- Search
| Ann Rehabil Med > Volume 36(5); 2012 > Article |
Abstract
Plasmacytoma is a rare disease, which afflicts 2 to 3 people per every 100,000 of the general population. Solitary plasmacytoma accounts for 5% of the plasma cell neoplasm. Solitary plasmacytoma of the bone appears more vividly in the axial skeleton (25-60%), which has the red marrow and usually affects the thoracic vertebrae. We report a case of 54-year-old man who has a chest pain on the right side. After being treated for the muscle pain, his symptoms of pain were changed into weakness and allesthesia. We checked the MRI and found a mass lesion in the T5 vertebra, but there were no significant laboratory findings, in blood and urine samples. Finally, he got an operation due to the aggravation of the weakness. The result of biopsy indicated that it was a solitary plasmacytoma of the spine. After 5 months later, the weakness and allesthesia had disappeared.
Primary spinal tumor is one of the most uncommon cases of tumor, which only accounts for 4-8% of the entire tumor cases of the central nervous system. Histologically, the most common primary spinal tumors are schwannoma, meningioma and glioma. In addition, spinal hemangioma is the most common benign tumor of the spine, and metastatic tumor, Lymphoma and Multiple Myeloma are known as malignant tumors of high frequency.1
Plasmacytoma is a rare disease, occurs on 2 to 3 out of 100,000 people. Among the various types of plasmacytoma, solitary plasmacytoma of the bone is a unique entity, rating only 2-10% of the entire tumor cases. Solitary plasmacytoma of the bone is prone to occur on the axial skeleton, which has red bone marrow, and usually occurs on the thoracic spine.2,3 Solitary plasmacytoma is easily misconceived as a degenerative spinal disease, because generally, the radiating pain or the contracted local pain around the spine could occur. Thus, it usually takes 6 months, in average, to be diagnosed correctly. Because a number of plasmacytoma patients transmigrate to multiple myeloma, clinicians regard solitary palsmacytoma as an uncommon early stage of multiple myeloma.4 We report this unique case that caused us to encounter an atypical clinical symptom and laboratory finding, which led us to difficulties in the initial diagnosis.
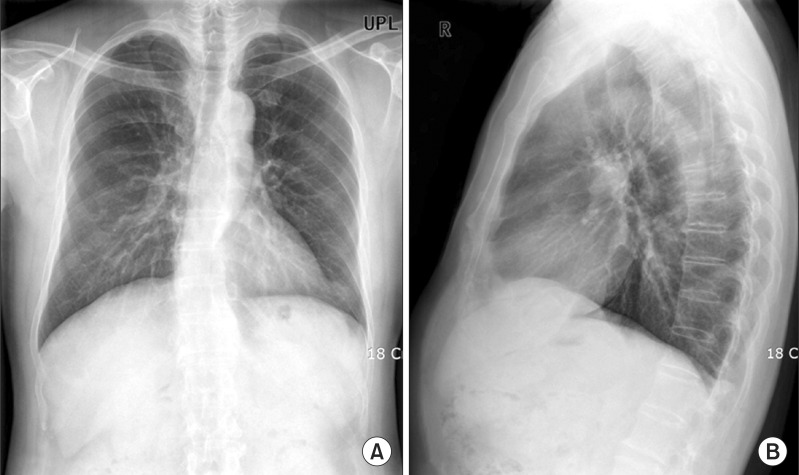
A 54-year-old man was presented to the outpatient clinic of the Department of Physical Medicine and Rehabilitation, Kyung Hee University Medical Center, with complaints of the right-side chest pain, which started in April, 2009. From the past medical history of the patient, he got peritonitis caused by perforated appendicitis and had surgery in 1976, and in 1984, he had pneumonia and received treatment. When he came to the clinic this time, for a basic inspection, he underwent an X-ray examination of the thorax and lumbar spine. Compared to the others in his age group, the patient had a relatively greater degenerative change in thoracic region and the lumbar vertebra. He also had slight spinal scoliosis, but any special findings were not revealed (Fig. 1). On that day, he received a trigger point injection, in accordance with myofascial pain syndrome, because no other neurological abnormal findings were perceived.
On his first visit, he had both lower extremity manual muscle test, and it showed a normal muscle power, including no symptom of dysaesthesia. Moreover, the result was fine and normal on both the lower extremity deep tendon reflexes, and there was no spasticity or ankle clonus. After giving the trigger point injection on the first visit, we prescribed NSAIDs and muscle relaxant. Additionally, the patient had physical therapy for a week. One week later, the pain itself showed a declining pattern, but the patient complained of numbness and weakness on both lower extremities. Physical examination was conducted again, but still, there was no special finding.
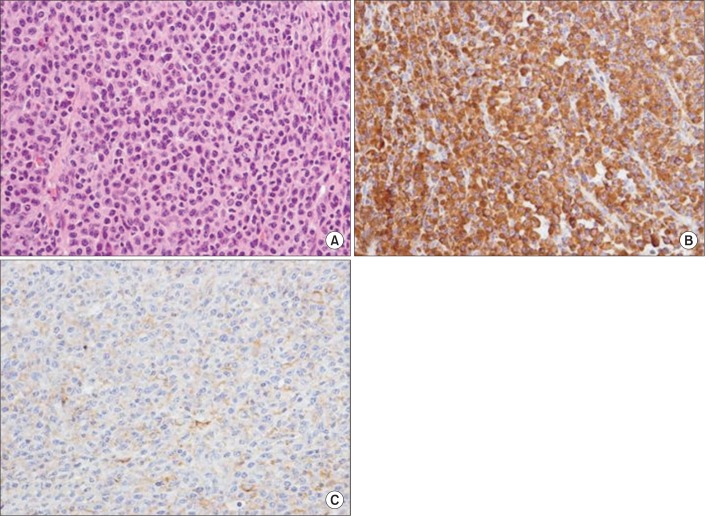
From the first day of the treatment, two weeks had passed and the patient came to the clinic, again. He complained of persisting weakness, so we checked a thoracic MRI for further diagnosis. In an MRI scan, we found a lesion occupying the 5th vertebral body and part of the posterior vertebral structure. Because of this lesion, the spinal cord was thrust out on the left side. Moreover, from the T1 and T2 enhanced images, this lesion showed a low signal intensity of the tumor, similar to the bone (Fig. 2). Although the tumor invaded one vertebral body and one bone marrow, the right-side neural and spinal canal, posterior spinous process, it didn't greatly damage the cortex of the bone.
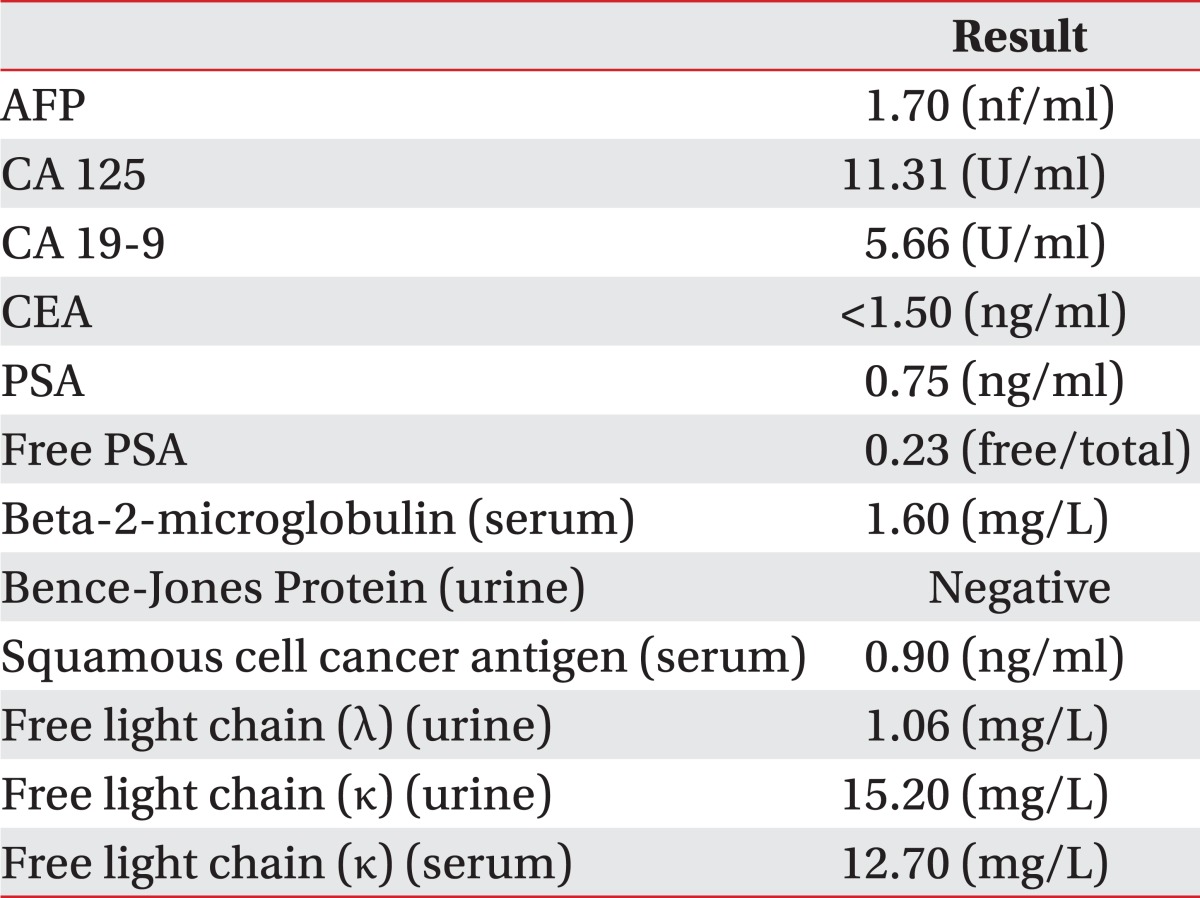
In the initial differential diagnosis, metastatic spinal tumor was suspected. As such, we checked the blood and urine of the patient, using a serum and urine free light chain (κ, λ), urine Bence-Jones protein, serum Beta-2-microglobulin, and tumor marker. From the laboratory findings, there was no significant incidence of tumor, like multiple myeloma or plasmacytoma (Table 1). Additionally, in the skull X-ray, there were no peculiar findings, either. Both somatosensory and motor evoked potential were examined; on the somatosensory evoked potential, on the right-side, the defect of sensory pathway were detected, and on the left-side, the test result was normal; the motor evoked potential showed non-significant findings.
Subsequent bone scan examination showed only a slight reaction of the bone formation on the 5th thoracic spine, and there were no other unusual findings.
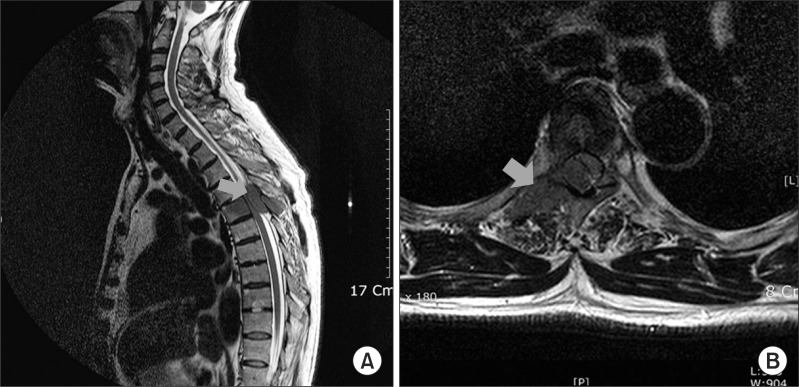
According to the laboratory and radiologic findings, this case was suspected as a lymphoma, one kind of a metastatic spinal cord tumor, and the patient was transferred to the department of neurosurgery. He underwent an operation and a biopsy; during the operation, the biopsy result was differing from the initial diagnosis, which suspected plasmacytoma. Afterwards, for the clinical confirmation, a bone marrow biopsy was conducted additionally, and the lesion was diagnosed as a plasmacytoma on the vertebral body of the 5th thoracic spine, Monoclonal Gammopathy of Undetermined Significance (Fig. 3). After ten times of the local radiation therapy, the patient's weakness and numbness on both the lower extremities were gradually subsided.
Neoplasm of the plasma cell can be divided as the plasma cell myeloma, plasmacytoma, immunogloblinopathy, osteoclastic myeloma, and heavy-chain disease. Among these diseases, plasmacytoma is a proliferative disorder of the plasma cell neoplasm, which could biologically be considered malignant. It is a truly unique disease, taking only 5% of the entire plasma cell neoplasms. Additionally, it can be divided into a solitary plasmacytoma of the bone and extramedullary plasmacytoma. Diagnosis can be done by physical, radiological and laboratory tests, but the clinical confirmation can be done by a biopsy.5 Furthermore, solitary plasmacytoma tends to develop into multiple myeloma, but related prognosis has not been defined yet. Through local treatments that targets the plasmacytoma, only 50% of the entire patient population proceeds into multiple myeloma.6 Thus, in case of solitary plasmacytoma, we must do a biopsy and find the other site of the lesion, which may exist for exact diagnosis.
We tried to diagnose accurately by testing the blood and urine, but couldn't get any meaningful results. After doing the biopsy, we came to get the precise diagnosis. Further, we checked a detailed imaging study for plasmacytoma as a solitary lesion. As mentioned above, in the cases of multiple myeloma or plasmacytoma, it is general to detect the tumor maker through the blood and urine tests. However, like this case illustrates, we figured out that there could be an atypical plasmacytoma, which can only be detected after a certain operational treatment. According to the location of the neoplasm of the spinal column, symptoms could be so slight that it is sometimes misperceived as myalgia. In addition, the symptom would not occur until it invades any structure that triggers certain reactions. Thus, the correct diagnosis could be delayed by the time when the actual symptoms appear.
Baba et al.7 reported a clinical pattern of the solitary plasmacytoma is pain in general, which can be an extended radiating pain in the course of time. Under this circumstance, the weakness of the muscle may imply a spinal cord compression or cauda equina syndrome. Furthermore, Dimopoulos et al.4 mentioned that pain caused by bone destruction from an invasion of the plasma cell tumor is the most common symptom, in relation to the solitary plasmacytoma of the bone. Additionally, they reported a compression fracture on the thoracic region or the lumbar vertebra, which can cause severe spasm or back pain, is also one of the common symptoms. Patients can possibly have neuropathic symptom because of the compression on the spinal cord or nerve root.8
Although 24% to 72% of the tumor marker, related to plasmacytoma, is usually detected by blood and urine tests, herein, nothing was found by a laboratory diagnosis.8 This case report is applicable to an atypical spinal tumor, which couldn't be detected by the initial physical examination and radiologic test. Thus, it is not easy to confirm the disease until the tissue is extracted through operations. On the basis of the above findings, the case had unique patterns compared to the common plasmacytoma cases, and moreover, unless the problematic neuropathic symptom is accompanied, this spinal tumor could be misperceived as a simple muscle pain. Thus, we report this as a clinical case of atypical plasmacytoma.
When a patient complains of back pain without any specific accompanied symptoms, it is easy to assume for some of the common causes, including muscle pain. However, if weakness or numbness on the extremity is accompanied, radiological diagnosis, including MRI, has to be checked. Afterwards, if the tumor is detected, blood and urine tests for tumor marker, bone marrow examination, and biopsy have to be followed up, and the operational treatment has to be considered. If plasmacytoma is found in a biopsy after the operation, additional radiotherapy or chemotherapy has to be carried out, with co-consultation of Oncologists, surgeons, and radiation oncologists.
Rehabilitation medication doctors have high possibility of detecting this kind of uncommon cases before any others. Thus, they should approach prudently and observe carefully not to miss any yet-invisible lesions. Even after the operation and radiotherapy, outpatient follow-up have to be done to chase for the appearance of another lesion or multiple myeloma, and also, surveillance and care on patient condition have to be continued.
References
1. Schellinger KA, Propp JM, Villano JL, McCarthy BJ. Descriptive epidemiology of primary spinal cord tumors. J Neurooncol 2008;87:173-179. PMID: 18084720.


2. Taira H, Takasita M, Yoshida S, Tsumura H, Torisu T. Extraosseous calcified plasmacytoma causing thoracic myelopathy. Skeletal Radiol 1999;28:347-349. PMID: 10450883.


3. Takahashi T, Koshu K, Tominaga T, Takahashi A, Yoshimoto T. Solitary plasmacytoma in the thoracic spine. Two case reports. Neurosurg Rev 1998;21:121-125. PMID: 9795946.


4. Dimopoulos MA, Moulopoulos LA, Maniatis A, Alexanian R. Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood 2000;96:2037-2044. PMID: 10979944.


5. Terada T. Solitary plasmacytoma of the thoracic vertebra presenting with sudden paraplegia and back pain: a pathologic case report. Pathol Oncol Res 2011;17:167-169. PMID: 20676811.


6. Poor MM, Hitchon PW, Riggs CE Jr. Solitary spinal plasmacytomas: management and outcome. J Spinal Disord 1988;1:295-300. PMID: 2980978.


7. Baba H, Maezawa Y, Furusawa N, Wada M, Kokubo Y, Imura S, Imamura Y, Yamada Y. Solitary plasmacytoma of the spine associated with neurological complications. Spinal Cord 1998;36:470-475. PMID: 9670382.



8. McLain RF, Weinstein JN. Solitary plasmacytoma of the spine: a review of 84 cases. J Spinal Disord 1989;2:69-74. PMID: 2520065.


Fig. 2
T2 weighted MRIs show low signal changes like bone mass in sagittal view (A) and transverse view (B). These mass lesions show homogenous densities and slightly destructed cortex, red arrow: suspected mass lesions.
- TOOLS