- Search
| Ann Rehabil Med > Volume 35(4); 2011 > Article |
Abstract
Objective
To determine if an early regular cardiac rehabilitation program would have an adverse effect on myocardial function after acute myocardial infarction (AMI).
Method
Patients who received percutaneous coronary intervention (PCI) after AMI were divided into the exercise group and control group in accordance with their willingness to participate. Patients in the exercise group (n=18) received ECG monitored exercise for six weeks and were instructed to maintain self exercise in their communities for four months. The control group (n=16) patients were just instructed of risk factor control. All the subjects underwent echocardiography at the time of the AMI as well as six months later. The echocardiography parameters, including the left ventricular ejection fraction (LVEF), stroke volume (SV), left ventricular end-diastolic diameter (LVEDD) and end-systolic diameter (LVESD), were measured.
Cardiac rehabilitation is known to improve motor recovery of patients quickly and reduce recurrence, reperfusion, and death rate for mid- and long-term patients with acute myocardial infarction (AMI).1-4 However, because of concern that exercise of AMI patients may adversely affect myocardial remodeling, regular cardiac rehabilitation program begins to be applied three or four, or even six to eight weeks after onset. Gaudron et al.5 reported that, in a follow-up observation of 70 patients diagnosed with AMI from the fourth day of onset for three years, 14 (20%) showed widening in diameter of the left ventricle, a phenomenon that may ultimately cause severe left ventricular failure. Jugdutt et al.6 reported that 12-week cardiac rehabilitation exercise on 13 patients with AMI of around 16 weeks after onset showed reduction in motility of the myocardial wall and left ventricular ejection fraction (LVEF) in echocardiography. On the other hand, many later studies report that a cardiac rehabilitation program may not have adverse effects on myocardial remodeling after AMI. Dubach et al.7 reported that one-hour daily cardiac rehabilitation exercise for two months on patients with AMI of around 35 days after onset did not induce adverse changes in left ventricular end diastolic diameter (LVEDD), left ventricular end systolic diameter (LVESD), left ventricular ejection fraction, and wall thickness of infracted area in magnetic resonance imaging (MRI). Cannistra et al.8 reported that cardiac rehabilitation training did not have adverse effects on myocardial remodeling in echocardiography when 12-week cardiac rehabilitation training was conducted for 68 patients who were three months (mean 8.3┬▒4.8 weeks) after the first diagnosis of AMI. Recently, cardiac rehabilitation exercise was conducted earlier than before because duration of admission for AMI has dramatically reduced and many patients return to their daily life immediately after early discharge.9
In this context, the authors in this study investigated the effects of regular cardiac rehabilitation program on myocardial remodeling that began from the 14th day (mean) after AMI onset by reviewing the results of echocardiography.
The subjects of this study were patients with AMI who entered the Cardiac Vascular Center of this hospital to undergo percutaneous coronary intervention (PCI). Those who already had cardiovascular, systemic inflammatory, and nervous musculoskeletal diseases and may cause inconvenience in the exercise program were excluded from this study.
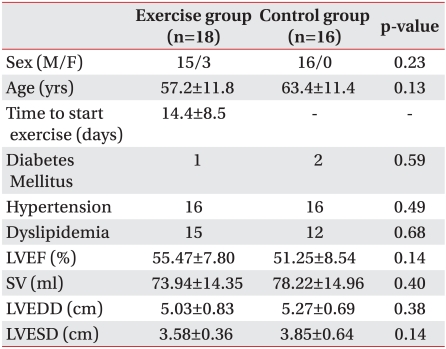
The eighteen patients in the exercise group included fifteen males and three females with 57.2┬▒11.8 years old. It took 14.4┬▒8.5 days between the onset of AMI and the beginning of the cardiac rehabilitation program. The control group included sixteen patients (all males) that were 63.4┬▒11.4 years old. There were no significant differences between the two groups in sex, age, diabetes, high blood pressure, and dyslipidemia (Table 1).
The patients were induced to participate in the cardiac rehabilitation program by sufficient in-advance education on necessity and contents of the program, and those who decided to participate in the program were classified into the exercise group and those who did not into the control group (non-exercise group).
The patients in the exercise group visited the outpatient cardiac rehabilitation clinic at the 10th day (mean) of the onset to undergo in-advance tests such as graded exercise test (GXT) and began a regular cardiac rehabilitation program in the hospital from the 14th day (mean) of the onset. For the GXT, a symptom limited method was used by modified Bruce protocol. In order to assess changes in cardiopulmonary motor ability in the GXT, indicators were measured such as maximal oxygen consumption (VO2max), maximal rate pressure product (RPPmax), submaximal rate pressure product at stage 3 (RPPIII), submaximal rate of perceived exertion at stage 3 (RPEIII), resting and maximal heart rate (HRrest & HRmax), and resting systolic and diastolic blood pressure (SBPrest & DBPrest).
Based on the resting and maximal heart rate of each patient obtained by the GXT, heart rate reserve was calculated and target heart rate was set up between 40% and 85% of the reserve as exercise intensity, which was increased gradually. The subjects were asked to participate in one-hour monitoring exercise, which consisted of 10 minutes of warm-up, 40 minutes of main exercise, and 10 minutes of cool-down in the hospital three times per week for a total six to eight weeks (or 18 to 24 sessions). After the six-to-eight week exercise program in the hospital, they were instructed to maintain self exercise in their communities until the sixth month after the onset based on their exercise prescription. The patients in the exercise group underwent echocardiography immediately before the exercise program, after six to eight weeks of the performance, and six months later, and underwent GXT immediately before the exercise program and six months later. The echocardiography was conducted by a cardiologist, measuring left ventricular ejection fraction (LVEF), stroke volume (SV), left ventricular end diastolic diameter (LVEDD), and left ventricular end systolic diameter (LVESD). The subjects were prescribed drugs and were under medical follow-up observation until approximately six months after the onset as outpatients.
Meanwhile, the control group that did not participate in the cardiac rehabilitation program underwent basic education on management of risk factors after AMI, but was instructed to do the management and exercise themselves. The subjects in the control group were prescribed drugs and were under follow-up observation until approximately six months after the onset as outpatients of cardiology, and underwent echocardiography immediately after the onset as well as six months later.
The differences in the LVEF, SV, LVEDD, and LVESD of the exercise group and the control groups measured at the early part and six months later in order to assess adverse myocardial remodeling based on the cardiac rehabilitation program from the 14th day (mean) were compared and analyzed by independent samples t-test. The differences in the indicators of the GXT measured at the early part and six months later in order to assess changes in cardiopulmonary motor ability of the exercise group were compared and analyzed by paired samples t-test. For statistical significance level, p-value was less than 0.05.
According to the results of early echocardiography conducted at the onsets of AMI, no significant difference was shown in the LVEF between the exercise group (55.47┬▒7.80%) and the control group (51.25┬▒8.54%). Also, there were no significant differences in the SV, LVEDD, and LVESD between the two groups (Table 1).
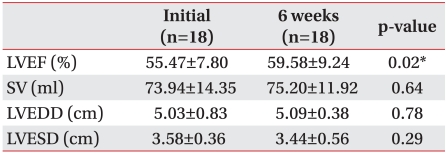
The LVEF significantly increased from 55.47┬▒7.80% at the onset of AMI to 59.58┬▒9.24% at six to eight weeks later after cardiac rehabilitation (p<0.05), while no significant changes were shown in the SV, LVEDD, and LVESD when compared between those at the onset and those at six to eight weeks after rehabilitation (Table 2).
In the GXT conducted after the six-month cardiac rehabilitation program after AMI, the maximal oxygen consumption (VO2max) significantly increased from 28.0┬▒5.6 ml/kg/min at early period to 30.3┬▒7.2 ml/kg/min six months later (p<0.05). The submaximal rate pressure product at stage 3 (RPPIII), submaximal rate of perceived exertion at stage 3 (RPEIII), and resting heart rate significantly decreased six months later when compared to those at an early period (p<0.05) (Table 3).
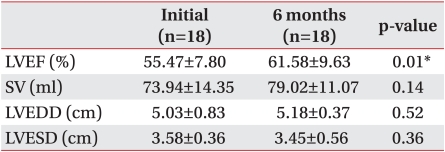
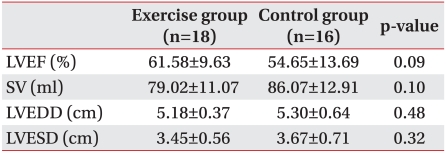
As for the exercise group, the LVEF six months later was 61.58┬▒9.63%, significantly increased when compared to that of early period (p<0.05), but the SV, LVEDD, and LVESD did not show significant changes (Table 4). Meanwhile, no significant changes in the LVEF, SV, LVEDD, and LVESD six months later between the exercise group and the control group (Table 5).
During the six-month cardiac rehabilitation program in this study, no cardiovascular complications such as angina pectoris, AMI, or death in the exercise group and the control group.
According to the statistics by the Korea Centers for Disease Control and Prevention in 2005, acute myocardial infarction occurred 1.05 out of 1,000 people with prevalence of 3.39 people and was gradually increasing annually.10 Acute myocardial infarction is classified as a main disease cause of death because of its death rate of 19.7 out of 100,000 people,10 and patients would have lower quality of life because the ones who survive find it hard to live daily life due to general deterioration in cardiopulmonary function.11 Therefore, it is most important to improve cardiopulmonary function and prevent recurrence of myocardial infarction after AMI, and cardiac rehabilitation improves both effectively.3,4 Furthermore, as the period of hospitalization for myocardial infarction becomes shorter and many patients return to their daily life immediately after early discharge, several studies are investigating methods to maximize effects of cardiac rehabilitation programs by applying the programs as early as possible.12,13
In this study, when the six-month regular cardiac rehabilitation program including six-to-eight week monitoring exercise actively starting at the 14th day (mean), when AMI was applied, the maximal oxygen consumption (VO2max) significantly increased, and maximal rate pressure product (RPPmax), perceived exertion, and resting heart rate significantly decreased. However, the cardiac rehabilitation program after AMI was not applied early because of concern that early exercise may have adverse effects on myocardial remodeling such as increase in left ventricular diameter and decrease in LVEF.5,6 Recently studies showed that cardiac rehabilitation programs did not have adverse effects on myocardial remodeling,7,8,14 but the controversy is still unsettled.
The results of the echocardiography in this study showed that six months after AMI onset the LVEF of the exercise group was 61.58┬▒9.63%, which was higher than that of the control group, 54.65┬▒13.69%, but not statistically significant. Such results indicate that the program did not have adverse effects on myocardial remodeling, but rather, higher LVEF may suggest that the cardiac rehabilitation program recovered myocardial function. However, large-scaled studies are needed to validate this observation because the number of subjects in both groups used in this study was insufficient to make conclusions about such a tendency. Based on the results of the echocardiography of the exercise group with consistent exercise for six months from the 14th day (mean) of AMI onset with regular cardiac rehabilitation program, the LVEF significantly increased but the SV, LVEDD, and LVESD did not show significant changes, indicating that early cardiac rehabilitation exercise did not have adverse effects on myocardial remodeling six to eight weeks later or six months later.
Such results are consistent with those of Dubach et al.7 and Cannistra et al.,8 reporting that relatively early cardiac rehabilitation exercise after AMI did not have adverse effects on myocardial remodeling.
This study had some limitations. First, because all the AMI patients as the subjects were asked to participate in the cardiac rehabilitation program and those who did not were classified into the control group, no random classification was applied to the selection of the exercise group and the control group. Second, the control group was not conducted of graded exercise test because they did not offer consent to participation in the cardiac rehabilitation program. Thus, it was not possible to ensure whether the significant increase in motor cardiopulmonary function of the exercise group participating in the six-month cardiac rehabilitation program was caused by the cardiac rehabilitation exercise or by natural recovery, a comparison that requires further studies. Third, the mean LVEF of the subjects was relatively favored, at least 50% and over. The adverse myocardial remodeling by exercise is known to occur more frequently when the size of ventricular wall infarction was larger and the LVEF was lower.15-17 Thus, further studies are needed for patients for whom LVEF was lower (30 to 50%). Also, it was not clearly assessed whether the control group managed risk factors well, which also needs further studies. Fourth, the number of subjects in this study was low and female subjects were too few, and further studies are needed to address this.
Traditionally, cardiac rehabilitation programs were carefully conducted after early four-to-six-week period for stability, but nowadays the initiation time is being advanced. In this study, during the early regular cardiac rehabilitation program conducted from the 14th day (mean) of AMI onset, there were no adverse changes in myocardial remodeling that was expected, and cardiovascular complications were not observed. Such results may ensure the safety of an early regular cardiac rehabilitation program, and further studies are needed to assess safety continuously.
The six-month cardiac rehabilitation program that started from the 14th day (mean) of the onset of AMI did not have adverse effects on myocardial function nor cause severe cardiovascular complications. Therefore, early regular cardiac rehabilitation program after AMI may be relatively safe.
References
1. Oldridge NB, Guyatt GH, Fischer ME, Rimm AA. Cardiac rehabilitation after myocardial infarction. Combined experience of randomized clinical trials. JAMA 1988;260:945-950. PMID: 3398199.


2. O'Connor GT, Buring JE, Yusuf S, Goldhaber SZ, Olmstead EM, Paffenbarger RS Jr, Hennekens CH. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation 1989;80:234-244. PMID: 2665973.


3. Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Porta TA, Kirkeeide RL, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998;280:2001-2007. PMID: 9863851.


4. Haskell WL, Alderman EL, Fair JM, Maron DJ, Mackey SF, Superko HR, Williams PT, Johnstone IM, Champagne MA, Krauss RM, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease: the Stan ford Coronary Risk Intervention Project (SCRIP). Circulation 1994;89:975-990. PMID: 8124838.


5. Gaudron P, Eilles C, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation 1993;87:755-763. PMID: 8443896.


6. Jugdutt BI, Michorowski BL, Kappagoda CT. Exercise training after anterior Q wave myocardial infarction: importance of regional left ventricular function and topography. J Am Coll Cardiol 1988;12:362-372. PMID: 3392328.


7. Dubach P, Myers J, Dziekan G, Goebbels U, Reinhart W, Vogt P, Ratti R, Muller P, Miettunen R, Buser P. Effect of exercise training on myocardial remodeling in patients with reduced left ventricular function after myocardial infarction: application of magnetic resonance imaging. Circulation 1997;95:2060-2067. PMID: 9133516.


8. Cannistra LB, Davidoff R, Picard MH, Balady GJ. Moderate-high intensity exercise training after myocardial infarction: effect on left ventricular remodeling. J Cardiopulm Rehabil 1999;19:373-380. PMID: 10609188.


9. Newby LK, Eisenstein EL, Califf RM, Thompson TD, Nelson CL, Peterson ED, Armstrong PW, Van de Werf F, White HD, Topol EJ, et al. Cost effectiveness of early discharge after uncomplicated acute myocardial infarction. N Engl J Med 2000;342:749-755. PMID: 10717009.


10. Korea Centers for Disease Control and Prevention. 2005 Health Behavior and Chronic Disease Statics. 2008.Korea: Ministry of health & Welfare; p.56-60.
11. Brezinka V, Kittel F. Psychosocial factors of coronary heart disease in women: a review. Soc Sci Med 1996;42:1351-1365. PMID: 8735892.


12. Aamot IL, Moholdt T, Amundsen BH, Solberg HS, M├Ėrkved S, St├Ėylen A. Onset of exercise training 14 days after uncomplicated myocardial infarction: a randomized controlled trial. Eur J Cardiovasc Prev Rehabil 2010;17:387-392. PMID: 19940774.


13. Alhaddad IA, Hakim I, Siddiqi F, Lagenback E, Mallavarapu C, Nethala V, Mounce D, Ross PL, Browm EJ Jr. Early exercise after experimental myocardial infarction: effect on left ventricular remodeling. Coron Artery Dis 1998;9:319-327. PMID: 9812181.


14. Schmid JP, Anderegg M, Romanens M, Morger C, Noveanu M, Hellige G, Saner H. Combined endurance/resistance training early on, after a first myocardial infarction, does not induce negative left ventricular remodeling. Eur J Cardiovasc Prev Rehabil 2008;15:341-346. PMID: 18525391.


15. Giannuzzi P, Temporelli PL, Corra U, Gattone M, Giordano A, Tavazzi L. Attenuation of unfavorable remodeling by exercise training in postinfarction patients with left ventricular dysfunction: results of the exercise in left ventricular dysfunction (ELVD) trial. Circulation 1997;96:1790-1797. PMID: 9323063.


16. Gaudron P, Hu K, Schamberger R, Budin M, Walter B, Ertl G. Effect of endurance training early or late after coronary artery occlusion on left ventricular remodeling, hemodynamics, and survival in rats with chronic transmural myocardial infarction. Circulation 1994;89:402-412. PMID: 8281676.


17. Oh BH, Ono S, Gilpin E, Ross J Jr. Altered left ventricular remodeling with beta-adrenergic blockade and exercise after coronary reperfusion in rats. Circulation 1993;87:608-616. PMID: 8093867.


Table┬Ā3
Changes of Graded Exercise Test in Exercise Group after 6 Months
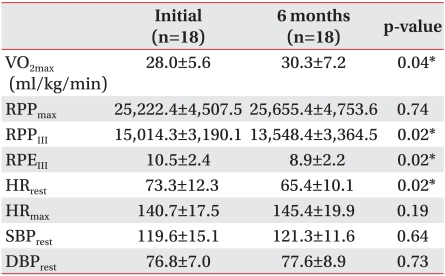
Values are given as mean┬▒standard deviation
VO2max: Maximal oxygen consumption, RPPmax: Maximal rate pressure product, RPPIII: Submaximal rate pressure product at stage 3, RPEIII: Submaximal rate of perceived exertion at stage 3, HRrest: Resting heart rate, HRmax: Maximal heart rate, SBPrest: Resting systolic blood pressure, DBPrest: Resting diastolic blood pressure
*p<0.05
-
METRICS

-
- 12 Crossref
- Scopus
- 5,138 View
- 63 Download
- Related articles in ARM