- Search
| Ann Rehabil Med > Volume 46(3); 2022 > Article |
|
Abstract
Objective
To systematically review the available literature on the efficacy of tibial nerve stimulation on faecal incontinence and quality of life in adult patients with low anterior resection syndrome following surgery for colorectal cancer.
Methods
A primary search of electronic databases was conducted adopting a combination of search terms related to the following areas of interest: “efficacy”, “tibial nerve stimulation” and “low anterior resection syndrome”. A secondary search of the grey literature was performed in addition to checking the reference list of included studies and review papers. The review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. A descriptive analysis was used to integrate the review findings.
Results
Five distinct studies involving 116 patients met the inclusion criteria for the review. The included studies suggest that tibial nerve stimulation may have a positive effect on faecal incontinence and quality of life in some patients with low anterior resection syndrome and might be considered as an additional treatment option.
Conclusion
There were a limited number of studies and a great degree of heterogeneity of evidence due to differences in participants’ baseline characteristics, dropout rates, and follow-up periods. Further research adopting validated, consistent, and complex outcome assessment methods is recommended to determine the efficacy of tibial nerve stimulation for treatment of patients with low anterior resection syndrome.
Colorectal cancer is the third most prevalent cancer worldwide [1]. The widespread application of total mesorectal excision and multimodal therapy not only substantially improves its outcomes but also increases the feasibility of sphincter preservation and restoration of intestinal continuity [2]. Such sphincter-preserving surgeries help avoid permanent colostomy or ileostomy and account for approximately 80% of the procedures performed for colorectal cancer [3]. Nonetheless, up to 70% of patients who undergo anterior resection experience a form of bowel dysfunction, referred to as low anterior resection syndrome (LARS) [4]. This syndrome is characterized by a spectrum of symptoms, including fecal incontinence or urgency, stool clustering, incomplete evacuation, and fragmented defecation [2]. The symptoms of LARS have been deemed to be transient, mostly improving in the first year after surgery [5]. Long-term studies suggest that the symptoms of bowel dysfunction can present for up to 15 years after anterior resection, significantly deteriorating the patients’ quality of life and mental status [2,6,7].
Currently, there is no specific treatment for LARS, and its therapeutic management remains symptomatic. This includes administering medication for constipation, physiotherapy, transanal irrigation, biofeedback, and neuromodulation by sacral nerve stimulation [8-10]. Sacral nerve stimulation has been shown to have a direct influence on the anal sphincters and the ability to lessen antegrade colonic motor activity and strengthen retrograde activity [11]. Tibial nerve stimulation is a new, costeffective, and less invasive form of indirect neuromodulation of the sacral nerve function. The tibial nerve is a mixed sensory-motor nerve, including L4-S3 fibers that emanate from the same spinal segments as the nerves to the pelvic floor. Although the mechanism of tibial nerve stimulation is not fully defined, it is thought to induce multiple physiological effects. First, tibial nerve stimulation may enhance the baseline and stress pressure of the anal sphincters and improve rectal sensitivity by triggering multiple nerve pathways at the medullary and brain levels. Second, it causes alterations in the colonic motility and sphincter activity by triggering changes in local somato-visceral reflexes [12]. Third, tibial nerve stimulation might modulate a higher perception of afferent information, as the tibial nerve originates from the sacral roots. A limitation of the current academic literature is that there is very little unifying research on the efficacy of tibial nerve stimulation for the management of LARS [1]. Such a research gap compromises any attempts to justify the importance of tibial nerve stimulation and evaluate its impact on fecal incontinence and the patient’s quality of life.
Against this background, the current study aimed to systematically review the available literature on the efficacy of tibial nerve stimulation on fecal incontinence and quality of life in adult patients with LARS following surgery for colorectal cancer.
The protocol for this systematic review was registered in PROSPERO (CRD42021258925). This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13].
The following four electronic databases were searched: PubMed, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials on June 10, 2021. The search terms were developed with the assistance of information scientists following the PICOTS-SD guidelines. The search terms combined three overlapping areas with keywords, such as “efficacy” AND “tibial nerve stimulation” AND “low anterior resection syndrome” (see Supplement A and B for a full search strategy). Publication bias was diminished by searching conference records and unpublished literature using Google Scholar, OpenGrey, EThOS, and Copac. In addition, backward and forward citation tracking were applied to the included studies and review records.
Studies were eligible if they evaluated the efficacy of tibial nerve stimulation on fecal incontinence and/or quality of life in adult patients (>18 years old) with LARS following surgery for colorectal cancer. Both randomized controlled trials (RCTs) and non-randomized studies on intervention effects were included, from which a limited number of potentially eligible studies were expected. Studies were excluded if they met any one of the following criteria: (1) non-research-based articles, such as conference abstracts, commentaries, opinion pieces, book chapters, and editorials; (2) if the sample included patients under 18 years of age; (3) if the sample included patients with low anterior syndrome following surgery for any condition other than colorectal cancer; (4) case series with fewer than three cases; (5) any study that was not written using the Latin alphabet, Russian, or Kazakh; (6) an abstract was not available; or (7) the full text was not available.
The titles and abstracts of the identified records were exported to EndNote X8 reference management software and screened by the first reviewer (AT) to exclude irrelevant records and duplicates. A random subsample of 20% of the titles and abstracts was screened by AT and MT to ensure selection accuracy. Full-text articles were inspected again (by AT, AM, AB, and MD) for relevance according to the inclusion criteria. The level of agreement between AT and AM, AT and AB, and AT and MD was 70%, 75%, and 65%, respectively. Discrepancies were resolved by involving AS.
The data from each study, including the study details, participant demographics, and key results on fecal incontinence and quality of life, were extracted into a spreadsheet by the first reviewer (AT). Subsequently, AM, AB, and AS ensured accuracy at this stage by independently extracting data from all the included studies.
The methodological quality was assessed using the Quality Assessment of Controlled Intervention Studies [14] for any randomized controlled trial and the Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group [15] for any prospective non-randomized studies developed by the National Heart, Lung, and Blood Institute.
The primary outcome was the efficacy of tibial nerve stimulation on fecal incontinence measured by the LARS score and Wexner score. Although the LARS score was provided in all the included studies, the reported data differed considerably, limiting the opportunities for a meta-analysis. Therefore, owing to the limited number of eligible studies and their heterogeneity, no specific outcome measures were analyzed, and a descriptiveanalytical method was used for the current review.
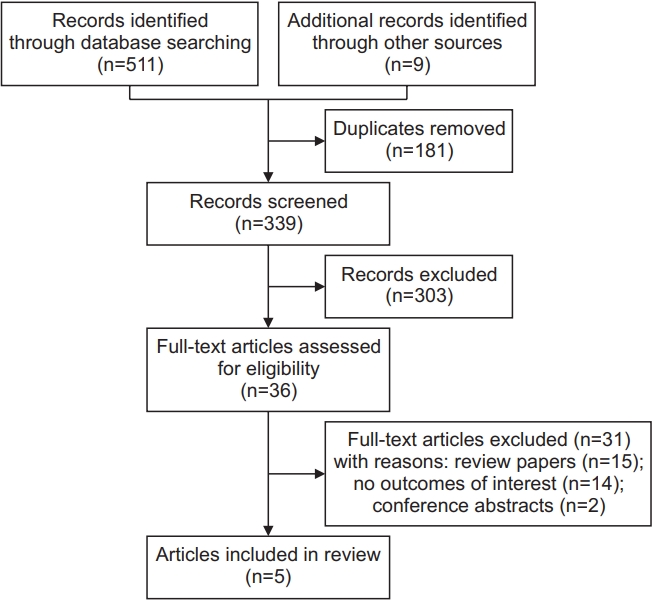
The original search yielded 511 records through database searches and nine records from other sources. A total of 181 records were excluded as duplicates, and 303 records were removed because they did not meet the eligibility criteria. The full texts of the remaining 36 articles were examined, five of which were included and represented five distinct studies. The detailed selection process is presented in a PRISMA flow diagram (Fig. 1).
The included studies were published between 2017 and 2021 and were conducted in Spain [16-18] and Italy [19], while one study was multi-centered [20]. Regarding the study design, two of the included studies were prospective non-randomized studies [16,20], and three studies were RCTs [17-19]. All included studies employed an identical tibial nerve stimulation technique in which a needle was placed at the percutaneous or posterior tibial nerve without anesthesia; additionally, the stimulation parameters were set to a 200 μs pulse width and a frequency of 20 Hz. Stimulation was gradually increased until sensory and/or motor responses were observed and set at a well-tolerated intensity.
With regard to the outcome measures, the LARS score [21] was adopted to assess the bowel function after anterior rectal resection for colorectal cancer in all the included studies. Additionally, to assess the frequency, type, and severity of fecal incontinence, the obstructed defecation syndrome (ODS) score [22] was employed in three studies [17,19,20], the St. Mark Fecal Incontinence score [23] was used in two studies [18,20], and the Wexner score [24] and the Fecal Incontinence Severity Index (FISI) [25] were adopted in one study each [16,19]. The impact of fecal incontinence on the patient quality of life was evaluated using the Fecal Incontinence Quality of Life (FIQL) score in three studies [16,19,20] and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire [26] in three other studies [17-19].
The results of this review are presented in two parts. In the first part, prospective non-randomized studies included in the review are introduced. In the second part, the findings of the included RCTs are presented.
Two prospective non-randomized studies [16,20] involved 31 patients with LARS after surgery for colorectal cancer. In both studies, the patients were included after the failure of conservative treatment (diet, medical treatment, biofeedback, or bulking agents). Additionally, approximately half of the patients underwent preoperative and postoperative chemo/radiotherapy. Tibial nerve stimulation was administered during 12 sessions [20] and 18 sessions [16] of 30 minutes of stimulation each, with follow-up periods of 6 months [20] and 3 weeks [16], respectively.
In the study conducted by Altomare et al. [20], the patients reported a significant improvement in LARS and St. Mark Fecal Incontinence scores, while obstructed defecation improved in only three patients and did not indicate a significant change in the ODS score from baseline to follow-up. In a study conducted by Vigorita et al. [16], tibial nerve stimulation was administered in two phases. In the first phase, all the patients received stimulation, whereas only those who experienced an improvement were included in the second phase. After the first phase, seven of 10 patients responded positively to treatment, which reflected a significant improvement in LARS and Wexner scores over baseline. These seven patients received the second phase of treatment, five of whom reported an improvement in LARS symptoms. No significant improvement in the LARS score was detected after the second phase due to the small number of patients included. Altomare et al. [20] did not observe any significant changes in the FIQL scores, whereas Vigorita et al. [16] reported significant improvements in the lifestyle, coping/behavior, and depression domains of the scale after the first phase of the study. The characteristics of the included prospective non-randomized studies are summarized in Tables 1 and 2.
Three RCTs involved 85 patients with LARS following surgery for colorectal cancer. All the studies were intervention-controlled and used transanal irrigation [17], medical treatment [19], and sham therapy [18] as alternative treatment methods. One study was open [17], whereas single-blinding [19] and double-blinding [18] were adopted in a single trial. Tibial nerve stimulation was administered during 20 sessions [17], 17 sessions [19], and 16 sessions [18] of 30 minutes of stimulation each, with follow-up periods of 6 months [17] and 12 months [18,19], respectively.
Enriquez-Navascues et al. [17] reported that although LARS scores significantly decreased in both the intervention and control groups, the number of patients transferred from the “major LARS” category to the “no LARS” category was higher in the control group (eight out of 10 patients) than in the intervention group (three out of 13 patients). In two other studies [18,19], the LARS score improved significantly in patients who received tibial nerve stimulation, whereas no significant change from baseline to follow-up was observed in the control group. Enriquez-Navascues et al. [17] described no significant improvements in the ODS score in either arm, whereas Cuicchi et al. [19] described a significant decline in the intervention arm compared to the control arm. Furthermore, a significant reduction in the FISI and St. Mark Fecal Incontinence scores in the intervention arm were observed in each trial [18,19]. Although improvements in the quality of life indicators in both the intervention and control groups were described, none of the included trials indicated these changes to be statistically significant. The overall characteristics of the included RCTs are summarized in Tables 3 and 4.
On the Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group, both the included prospective non-randomized studies were rated as fair [16,20]. In the Quality Assessment of Controlled Intervention Studies, one study was rated as poor [17] and two as fair [18,19]. A complete risk of bias assessment is presented in Supplement C.
The current study aimed to systematically review the available literature on the efficacy of tibial nerve stimulation on fecal incontinence and quality of life in adult patients with LARS following surgery for colorectal cancer. The results from five distinct studies suggest that percutaneous or posterior tibial nerve stimulation may have a positive effect on fecal incontinence and quality of life in some patients with LARS and thus might be considered as an additional treatment option. However, the conclusions are tentative for the following reasons: First, the included studies reported relatively short follow-up periods ranging from 6 to 12 months, making changes in fecal incontinence and quality of life scores somewhat questionable. The available literature suggests that the severity of LARS symptoms may diminish within 2 years of surgery [1]. Therefore, studies with a shorter follow-up period should be considered with caution, as some clinical improvements might be either missed or observed regardless of treatment. Second, the eligible studies included a small number of participants, making it difficult to detect any within-group effects. Third, the influence of different confounding variables, including the type and level of anastomosis and the role of comorbidities, self-management, and social support, has been barely explored.
A recent meta-analysis estimated that approximately 65% of patients suffer from LARS after oncological rectal resection, and 45% experience major symptoms [27]. Although different treatment options are used, there is no evidence of an intervention that can help manage the symptoms of this syndrome. According to a systematic review of pelvic floor rehabilitation, pelvic floor training might be a useful method for improving the functional outcomes following low anterior resection [28]. Meanwhile, other authors admit that this rehabilitative technique is unlikely to address a low resting tone and neorectal hypersensitivity, which are common in the postoperative period [20]. Another systematic review reported a promising success rate of 74% with sacral nerve stimulation for LARS [29]. Although this improvement is similar to its use for treating other forms of fecal incontinence [29], the high cost of the procedure limits its wider application. Based on the findings of the current review, tibial nerve stimulation resulted in a moderate improvement in the symptoms of LARS. However, the overall results did not demonstrate any evident improvement in fecal incontinence and quality of life, as reported after sacral nerve stimulation [30]or sham therapy [31,32].
To our knowledge, this is the first systematic review of the available literature on the efficacy of tibial nerve stimulation on fecal incontinence and quality of life in adult patients with LARS following surgery for colorectal cancer. Another strength is that the review employed a comprehensive and reproducible search strategy without limitations regarding the year of publication, language, or country of origin of any studies considered. However, this approach has several limitations. First, owing to the limited number of included studies and their heterogeneity, it was not feasible to conduct a meta-analysis; therefore, the final interpretation was made using descriptiveanalytical procedures. Second, the exclusive adoption of scoring systems to assess improvements in fecal incontinence and quality of life may have left some of the positive clinical outcomes unnoticed. Third, the comparability of findings across the included studies may be limited because of the wide variability in participants’ baseline characteristics and dropout rates.
To navigate the practical implications, future research should address several research gaps. First, further evidence regarding the mechanism of action of tibial nerve stimulation on the symptoms of LARS is needed. Second, future studies may need to ensure adequate assessment of outcome measures by adopting a set of different methods, including recommendations of the existing literature and validated scoring systems, thorough clinical examination, and evaluation of bowel diaries. Third, there is a need to assess the efficacy of different timing and modalities of tibial nerve stimulation delivery. Finally, the potential adverse effects of tibial nerve stimulation should be further explored.
In conclusion, this systematic review provides evidence for the effectiveness of tibial nerve stimulation on fecal incontinence and quality of life in some patients with LARS. Considering the high heterogeneity and limited quality of the included studies, our conclusions are somewhat tentative. There is a need for large prospective randomized controlled trials adopting validated, consistent, and complex assessment methods to determine the efficacy of tibial nerve stimulation in treating patients with LARS.
AUTHOR CONTRIBUTION
Conceptualization: AT, AS. Methodology: AS. Formal analysis: AT. Project Administration: AT, AS, AM, AB. Visualization: AB, MD, MT. Writing – original draft: AT. Writing – review and editing: AS, AM. Administrative support: AM, AB, MD, MT. Approval of the final manuscript: all authors.
Table 1.
Characteristics of included prospective studies
| Altomare et al. [20] | Vigorita et al. [16] | |
|---|---|---|
| Country | Multi-centered (Italy and Spain) | Spain |
| Study design | Prospective | Prospective |
| Sampling | Convenience | Not reported |
| Total number of patients | 21 | 10 |
| Male | 10 (47.6) | 6 (60.0) |
| Female | 11 (52.4) | 4 (40.0) |
| Age (yr) | 66±5.8 | 62 (51.75–51.72) |
| Cancer stage | ||
| Stage I | 10 (47.6) | Not reported |
| Stage II | 6 (28.6) | Not reported |
| Stage III | 5 (23.8) | Not reported |
| Surgical procedure | ||
| Laparotomy | 15 (71.4) | Not reported |
| Laparoscopy | 6 (28.6) | Not reported |
| Preoperative chemo/radiotherapy | 10 (47.6) | 5 (50.0) |
| Postoperative chemo/radiotherapy | 13 (61.9) | 5 (50.0) |
| Number of withdrawals | None | 3 (30.0) after Phase 1 |
| Type of treatment | Percutaneous tibial nerve stimulation | Posterior tibial nerve stimulation |
| Treatment period | 12 sessions (2 per week for the first 4 weeks and 1 per week for the last 4 weeks) of 30 minutes stimulation. | Phase 1: 12 sessions (2 per week for 6 weeks) of 30 minutes stimulation. |
| Phase 2: 6 sessions (single weekly sessions for 6 weeks) of 30 minutes stimulation. | ||
| Treatment technique | Stimulation parameters were set at 200 μs pulse width and 20 Hz frequency. Stimulation was gradually increased until sensory and/or motor response were seen and set at a well-tolerated intensity. | Stimulation parameters were set at 200 μs pulse width and 20 Hz frequency. Stimulation was gradually increased until sensory and/or motor response were seen and set at a well-tolerated intensity. |
| Follow-up period | 6 months | 3 weeks after Phase 1 |
Table 2.
Outcome measures of included prospective studies
|
Altomare et al. [20] |
Vigorita et al. [16] |
|||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | p-value | Baseline | Follow-up | p-value | |
| LARS score | 32 (30–38) | 27 (17–37) | * | 35.5 (25–39) | 23 (21–34) | * |
| Wexner score | N/A | N/A | 14 (10.75–18.5) | 10 (6.5–18) | * | |
| ODS score | 9 (7–11) | 8 (6.5–10) | ns | N/A | N/A | |
| St. Mark Fecal Incontinence score | 18 (11–19) | 13 (11–18) | * | N/A | N/A | |
| FIQL score | ||||||
| Lifestyle | 2.7 (not reported) | 2.8 (not reported) | ns | 2.25 (1.3–2.38) | 3.48 (1.48–3.8) | * |
| Coping/behavior | 1.6 (not reported) | 1.4 (not reported) | ns | 1.72 (1.17–2.45) | 2.83 (1.86–4) | * |
| Depression | 1.7 (not reported) | 1.9 (not reported) | ns | 2.46 (1.48–2.6) | 3.3 (2.55–4) | * |
| Embarrassment | 1 (not reported) | 1.3 (not reported) | ns | 1.66 (1.25–3.17) | 2.67 (2.06–3.75) | ns |
Table 3.
Characteristics of included RCTs
| Enriquez-Navascues et al. [17] | Cuicchi et al. [19] | Marinello et al. [18] | ||
|---|---|---|---|---|
| Country | Spain | Italy | Spain | |
| Study design | RCT (open, transanal irrigation controlled) | RCT (pilot, single-blind, medical treatment controlled) | RCT (double-blind, sham therapy controlled) | |
| Total number of patients | 27 | 12 | 46 | |
| Male | 17 (63) | 7 (58.3) | 27 (58.7) | |
| Female | 10 (37) | 5 (41.7) | 19 (42.3) | |
| Arms | ||||
| Intervention arm | 14 (51.8) | 6 (50.0) | 23 (50.0) | |
| Control arm | 13 (48.2) | 6 (50.0) | 23 (50.0) | |
| Age (yr) | ||||
| Intervention arm | 68 (56–76) | 62.5 (50–75) | Not reported | |
| Control arm | 68 (48–71) | 71.5 (56–79) | Not reported | |
| Number of withdrawals | ||||
| Intervention arm | 1 (7.1) | None | 4 (17.4) | |
| Control arm | 3 (23.1) | None | 9 (39.1) | |
| Preoperative chemo/radiotherapy | ||||
| Intervention arm | 8 (57) | 6 (100) | 21 (91.3) | |
| Control arm | 9 (69) | 6 (100) | 19 (82.6) | |
| Type of treatment | ||||
| Intervention arm | 20 sessions of 30 minutes stimulation each (once a week for 12 consecutive weeks, followed by 4 additional sessions once a fortnight for the following 2 months and 4 further sessions once a month). | 17 sessions of 30 minutes stimulation each (once a week for 12 consecutive weeks, followed by 2 fortnightly sessions, 1 session a month later and 2 sessions at intervals of 6 months). | 16 sessions of 30 minutes stimulation each (once a week for 12 consecutive weeks followed by 4 additional sessions once a fortnight for the following 4 weeks). | |
| Control arm | Initially once a day then three to four times a week for a period of up to 6 months. | - | - | |
| Treatment technique | ||||
| Intervention arm | Stimulation parameters were set at 200 μs pulse width and 20 Hz frequency. | Stimulation parameters were set at 200 μs pulse width and 20 Hz frequency. | Stimulation parameters were set at 200 μs pulse width and 20 Hz frequency. | |
| Control arm | Peristeen system | Depending on the predominant symptom. In the case of faecal incontinence, urgency, or fractional defecation, the therapies were kaolin (1 sachet a day) or loperamide (1 tablet a day) and pelvic floor physical therapy. If the prevailing symptom was obstructed defecation, it was recommended to take osmotic laxatives or fiber (Psyllo). | Sham procedure | |
| Follow-up period (mo) | 6 | 12 | 12 | |
Table 4.
Outcome measures of included RCTs
|
Enriquez-Navascues et al. [17] |
Cuicchi et al. [19] |
Marinello et al. [18] |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | p-value | Baseline | Follow-upa) | p-value | Baseline | Follow-up | p-value | |||
| LARS score | |||||||||||
| Intervention arm | 35 (34–37) | 30 (25–33) | * | 35.8±6.2 | 28.2±9.5 | * | 36.4±3.9 | 30.7±11.5 | 0.018 | ||
| Control arm | 35 (32–39) | 12 (12–26) | * | 33.2±5.3 | 31.8±5.2 | ns | 36.3±3.2 | 33.9±6.6 | 0.209 | ||
| ODS score | |||||||||||
| Intervention arm | 9 (7–12) | 8 (4–9) | ns | 10.3±3.9 | 8.0±4.9 | ** | N/A | N/A | |||
| Control arm | 10 (7–14) | 8 (6–9) | ns | 7.2±1.2 | 6.8±1.2 | ns | N/A | N/A | |||
| St. Mark Fecal Incontinence score | |||||||||||
| Intervention arm | N/A | N/A | N/A | N/A | 15.4±5.2 | 12.5±6.4 | * | ||||
| Control arm | N/A | N/A | N/A | N/A | 15.4±5.3 | 15.7±5.9 | ns | ||||
| EORTC QLQ-C30 score | |||||||||||
| Global health status | |||||||||||
| Intervention arm | 9 (7–10) | 12 (9–12) | ns | 66.7±19.0 | 76.4±18.6 | ns | 42.8±28.3 | 41.2±27.8 | ns | ||
| Control arm | 8 (8–9) | 12 (9–12) | * | 48.6±6.2 | 45.8±7.0 | ns | 45.2±25.2 | 43.4±23.4 | ns | ||
| Physical functioning | |||||||||||
| Intervention arm | 33 (27-40) | 28 (23–31) | ns | Not reported | Not reported | 90.0±3.6 | 90.6±3.9 | ns | |||
| Control arm | 35 (28–43) | 28 (26–34) | ns | Not reported | Not reported | 88.6±4.5 | 89.2±5.5 | ns | |||
| Role functioning | |||||||||||
| Intervention arm | 7 (7–8) | 7 (7–8) | ns | Not reported | Not reported | 66.3±15.1 | 68.9±16.4 | ns | |||
| Control arm | 8 (7–8) | 7 (7–7) | ns | Not reported | Not reported | 65.6±16.1 | 65.5±16.9 | ns | |||
| Emotional functioning | |||||||||||
| Intervention arm | Not reported | Not reported | Not reported | Not reported | 85.1±5.4 | 85.8±4.5 | ns | ||||
| Control arm | Not reported | Not reported | Not reported | Not reported | 83.8±7.0 | 83.0±6.0 | ns | ||||
| FIQL score | |||||||||||
| Lifestyle | |||||||||||
| Intervention arm | N/A | N/A | 2.9±0.3 | 3.3±0.7 | ns | N/A | N/A | ||||
| Control arm | N/A | N/A | 2.9±1.1 | 2.8±1.0 | ns | N/A | N/A | ||||
| Coping/behavior | |||||||||||
| Intervention arm | N/A | N/A | 2.6±0.5 | 3.0±0.9 | ns | N/A | N/A | ||||
| Control arm | N/A | N/A | 2.7±0.9 | 2.7±0.9 | ns | N/A | N/A | ||||
| Depression | |||||||||||
| Intervention arm | N/A | N/A | 3.2±0.8 | 3.7±0.5 | ns | N/A | N/A | ||||
| Control arm | N/A | N/A | 3.5±0.7 | 3.4±0.7 | ns | N/A | N/A | ||||
| Embarrassment | |||||||||||
| Intervention arm | N/A | N/A | 2.7±0.4 | 3.7±0.5 | * | N/A | N/A | ||||
| Control arm | N/A | N/A | 2.9±0.9 | 2.9±0.9 | ns | N/A | N/A | ||||
Values are presented as number (%) or median (interquartile range).
RCT, randomized controlled trial; LARS, low anterior resection syndrome; ODS, obstructed defecation syndrome; EORTC QLQ-C30, European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30; FIQL, Fecal Incontinence Quality of Life; N/A, not applicable; ns, not significant.
REFERENCES
1. Bulfone G, Del Negro F, Del Medico E, Cadorin L, Bressan V, Stevanin S. Rehabilitation strategies for low anterior resection syndrome: a systematic review. Ann Ist Super Sanita 2020;56:38-47.

2. Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL. Anterior resection syndrome. Lancet Oncol 2012;13:e403. -8.


3. Dulskas A, Smolskas E, Kildusiene I, Samalavicius NE. Treatment possibilities for low anterior resection syndrome: a review of the literature. Int J Colorectal Dis 2018;33:251-60.



4. Emmertsen KJ, Laurberg S. Bowel dysfunction after treatment for rectal cancer. Acta Oncol 2008;47:994-1003.


5. Camilleri-Brennan J, Steele RJ. Prospective analysis of quality of life and survival following mesorectal excision for rectal cancer. Br J Surg 2001;88:1617-22.



6. van Duijvendijk P, Slors JF, Taat CW, van Tets WF, van Tienhoven G, Obertop H, et al. Prospective evaluation of anorectal function after total mesorectal excision for rectal carcinoma with or without preoperative radiotherapy. Am J Gastroenterol 2002;97:2282-9.


7. Pieniowski EH, Palmer GJ, Juul T, Lagergren P, Johar A, Emmertsen KJ, et al. Low anterior resection syndrome and quality of life after sphincter-sparing rectal cancer surgery: a long-term longitudinal follow-up. Dis Colon Rectum 2019;62:14-20.


9. Norton C, Chelvanayagam S, Wilson-Barnett J, Redfern S, Kamm MA. Randomized controlled trial of biofeedback for fecal incontinence. Gastroenterology 2003;125:1320-9.


10. Maeda Y, Matzel K, Lundby L, Buntzen S, Laurberg S. Postoperative issues of sacral nerve stimulation for fecal incontinence and constipation: a systematic literature review and treatment guideline. Dis Colon Rectum 2011;54:1443-60.


11. Michelsen HB, Christensen P, Krogh K, Rosenkilde M, Buntzen S, Theil J, et al. Sacral nerve stimulation for faecal incontinence alters colorectal transport. Br J Surg 2008;95:779-84.



12. Giani I, Novelli E, Martina S, Clerico G, Luc AR, Trompetto M, et al. The effect of sacral nerve modulation on cerebral evoked potential latency in fecal incontinence and constipation. Ann Surg 2011;254:90-6.


13. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097.



14. National Health, Lung, and Blood Institute. Study Quality Assessment Tools: Quality Assessment of Controlled Intervention Studies [Internet]. Bethesda, MD, National Health, Lung, and Blood Institute. 2021;[cited 2022 May 30]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
15. National Health, Lung, and Blood Institute. Study Quality Assessment Tools: Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group [Internet]. Bethesda, MD, National Health, Lung, and Blood Institute. 2021;[cited 2022 May 30]. Available from: https://www.nhlbi.nih.gov/healthtopics/study-quality-assessment-tools.
16. Vigorita V, Rausei S, Troncoso Pereira P, Trostchansky I, Ruano Poblador A, Moncada Iribarren E, et al. A pilot study assessing the efficacy of posterior tibial nerve stimulation in the treatment of low anterior resection syndrome. Tech Coloproctol 2017;21:287-93.



17. Enriquez-Navascues JM, Labaka-Arteaga I, Aguirre-Allende I, Artola-Etxeberria M, Saralegui-Ansorena Y, Elorza-Echaniz G, et al. A randomized trial comparing transanal irrigation and percutaneous tibial nerve stimulation in the management of low anterior resection syndrome. Colorectal Dis 2020;22:303-9.



18. Marinello FG, Jimenez LM, Talavera E, Fraccalvieri D, Alberti P, Ostiz F, et al. Percutaneous tibial nerve stimulation in patients with severe low anterior resection syndrome: randomized clinical trial. Br J Surg 2021;108:380-7.



19. Cuicchi D, Di Fabio F, Guido A, Llimpe FL, Morganti AG, Ardizzoni A, et al. Randomized pilot trial of percutaneous posterior tibial nerve stimulation versus medical therapy for the treatment of low anterior resection syndrome: one-year follow-up. Dis Colon Rectum 2020;63:1602-9.


20. Altomare DF, Picciariello A, Ferrara C, Digennaro R, Ribas Y, De Fazio M. Short-term outcome of percutaneous tibial nerve stimulation for low anterior resection syndrome: results of a pilot study. Colorectal Dis 2017;19:851-6.



21. Emmertsen KJ, Laurberg S. Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 2012;255:922-8.

22. Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V. Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis 2008;10:84-8.


23. Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut 1999;44:77-80.



24. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum 1993;36:77-97.


25. Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, et al. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum 1999;42:1525-32.

26. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-76.


27. Croese AD, Lonie JM, Trollope AF, Vangaveti VN, Ho YH. A meta-analysis of the prevalence of Low Anterior Resection Syndrome and systematic review of risk factors. Int J Surg 2018;56:234-41.


28. Visser WS, Te Riele WW, Boerma D, van Ramshorst B, van Westreenen HL. Pelvic floor rehabilitation to improve functional outcome after a low anterior resection: a systematic review. Ann Coloproctol 2014;30:109-14.



29. Ramage L, Qiu S, Kontovounisios C, Tekkis P, Rasheed S, Tan E. A systematic review of sacral nerve stimulation for low anterior resection syndrome. Colorectal Dis 2015;17:762-71.


30. de Miguel M, Oteiza F, Ciga MA, Armendariz P, Marzo J, Ortiz H. Sacral nerve stimulation for the treatment of faecal incontinence following low anterior resection for rectal cancer. Colorectal Dis 2011;13:72-7.


31. Leroi AM, Siproudhis L, Etienney I, Damon H, Zerbib F, Amarenco G, et al. Transcutaneous electrical tibial nerve stimulation in the treatment of fecal incontinence: a randomized trial (CONSORT 1a). Am J Gastroenterol 2012;107:1888-96.



32. Knowles CH, Horrocks EJ, Bremner SA, Stevens N, Norton C, O’Connell PR, et al. Percutaneous tibial nerve stimulation versus sham electrical stimulation for the treatment of faecal incontinence in adults (CONFIDeNT): a double-blind, multicentre, pragmatic, parallel-group, randomised controlled trial. Lancet 2015;386:1640-8.