-analysis. BMC Musculoskelet Disord 2019;20:446.




15. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 2010;69:1580-8. Erratum in: Ann Rheum Dis 2010;69:1892.
16. Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med 2009;43:409-16.


17. Chaconas EJ, Kolber MJ, Hanney WJ, Daugherty ML, Wilson SH, Sheets C. Shoulder external rotator eccentric training versus general shoulder exercise for subacromial pain syndrome: a randomized controlled trial. Int J Sports Phys Ther 2017;12:1121-33.



18. Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum 2009;61:623-32.


19. Alsanawi HA, Alghadir A, Anwer S, Roach KE, Alawaji A. Cross-cultural adaptation and psychometric properties of an Arabic version of the Shoulder Pain and Disability Index. Int J Rehabil Res 2015;38:270-5.


20. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008;31:165-9.


21. Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg 2009;18:927-32.


22. Michener LA, Subasi Yesilyaprak SS, Seitz AL, Timmons MK, Walsworth MK. Supraspinatus tendon and subacromial space parameters measured on ultrasonographic imaging in subacromial impingement syndrome. Knee Surg Sports Traumatol Arthrosc 2015;23:363-9.



23. Karthikeyan S, Rai SB, Parsons H, Drew S, Smith CD, Griffin DR. Ultrasound dimensions of the rotator cuff in young healthy adults. J Shoulder Elbow Surg 2014;23:1107-12.


24. Smith TO, Back T, Toms AP, Hing CB. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol 2011;66:1036-48.


25. Collinger JL, Gagnon D, Jacobson J, Impink BG, Boninger ML. Reliability of quantitative ultrasound measures of the biceps and supraspinatus tendons. Acad Radiol 2009;16:1424-32.



26. Anderson JK, Zimmerman L, Caplan L, Michaud K. Measures of rheumatoid arthritis disease activity: Patient (PtGA) and Provider (PrGA) Global Assessment of Disease Activity, Disease Activity Score (DAS) and Disease Activity Score with 28-Joint Counts (DAS28), Simplified Disease Activity Index (SDAI), Clinical Disease Activity Index (CDAI), Patient Activity Score (PAS) and Patient Activity Score-II (PASII), Routine Assessment of Patient Index Data (RAPID), Rheumatoid Arthritis Disease Activity Index (RADAI) and Rheumatoid Arthritis Disease Activity Index-5 (RADAI-5), Chronic Arthritis Systemic Index (CASI), Patient-Based Disease Activity Score With ESR (PDAS1) and Patient-Based Disease Activity Score without ESR (PDAS2), and Mean Overall Index for Rheumatoid Arthritis (MOI-RA). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S14-36.


27. Borstad JD, Ludewig PM. Comparison of three stretches for the pectoralis minor muscle. J Shoulder Elbow Surg 2006;15:324-30.


28. Moezy A, Sepehrifar S, Solaymani Dodaran M. The effects of scapular stabilization based exercise therapy on pain, posture, flexibility and shoulder mobility in patients with shoulder impingement syndrome: a controlled randomized clinical trial. Med J Islam Repub Iran 2014;28:87.


29. Kinsella R, Cowan SM, Watson L, Pizzari T. A comparison of isometric, isotonic concentric and isotonic eccentric exercises in the physiotherapy management of subacromial pain syndrome/rotator cuff tendinopathy: study protocol for a pilot randomised controlled trial. Pilot Feasibility Stud 2017;3:45.




30. Camci E, Duzgun I, Hayran M, Baltaci G, Karaduman A. Scapular kinematics during shoulder elevation performed with and without elastic resistance in men without shoulder pathologies. J Orthop Sports Phys Ther 2013;43:735-43.


31. El-Labban AS, Omar HA, El-Shereif RR, Ali F, ElMansoury TM. Pattern of young and old onset rheumatoid arthritis (YORA and EORA) among a group of Egyptian patients with rheumatoid arthritis. Clin Med Insights Arthritis Musculoskelet Disord 2010;3:25-31.




32. Desmeules F, Boudreault J, Dionne CE, Frémont P, Lowry V, MacDermid JC, et al. Efficacy of exercise therapy in workers with rotator cuff tendinopathy: a systematic review. J Occup Health 2016;58:389-403.




33. Blume C, Wang-Price S, Trudelle-Jackson E, Ortiz A. Comparison of eccentric and concentric exercise interventions in adults with subacromial impingement syndrome. Int J Sports Phys Ther 2015;10:441-55.


34. Chow BC, Li S, Zhu X, Jiao J, Quach B, Baker JS, et al. Effects of descending or ascending stair exercise on body composition, insulin sensitivity, and inflammatory markers in young Chinese women with obesity: a randomized controlled trial. J Sports Sci 2021;39:496-502.


35. Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology (Oxford) 2006;45:508-21.


36. Yu TY, Tsai WC, Cheng JW, Yang YM, Liang FC, Chen CH. The effects of aging on quantitative sonographic features of rotator cuff tendons. J Clin Ultrasound 2012;40:471-8.


37. Grigg NL, Wearing SC, Smeathers JE. Eccentric calf muscle exercise produces a greater acute reduction in Achilles tendon thickness than concentric exercise. Br J Sports Med 2009;43:280-3.


38. Chimenti RL, Flemister AS, Tome J, McMahon JM, Flannery MA, Xue Y, et al. Altered tendon characteristics and mechanical properties associated with insertional Achilles tendinopathy. J Orthop Sports Phys Ther 2014;44:680-9.


39. Kadi R, Milants A, Shahabpour M. Shoulder anatomy and normal variants. J Belg Soc Radiol 2017;101(Suppl 2): 3.



40. Wells G, Becker JC, Teng J, Dougados M, Schiff M, Smolen J, et al. Validation of the 28-joint Disease Activity Score (DAS28) and European League Against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann Rheum Dis 2009;68:954-60.












