- Search
| Ann Rehabil Med > Volume 37(3); 2013 > Article |
Abstract
A 22-year-old woman visited our clinic with a history of radiofrequency volumetric reduction for bilateral masseter muscles at a local medical clinic. Six days after the radiofrequency procedure, she noticed a facial asymmetry during smiling. Physical examination revealed immobility of the mouth drawing upward and laterally on the left. Routine nerve conduction studies and needle electromyography (EMG) in facial muscles did not suggest electrodiagnostic abnormalities. We assumed that the cause of facial asymmetry could be due to an injury of zygomaticus muscles, however, since defining the muscles through surface anatomy was difficult and it was not possible to identify the muscles with conventional electromyographic methods. Sono-guided needle EMG for zygomaticus muscle revealed spontaneous activities at rest and small amplitude motor unit potentials with reduced recruitment patterns on volition. Sono-guided needle EMG may be an optimal approach in focal facial nerve branch injury for the specific localization of the injury lesion.
Facial palsy is a common form of neuropathy due to damage through 7th cranial nerve pathway [1]. The diagnosis of facial muscle palsy is primarily based on clinical presentation, nerve conduction study (NCS), and electromyography (EMG). Among the 20 facial nerve innervated muscles, conventional electrodiagnostic tests are performed in only the three or four muscles [2]. Also, anatomic variation and tiny muscle size pose difficulties to electrodiagnostic tests in the target muscles. In order to overcome this clinical obstacle, ultrasonography-guided needle EMG could be a useful tool for the diagnosis of facial palsy.
Here, we report a case of zygomaticus muscle paralysis after radiofrequency volumetric reduction for masseteric muscle, diagnosed using sono-guided needle EMG.
A 22-year-old woman visited our clinic complaining of left facial palsy that for four weeks. Five weeks earlier, the patient received radiofrequency volumetric reduction for masseter muscles in the bilateral buccal regions at a local medical clinic. Under local anesthesia, monopolar radiofrequency probes were inserted into the lower third of the masseter muscles through oral mucosa and coagulation was done at 20 to 30 spots in each masseter muscle. Her primary symptom was asymmetry of facial muscles. In physical examination, she was freely able to wrinkle the forehead, close the eyes completely, lift the nasal ala up and forward and contract the mouth. The only abnormal finding of the facial expression was an incomplete elevation of the left corner of the mouth when smiling (Fig. 1).
Electrophysiologic tests such as NCS, EMG, and blink reflex study for evaluation of facial nerve function revealed normal findings. Ultrasonographic search on the affected side around the inferior region of the zygomatic bone revealed a hypomobile tiny zygomaticus muscle (Fig. 2). On the other side, the zygomaticus muscle was drawn upward and laterally and normal muscle activity when the patient was smiling. Thickness and sizes of bilateral muscles were symmetric with the thickness, 0.15 cm/left, 0.18 cm/right and area, 0.18 cm2/left, 0.14 cm2/right.
EMG needle was inserted under the guidance of ultrasonography into the zygomaticus muscle which led to the detection of abnormal spontaneous activities at rest and small amplitude motor unit action potentials with reduced recruitment patterns on volition (Fig. 3).
Furthermore, facial magnetic resonance imaging (MRI) was performed to detect muscle atrophy and discontinuity of focal facial nerve branch. However, there was no definite muscle atrophic change or nerve injury lesion such as swelling, fluid collection or mass.
To the best of our knowledge, this is the first case of facial focal peripheral neuropathy diagnosed by needle EMG with ultrasonography guidance.
In the present case, the patient received radiofrequency volumetric reduction for masseter muscles in the bilateral buccal regions the development of before facial palsy. This radiofrequency procedure is a minimally invasive method for volumetric reduction of masseteric hypertrophy performed in the lower third of the masseter muscles through oral mucosa under local anesthesia. A study by Park and Lee [4] on two cases of facial nerve palsy complication in 350 patients suggested that the radiofrequency probe must be inserted into the lower one third of the masseter muscle to protect the buccal branches of the facial nerves. However, the above study did not discuss the severity or location of the symptoms. In our case, the lesion of facial asymmetry caused by radiofrequency procedure was diagnosed by ultrasonographic procedure.
Zygomaticus muscle is primarily innervated by the zygomatic and buccal branches of the facial nerve and these branches also have some variation. A morphological study of facial nerves in Koreans found several types of anastomosis in the facial nerve branches and complex anastomosis of the mandibular branch and zygomatic branch in up to 17% [4].
In our ultrasonographic study, we found the hypomobile zygomaticus muscle at the affected side. Zygomaticus muscles consist of zygomaticus major and minor, which arise from the lateral surface of the zygomatic bone and attached to lateral lip [5]. There are some variant types, such as bifid zygomaticus muscle [6]. Our findings enabled to define the zygomatic muscles around the zygomatic bone by using ultrasonography. Previous studies have revealed the size of the zygomaticus muscles ranging from approximately 3.33 to 5.79 mm, using ultrasonography [7,8], in the present, the thickness of the zygomaticus muscle was about 1.5 to 1.8 mm symmetrically. These differences may be due to the measurement levels, in which we tried to measure the thickness of the muscles near the insertion level for a better observation of the muscle movement at the affected side, whereas previous studies measured the thickness of muscles at its thickest level for the purpose of facial morphologic study.
It was difficult to differentiate between direct muscle injury and nerve damage. Fibrillations and positive sharp waves may also occur after muscle trauma as well as nerve injury [9]. Our patient was having nerve injury rather than muscle injury as the sonographic study, thicknesses of bilateral zygomaticus muscles were symmetric and there were no evidence of muscle tear. According to the study of Barqfrede et al. [10], the first ultrasonographic abnormalities such as increased muscular echo intensity, appeared 2 weeks after acute injury and the pathological spontaneous activity was not associated with high muscle echo intensity in about 27% of extremity muscles examined. In this case, we were able to find only the electromyographic abnormality in the zygomaticus muscle on the affected side only about a month after injury and there was no evidence of inflammation or hematoma associated with direct muscle trauma on MRI. In our patient, the radiofrequency probe approach technique may have induced injury to the zygomatic branch of the facial nerve.
In needle EMG, use of monopolar needle electrodes or standard concentric needle electrodes is the standard practice. The recording area of the concentric needle electrode is a hemisphere with a radius range approximately 1.0 to 2.5 mm. This uptake area's radius is approximately two-third times that of monopolar needle electrode [2]. In our study, we used both needles and through the concentric needle electrode, we were able to gather more stable baseline with less noise compared with the monopolar type. We believe that using the concentric needle electrode is more appropriate when approaching tiny facial muscles such as zygomaticus muscle.
Focal facial neuropathy is often difficult to diagnose due its size and variations. Sono-guided needle EMG may be an optimal approach to detect the lesion and confirm the focal facial neuropathy.
References
1. Roob G, Fazekas F, Hartung HP. Peripheral facial palsy: etiology, diagnosis and treatment. Eur Neurol 1999;41:3-9. PMID: 9885321.

2. Dumitru D, Amato AA, Zwarts MJ. Electrodiagnostic medicine. 2nd ed. Philadelphia: Hanley & Belfus; 2002.
3. Park YJ, Jo YW, Bang SI, Kim HJ, Lim SY, Mun GH, et al. Radiofrequency volumetric reduction for masseteric hypertrophy. Aesthetic Plast Surg 2007;31:42-52. PMID: 17235460.


4. Park IY, Lee ME. A morphological study of the parotid gland and the peripheral branches of the facial nerve in Koreans. Yonsei Med J 1977;18:45-51. PMID: 617028.


5. Gray H, Standring S. Gray's anatomy: the anatomical basis of clinical practice. 39th ed. Edinburgh: Elsevier Churchill Livingstone; 2005.
6. Pessa JE, Zadoo VP, Garza PA, Adrian EK Jr, Dewitt AI, Garza JR. Double or bifid zygomaticus major muscle: anatomy, incidence, and clinical correlation. Clin Anat 1998;11:310-313. PMID: 9725574.


7. Satiroğlu F, Arun T, Isik F. Comparative data on facial morphology and muscle thickness using ultrasonography. Eur J Orthod 2005;27:562-567. PMID: 16135538.



8. McAlister RW, Harkness EM, Nicoll JJ. An ultrasound investigation of the lip levator musculature. Eur J Orthod 1998;20:713-720. PMID: 9926638.



9. Robinson LR. Traumatic injury to peripheral nerves. Muscle Nerve 2000;23:863-873. PMID: 10842261.


10. Bargfrede M, Schwennicke A, Tumani H, Reimers CD. Quantitative ultrasonography in focal neuropathies as compared to clinical and EMG findings. Eur J Ultrasound 1999;10:21-29. PMID: 10502636.


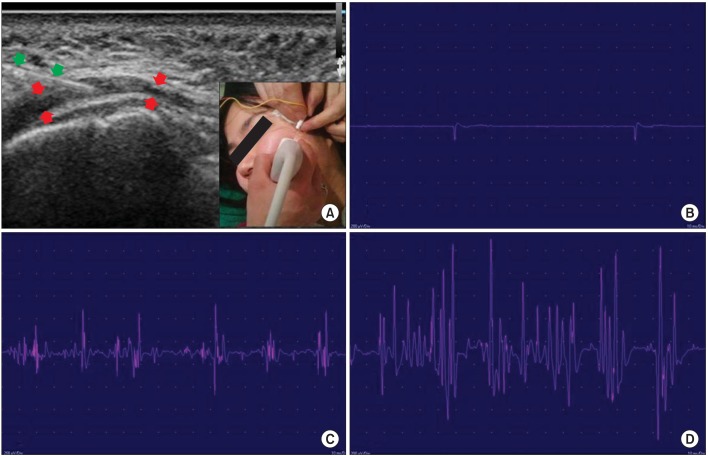
Fig. 1
Clinical figures of face. (A) Resting state, (B) frontalis muscle activation, and (C) orbicularis oris muscle activation demonstrated symmetry on both sides. However, (D) zygomaticus muscle activation (on smiling) showed asymmetry.
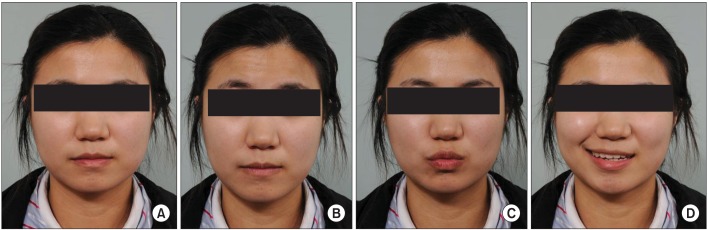
Fig. 2
Ultrasonographic figures of zygomaticus muscle. (A) Left zygomaticus muscle longitudinal view, (B) left zygomaticus muscle crossection view, (C) right zygomaticus muscle longitudinal view, (D) right zygomaticus muscle crossection view thickness and area of bilateral muscles were symmetric. Red arrow, zygomaticus muscle; Z, zygomatic bone.
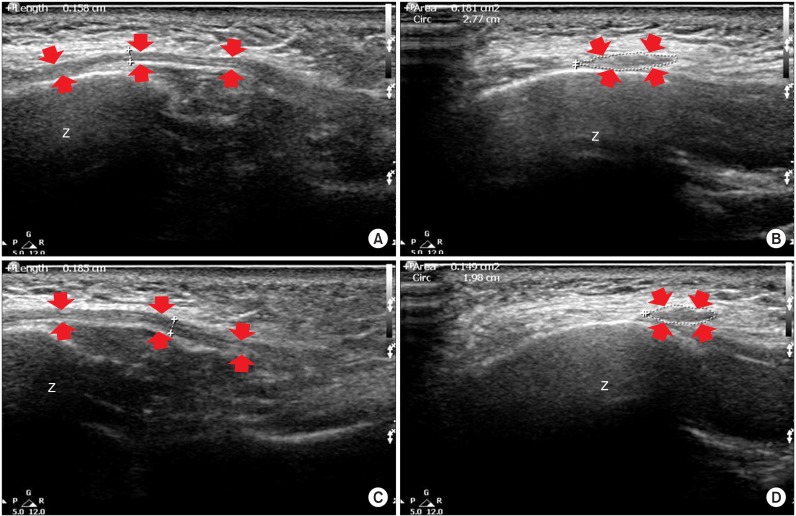
Fig. 3
Positive sharp waves and motor unit action potentials (MUAP) of zygomaticus muscle. (A) Needle insertion position in the muscle, (B) positive sharp waves in left zygomaticus, (C) MUAPs in left zygomaticus, and (D) MUAPs in right zygomaticus: gain, 200 µV/div; sweep speed, 10 ms/div. Green arrow, needle electrode; red arrow, zygomaticus muscle.