- Search
| Ann Rehabil Med > Volume 35(4); 2011 > Article |
Abstract
Objective
To investigate the characteristics of foot deformities in patients with Charcot-Marie-Tooth (CMT) disease compared with normal persons according to severity of disease.
Method
Sixty-two patients with CMT disease were recruited for this study. The normal control group was composed of 28 healthy people without any foot deformity. Patients were classified into a mild group and a moderate group according to the CMT neuropathy score. Ten typical radiological angles representing foot deformities such as pes equinus and pes varus were measured. The CMT group angles were compared with those of the normal control group, and those of the mild group were also compared with those of the moderate group.
Results
The lateral (Lat.) talo-first metatarsal angle, anteroposterior talo-first metatarsal angle, Lat. calcaneal-first metatarsal angle, Lat. naviocuboid overlap, Lat. calcaneal pitch, Lat. tibiocalcaneal angle, and Lat. talocalcaneal angle in the CMT group showed a significant difference compared to the normal control group (p<0.05). These findings revealed CMT patients have pes cavus, forefoot adduction, midfoot supination and pes varus deformity. Compared to the mild group, the moderate group significantly showed an increased Lat. calcaneal pitch and decreased Lat. calcaneal-first metatarsal angle, Lat. tibiocalcaneal angle, Lat. talocalcaneal angle, and Lat. talo-first metatarsal angle (p<0.05). These findings revealed that the pes cavus deformity of CMT patients tend to be worse with disease severity.
Charcot-Marie-Tooth disease (CMT) is known to be a hereditary motor sensory neuropathy or progressive peroneal muscular atrophy since Charcot, Marie and Tooth made the first report on 10 patients whose chief complaints were peroneal muscular atrophy in 1886. Its causes and pathophysiological mechanism have been multilaterally researched so far1-5 but are still not clear.6 This disease is autosomally, dominantly inherited and a kind of peripheral neuropathy that causes progressive and symmetric motor and sensory disturbance in lower limbs, in which occurrence is focused on the lower limbs. Clinically, it is characterized by paresthesia and muscle atrophy that develops from the periphery of hands and feet and gradually spreads to the proximal region. It is known that the severity of such symptoms is influenced by the degree of axonal degeneration.7,8 However, the natural clinical progress of CMT is not fully known.
Most patients with CMT complain of pains, muscle weakness and deformities.9 In particular, pes cavus and pes varus comprise the highest proportion of foot deformities.10 Such deformities cause abnormal gait, and in serious cases patients may lose the ability to walk. In addition, common shoes may not be suitable for patients, which may give rise to pains. With regards to the mechanism of foot deformities, various hypotheses have been suggested, but atrophy and imbalance of foot intrinsic muscles have been known to be the primary cause.11,12 Many previous studies have investigated the characteristics of foot deformities in patients with CMT compared to the normal control group,13,14 but there has been no study on the correlation between foot deformity and disease progress or severity.
Therefore, in this study, radiography was performed on the feet of 62 patients with CMT in a standing posture, and an analysis of the severity of foot deformities was performed. A control group was applied to this study to determine the characteristics of foot deformities. In addition, the CMT neuropathy score (CMT-NS) was analyzed and compared with the severity of foot deformities for the same purpose.
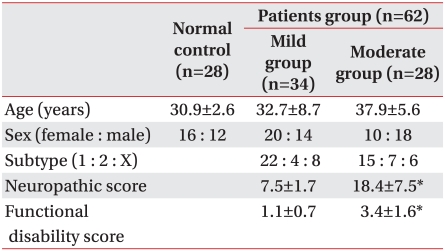
This study was conducted on 62 patients aged 18 and older who were able to walk independently and were definitely diagnosed with CMT on the authority of physical examinations, family history research, electromyography (EMG) and molecular genetic tests. Patients who did not want to take part or had difficulty maintaining the standing posture were excluded from this study. Subjects included 30 men and 32 women. They consisted of 37 type 1 patients, 11 type 2 patients and 14 type X patients. Their average age was 35.27. All of the 62 subjects were classified into 2 groups in accordance with the CMT-NS and the standard of Shy.15 The 34 patients who scored 10 points and less were classified as the mild group and the other 28 who scored more than 11 points were classified as the moderate group. In relation to age, gender and subtypes, there were no significant intergroup differences. In the CMT-NS, the mild group and the moderate group scored average 7.5 and 18.4 points, respectively. For the functional disability score (FDS),16 the mild group and the moderate group scored an average of 1.1 and 3.4, respectively. Statistically, the moderate group got higher grades on CMT-NS and FDS in comparison with the mild group (p<0.05). The control group was composed of 28 normal adults aged between 20 and 60. In relation to age and gender, there were no significant differences between the experimental and control group (Table 1).
In all the groups, sensory and motor symptoms were observed and physical examinations, including limb sensation and muscle power, were performed. CMT-NS was calculated by the measurement of the compound motor action potential and sensory action potential in the ulnar nerve. CMT-NS was criteria to analyze the clinical progress of CMT and the therapeutic effect, which was based on the total neuropathy score (TNS)17 that has been used for diabetic neuropathy and toxic neuropathy. CMT-NS reflected the severity of CMT well and its reliability and validity has been proved.
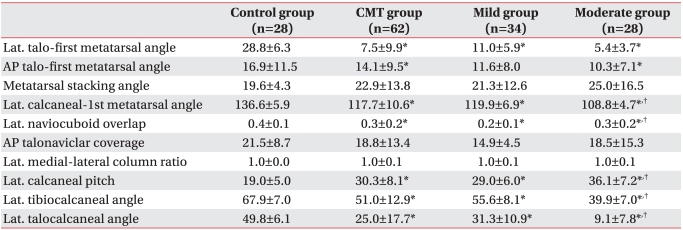
Anteroposterior and lateral-view plain radiography was performed on the feet of all the subjects in a standing posture, and 10 radiologic indexes related to forefoot, midfoot and hindfoot deformities were calculated (Fig. 1). In the 10 radiologic indexes, the lateral (Lat.) talo-first metatarsal angle, the metatarsal stacking angle, the anteroposterior (AP) talo-first metatarsal angle18 and the Lat. naviculocuboid overlap reflect the severity of forefoot deformity. The Lat. calcaneal-first metatarsal angle, the AP talonavicular coverage and the Lat. medial-lateral column ratio reflect the severity of midfoot deformity. The Lat. calcaneal pitch, the Lat. tibiocalcaneal angle and the Lat. talocalcaneal angle reflect the severity of hindfoot deformity.
The Lat. talo-first metatarsal angle decreases in proportion to the severity of cavus deformity in the forefoot, which was defined as the angle between the longitudinal midline of the talus and that of the first metatarsal bone. The metatarsal stacking angle increases in proportion to the severity of supination deformity in the forefoot. The plantar region of the first metatarsal head, the base and the plantar region of the fifth metatarsal bone were referred to as 'A', 'B' and 'C' respectively, for which the included angle was measured. The AP talo-first metatarsal angle decreased in proportion to the severity of adduction deformity in the forefoot, which was defined as the angle between the longitudinal midline of the first metatarsal bone and of the talus.
The Lat. calcaneal-first metatarsal angle18 decreased in proportion to the severity of cavus deformity in the midfoot. A hypothetical line was drawn from the front most protrusion of the calcaneus and the calcaneal tuberosity in the proximal region of calcaneocuboid articular surface, and an extension line was drawn from the first metatarsal midline, from which the included angle was measured. The Lat. naviculocuboid overlap was in inverse proportion to supination in the midfoot. The upper edge of the cuboid and its lower edge were referred to as 'a' and 'b' respectively, and the lower edge of the navicula was referred to as 'c'. The ratio of the distance between 'a' and 'c' and that between 'a' and 'b' was scored on a percentage basis. The AP talonavicular coverage was in proportion to the severity of abduction in the midfoot. The medial part of the talar articular surface and its lateral part were referred to as 'a' and 'b', respectively, and those of navicular articular surface were referred to as 'c' and 'd', respectively. Then, two vertical lines were referred to as 'A' and 'B' respectively, from which the included angle was measured. In the case of the Lat. medial-lateral column ratio, the more elevated the medial column became compared to the lateral one, the higher the ratio became. A hypothetical line drawn from the distal region of the first metatarsal bone to the posterior region of the talus was referred to as the medial column, and that from the distal region of the fifth metatarsal bone to the posterior region of the calcaneus was referred to as the lateral column, from which the medial-lateral column ratio was calculated.
In the case of the Lat. calcaneal pitch, its rise implies that cavus deformity in the hindfoot progresses. It was calculated by the measurement of the angle between a hypothetical line, drawn from the greatest protrusion of the calcaneus in the proximal region of calcaneocuboid articular surface to the lowest plantar region of the calcaneal tuberosity,19 and an extension line drawn from the plantar soft tissue so that it could be parallel with the floor. In a similar way, the Lat. tibiocalcaneal angle was to show the severity of the cavus deformity in the hindfoot, which was inversely proportional to the severity of the cavus deformity. The angle between a hypothetical line was used to calculate this measurement, drawn from the greatest protrusion of the calcaneus in the proximal region of the calcaneocuboid joint to the lowest plantar region of the calcaneal tuberosity,19 and a line from anatomical axis of the tibia. The Lat. talocalcaneal angle reflects the severity of the varus deformity in the hindfoot, which is inversely proportional to the severity of the varus deformity in the hindfoot. The angle between a hypothetical line was used to calculate this measurement, drawn from the greatest protrusion of the calcaneus in the proximal region of the calcaneocuboid joint to the calcaneal tuberosity,19 and a line from anatomical axis of the talus.
Plain radiography was performed on the feet of patients with CMT, from whom 10 radiologic indexes were analyzed. With regard to the results, a comparison was made between experimental groups and the control group, through which the characteristics in the foot deformities of patients with CMT were investigated. The severity of patients with CMT was classified into the mild group and the moderate group, on the basis of CMT-NS. In addition, 10 radiologic indexes were analyzed in the control group in the same way, in which intergroup comparisons and analyses were made. Taken altogether, the correlation between foot deformity and disease severity was investigated.
Data was statistically analyzed using the program SAS 13.0 (SPSS Inc., Chicago, USA). The radiologic indexes of the experimental and control group were analyzed by the student t-test, and comparisons were made by the ANOVA test. Intergroup comparisons were made by Turkey's-b test. The significance level was defined as a p-value of less than 0.05.
The Lat. talo-first metatarsal angle of experimental groups was 7.5 degrees on average, which was significantly narrower than that of the control group (28.8 degrees). Thus, experimental groups showed a higher incidence rate of cavus deformity in the forefoot. In experimental groups, the AP talo-first metatarsal angle averaged 14.1 degrees. It was significantly narrower compared to that of the control group (16.9 degrees). Experimental groups showed a higher incidence rate of adduction deformity in the forefoot in comparison with the control group (p<0.05). However, in the metatarsal stacking angle, which was an index for supination deformity in the forefoot, there was no significant inter group difference (Table 2).
The Lat. calcaneal-first metatarsal angle was 117.7 degrees on average in experimental groups, which was significantly narrower than that of the control group (136.6 degrees). Thus, experimental groups showed a higher incidence rate of cavus deformity in the midfoot. The Lat. naviculocuboid overlap was 0.3 degree in experimental groups, which was significantly narrower than that of the control group (0.4 degree). Patients showed a higher incidence rate of supination deformity in the midfoot (p<0.05). In the AP talonavicular coverage and Lat. medial-lateral column ratio, however, there was no significant intergroup difference (Table 2).
The Lat. calcaneal pitch was 30.3 degrees on average in experimental groups, which was significantly wider than that of the control group (19.0 degrees) and the Lat. tibiocalcaneal angle was 51.0 degrees on average in experimental groups, which was significantly narrower than that of the control group (67.9 degrees). Experimental groups showed a higher incidence rate of cavus deformity in the hindfoot (p<0.05). The Lat. talocalcaneal angle was 25.0 degrees in experimental groups, but that of the control group was 50.0 degrees. The incidence rate of varus deformity in the hindfoot was significantly higher in experimental groups (p<0.05) (Table 2).
The Lat. talo-first metatarsal angle was significantly narrower in both the mild group and moderate group in comparison to the control group (p<0.05). The moderate group averaged 5.4 degrees, while the mild group averaged 11.0 degrees, but this was not statistically significant. In the AP talo-first metatarsal angle, there was no significant difference between the mild group and the control group. However, it was significantly narrower in the moderate group (10.3 degrees) compared to the control group (16.9 degrees) (p<0.05). In addition, in the metatarsal stacking angle, there was no significant difference among the three groups (Table 2).
The Lat. calcaneal-first metatarsal angle was significantly narrower in experimental groups than in the control group. In particular, the moderate group showed a narrower angle (108.8 degrees) compared to the mild group (119.9 degrees), which was statistically significant (p<0.05). The Lat. naviculocuboid overlap was significantly narrower in experimental groups than in the control group (p<0.05). In the AP talonavicular coverage and the Lat. medial-lateral column ratio, significant intergroup differences were not observed (Table 2).
The Lat. calcaneal pitch was significantly wider in experimental groups than in the control group. In particular, the moderate group showed a narrower angle (26.1 degrees) compared to the mild group (29.0 degrees) (p<0.05). The Lat. tibiocalcaneal angle was significantly narrower in experimental groups than in the control group. The moderate group and the mild group showed 39.9 and 55.6 degrees, respectively, whereas the moderate group showed a narrower angle compared to the mild group (p<0.05). In the case of the Lat. talocalcaneal angle, the two experimental groups showed significantly narrower angles as compared to the control group. In experimental groups, the moderate group showed a statistically narrower angle (9.1 degrees) compared to the mild group (31.3 degrees) (p<0.05) (Table 2).
As shown above, CMT causes cavus deformity in the fore foot, midfoot and hindfoot. This result was consistent with previous studies in which macroscopic observations of pes cavus deformities18-20 of patients with CMT were performed. However, few studies have dealt with foot deformities using objective radiographic indexes. Aktas and Sussman13 performed plain radiography on 26 patients with CMT and measured their Lat. tibiocalcaneal angles and Lat. talo-first metatarsal angles, reporting that forefoot and hindfoot deformities were observed unlike normal. Chan et al.14 measured the Lat. talo-first metatarsal angle, Lat. calcaneal-first metatarsal angles and Lat. calcaneal pitches and reported pes cavus deformity in the forefoot, midfoot and hindfoot. The results of this study, based on radiographic indexes, were consistent with those of the previous studies based on plain radiography.
In this study, the moderate group showed a higher severity of pes cavus caused by midfoot and hindfoot deformities, in comparison with the mild group, which implies that pes cavus became more severe as the CMT progressed. One issue is that there has been no further study based on radiographic indexes or no previous study that has dealt with the correlation between deformity and disease severity, and thus it is difficult to compare results. Sabir and Lyttle19 made macroscopic observations of patients with CMT aged between 4 and 59 and reported that pes cavus comprised the highest proportion of foot deformities and that these deformities progressed. With regards to the mechanism and progress of pes cavus, Sabir and Lyttle19 maintained that denervation would develop from the distal region to the proximal region. Specifically, it began in the intrinsic muscles of the feet, and then progressed into the flexor digitorum longus, the flexor digitorum brevis, the extensor hallucis longus and the extensor hallucis brevis in the order named, by extension, into the peroneal muscle, the extensor digitorum longus, the tibialis posterior and the tibialis anterior. According to their report, in the initial stage, denervation occured in the intrinsic muscles of the feet and the metatarsophalangeal joint was excessively extended as the extensor digitorum longus applied extensive force, and as a result functioned as a windlass and so the longitudinal arch became higher. Then, small muscles in the plantar region atrophied and accelerated pes cavus. Contrary to Sabir and Lyttle,19 Mann and Missirian12,21 represented that intermuscular imbalance was the cause. In adult patients with CMT, they observed the anterior muscles of lower limbs became weak but the posterior muscles of lower limbs were similar in force to normal muscles, and the peroneus longus muscle was strong but peroneus brevis muscle was atrophied. In addition, the peroneus longus muscle was stronger relative to the anterior tibial muscle and the posterior tibial muscle was stronger relative to peroneus brevis muscle. Likewise, Tynan et al.22 performed MRI scans and reported intermuscular morphological imbalance. Additionally, they maintained that plantar flexion occurs in the first ray due to the peroneus longus muscle, which is stronger than the anterior tibial muscle, and consequently caused cavus deformity in the forefoot. In addition, small muscles in the plantar region atrophied and the ensuing contracture of the plantar fascia accelerated the pes cavus. However, there controversy about the two hypotheses still exists, and prospective studies have not been conducted to date.
In this study, the mild group and the moderate group showed significant differences in midfoot and hindfoot deformities, which means the pes cavus became more severe as the CMT progressed. However, intergroup differences were not observed in relation to the cavus deformity in the forefoot. Thus, pes cavus in the forefoot develops early on and becomes more severe or is maintained with time.23
In this study, the mild group did not show significant changes in connection with adduction deformity in the forefoot, but the moderate group showed significant adduction deformity compared to the control group. These results were consistent with those of previous studies, showing that in the early stages of foot deformity, atrophy occurred in the intrinsic muscles of the feet, and progressed in the muscles of the lower limbs. In this case, the peroneus brevis muscle atrophied faster than the posterior tibial muscle, and intermuscular imbalance and adduction deformity in the forefoot occurred.19
The results of this study showed that varus deformity in the hindfoot increased in the experimental groups compared to the control group and became more severe as the disease progressed. Likewise, supination deformity in the midfoot showed the same phenomena. In relation to the severity of supination deformity in the forefoot, experimental groups did not show significant differences compared to the control group. In this regard, Mann and Missirain21 and Jacobs and Carr et al.11 reported that varus deformity occurred as the posterior tibial muscle and the flexor digitorum longus muscle were stronger relative to the peroneus brevis muscle. Sabir and Lyttle19 showed that varus deformity in the hindfoot occurred as the subtalar joint was deformed when pes cavus progressed. Hallgrimsson24 and McCluskey et al.25 reported that varus in the hindfoot was to counteract the supination of the first ray in the forefoot during the stance phase. In this study, varus in the hindfoot and supination in the midfoot increased, but in relation to supination in the forefoot, significant differences were not observed. Since adduction in the forefoot occurred after the disease progressed, the hypothesis of intermuscular imbalance was considered to be more persuasive than the hypo thesis that varus in the hindfoot counteracts forefoot deformity.16,26
To evaluate foot deformities, physical examinations, plain radiography, motion analysis and foot printing are used. In the case of motion analysis, motion markers are used and it is convenient to analyze the motions of lower limbs, but it is difficult to observe foot deformities, which also can be a financial burden. Plain radiography has been widely used to observe foot deformities in many studies because it is convenient. Sala et al.27 and Rathjen and Mubarak28 performed plain radiography and measured radiological angles while observing foot deformities and their clinical progress. Radiography may be used in this way to comparatively analyze foot deformities and clinical progress. Foot deformities are greatly affected when it bears up body weight, and thus it is better to perform radiography when the patient is in a standing posture.29 In this study, all the subjects were in a standing posture while being radiographed.
This study was conducted on a comparatively large num ber of patients with CMT, and an investigation was made into the correlation between deformity and disease severity. However, it may be difficult to conduct pro spective long-term follow-ups, and therefore this study could not show foot deformity according to disease progress. Moreover, it could not deal with the claw toe, a common foot deformity of patients with CMT. In this connection, there is a need to conduct a prospective long-term study so that such drawbacks may be remedied.
In this study, radiography was performed on the feet of 62 patients with CMT in a standing posture, and the deformities of their feet were investigated. In addition, the correlation between deformity and disease severity in accordance with CMT-NS was analyzed. The results showed that pes cavus, forefoot adduction, midfoot supination and hindfoot varus occur in patients with CMT, and that such deformities became more severe as the disease progressed. This study was expected to be helpful to determine the correlation between deformity and disease severity, as well as to treat such deformities. In the event that follow-ups are conducted, the deformities may be analyzed more systematically.
ACKNOWLEDGEMENTS
This work was supported by Professor Research funds of Yonsei University College of Medicine in 2005 (6-2005-0034).
References
1. Dyck PJ, Lambert EH. Lower motor and primary sensory neuron diseases with peroneal muscular atrophy. I. Neurologic, genetic, and electrophysiologic findings in hereditary polyneuropathies. Arch Neurol 1968;18:603-618. PMID: 4297451.


2. Madrid R, Bradley WG, Davis CJ. The peroneal muscular atrophy syndrome. Clinical, genetic, electrophysiological and nerve biopsy studies. Part 2. Observations on pathological changes in sural nerve biopsies. J Neurol Sci 1977;32:91-122. PMID: 864493.


3. Apfel SC, Asbury AK, Bril V, Burns TM, Campbell JN, Chalk CH, Dyck PJ, Feldman EL, Fields HL, Grant IA, et al. Positive neuropathic sensory symptoms as endpoints in diabetic neuropathy trials. J Neurol Sci 2001;189:3-5. PMID: 11596565.


4. Thomas PK, Calne DB. Motor nerve conduction velocity in peroneal muscular atrophy: evidence for genetic heterogeneity. J Neurol Neurosurg Psychiatry 1974;37:68-75. PMID: 4813428.



5. Buchthal F, Behse F. Peroneal muscular atrophy (PMA) and related disorders. I. Clinical manifestations as related to biopsy findings, nerve conduction and electromyography. Brain 1977;100:41-66. PMID: 861715.



6. Nielsen VK, Pilgaard S. On the pathogenesis of Charcot-Marie-Tooth disease. A study of the sensory and motor conduction velocity in the median nerve. Acta Orthop Scand 1972;43:4-18. PMID: 5080641.


7. Krajewski KM, Lewis RA, Fuerst DR, Turansky C, Hinderer SR, Garbern J, Kamholz J, Shy ME. Neurological dysfunction and axonal degeneration in Charcot-Marie-Tooth disease type 1A. Brain 2000;123:1516-1527. PMID: 10869062.



8. Sahenk Z, Chen L. Abnormalities in the axonal cytoskeleton induced by a connexin32 mutation in nerve xenografts. J Neurosci Res 1998;51:174-184. PMID: 9469571.


9. Skre H. Genetic and clinical aspects of Charcot-Marie-Tooth's disease. Clin Genet 1974;6:98-118. PMID: 4430158.


10. Holmes JR, Hansen ST Jr. Foot and ankle manifestations of Charcot-Marie-Tooth disease. Foot Ankle 1993;14:476-486. PMID: 8253442.


11. Jacobs JE, Carr CR. Progressive muscular atrophy of the peroneal type (Charcot-Marie-Tooth disease) orthopaedic management and end-result study. J Bone Joint Surg Am 1950;32A:27-38. PMID: 15401720.


12. Mann DC, Hsu JD. Triple arthrodesis in the treatment of flxed cavovarus deformity in adolescent patients with Charcot-Marie-Tooth disease. Foot Ankle 1992;13:1-6. PMID: 1577335.


13. Aktas S, Sussman MD. The radiological analysis of pes cavus deformity in Charcot Marie Tooth disease. J Pediatr Orthop B 2000;9:137-140. PMID: 10868366.


14. Chan G, Sampath J, Miller F, Riddle EC, Nagai MK, Kumar SJ. The role of the dynamic pedobarograph in assessing treatment of cavovarus feet in children with Charcot-Marie-Tooth disease. J Pediatr Orthop 2007;27:510-516. PMID: 17585258.


15. Shy ME, Rose MR. Charcot-Marie-Tooth disease impairs quality of life: Why? And how do we improve it? Neurology 2005;65:790-791. PMID: 16186514.


16. Gallardo E, Garcia A, Combarros O, Berciano J. Charcot-Marie-Tooth disease type 1A duplication: spectrum of clinical and magnetic resonance imaging features in leg and foot muscles. Brain 2006;129:426-437. PMID: 16317020.



17. Cornblath DR, Chaudhry V, Carter K, Lee D, Seysedadr M, Miernicki M, Joh T. Total neuropathy score: validation and reliability study. Neurology 1999;53:1660-1664. PMID: 10563609.


18. Azmaipairashvili Z, Riddle EC, Scavina M, Kumar SJ. Correction of cavovarus foot deformity in Charcot-Marie-Tooth disease. J Pediatr Orthop 2005;25:360-365. PMID: 15832156.


19. Sabir M, Lyttle D. Pathogenesis of pes cavus in Charcot-Marie-Tooth disease. Clin Orthop Relat Res 1983;175:173-178. PMID: 6839584.

20. Coleman SS, Chesnut WJ. A simple test for hindfoot flexibility in the cavovarus foot. Clin Orthop Relat Res 1977;123:60-62. PMID: 852192.

21. Mann RA, Missirain J. Pathophysiology of Charcot-Marie-Tooth disease. Clin Orthop Relat Res 1988;234:221-228. PMID: 3409580.

22. Tynan MC, Klenerman L, Helliwell TR, Edwards RH, Hayward M. Investigation of muscle imbalance in the leg in symptomatic forefoot pes cavus: a multidisciplinary study. Foot Ankle 1992;13:489-501. PMID: 1478577.


23. Swanson AB, Browne HS, Coleman JD. The cavus foot: concepts of production and treatment by metatarsal osteotomy. J Bone Joint Surg Am 1966;48:1019-1020.
24. Hallgrimsson S. Pes cavus, seine behandlung und einige bemerkungen uber steinie atiologic. Acta Orthop Scand 1939;10:73-76.

25. McCluskey WP, Lovell WW, Cummings RJ. The cavovarus foot deformity. Etiology and management. Clin Orthop Relat Res 1989;247:27-37. PMID: 2676298.
26. Alexander IJ, Johnson KA. Assessment and management of pes cavus in Charcot-Marie-Tooth disease. Clin Orthop Relat Res 1989;246:273-281. PMID: 2766615.

27. Sala DA, Grant AD, Kummer FJ. Equinus deformity in cerebral palsy: recurrence after tendo Achillis lengthening. Dev Med Child Neurol 1997;39:45-48. PMID: 9003729.


28. Rathjen KE, Mubarak SJ. Calcaneal-cuboid-cuneiform osteotomy for the correction of valgus foot deformities in children. J Pediatr Orthop 1998;18:775-782. PMID: 9821135.


29. Cooke TD, Scudamore RA, Bryant JT, Sorbie C, Siu D, Fisher B. A quantitative approach to radiography of the lower limb. Principles and applications. J Bone Joint Surg Br 1991;73:715-720. PMID: 1894656.


-
METRICS

-
- 12 Crossref
- Scopus
- 4,878 View
- 43 Download
- Related articles in ARM
-
The Change of the Visual Analogue Scale According to Decreased Skin Temperature1996 June;20(2)