- Search
| Ann Rehabil Med > Volume 36(1); 2012 > Article |
Abstract
Objective
To investigate the efficacy of ultrasonography (US)-guided injections in patients with low lumbar facet syndrome, compared with that in patients who received fluoroscopy (FS)-guided injections.
Method
Fifty-seven subjects with facet syndrome of the lumbar spine of the L4-5 and L5-S1 levels were randomly divided into two groups to receive intraarticular injections into the facet joint. One group received FS-guided facet joint injections and the other group received US-guided facet joint injections. Treatment effectiveness was assessed using a visual analogue scale (VAS), physician's and patient's global assessment (PhyGA, PaGA), and the modified Oswestry Disability Index (MODI). All parameters were evaluated four times: before injections, and at a week, a month, and three months after injections. We also measured, in both groups, how long it took to complete the whole procedure.
Results
Each group showed significant improvement from the facet joint injections on the VAS, PhyGA, PaGA, and MODI (p<0.05). However at a week, a month, and three months after injections, no significant differences were observed between the groups with regard to VAS, PhyGA, PaGA, and MODI (p>0.05). Statistically significant differences in procedure time were observed between groups (FS: 248.7┬▒6.5 sec; US: 263.4┬▒5.9 sec; p=0.023).
Lumbar facet or zygapophysial joints are common sources of lumbar spinal pain.1 In addition to causing localized spinal pain, facet joint pain may refer to adjacent structures. In particular, lumbar facet joints may refer pain to the back, buttocks, and proximal lower extremities.2 "Facet syndrome" includes buttock pain, pseudoradicular-type pain in the posterior thigh or inguinal area, tenderness of paravertebral regions corresponding to facet joints, and aggravation of pain from maneuvers that exert maximum irritation on the joints, or from transitional movements. Facet syndrome is diagnosed by clinical characteristics and by excluding other causes of lower back pain.3
Facet joint injections are commonly administered to alleviate back pain and/or to aid in determining whether the facet joint is a source of pain. Injections are usually administered under fluoroscopy (FS) guidance to ensure success and to avoid complications.4 Some physicians also use computed tomography (CT) scanning for guidance, when available. However, these techniques include exposure to ionizing radiation for both the patient and the therapist, and can only be performed in specially equipped pain clinics.5
In contrast ultrasonography (US) is a portable, moderately priced imaging modality which is not associated with radiation exposure. The current role of US-guided injections has recently been summarized6: so far, US has been used for guidance with a broad variety of injections.
Galiano et al.7 demonstrated that a US approach to the facet joint is feasible and has minimal risk, compared to CT-controlled injections. CT-guided injections are difficult to perform because of the large size of the equipment required and the high cost. Therefore, the purpose of this study is to investigate the efficacy of US-guided injections in patients with facet syndrome of the low lumbar spine, compared with that in patients who received FS-guided injections.
Subjects who visited our outpatient department with low-back pain were included in the study. Fifty-nine patients diagnosed with facet syndrome of the lumbar spine were participants, and fifty-seven patients completed the entire study protocol.
Patients were included if they (1) had pain associated with lumbar hyper-extension, lateral flexion, and tenderness on paravertebral regions corresponding to facet joints but normal findings on the straight leg raise test and neurologic examination, (2) had undergone a simple X-ray of their lumbar spine, and (3) were >18 years old. Patients were excluded if they (1) had a local or systemic infection, (2) had an allergy to steroids or lidocaine, (3) had uncorrectable coagulopathy, or (4) were pregnant.7 Patients were randomly assigned to one of two groups to receive intraarticular injections into the lumbar facet joint. One group received FS-guided facet joint injections, and the other group received US HD 11 XE (Philips Medical System, Bothell, USA)-guided facet joint injections. Facet joint injections were limited to the L4-5 and L5-S1 levels.
FS-guided facet joint injections were administered in a fluoroscopy room at a radiology center. Interventions were performed in a 45┬░ tilted state from the prone position with a pillow under the abdomen.8 If the facet joint was clearly identified under FS, a spinal needle was advanced perpendicularly until bony contact was felt. All procedures were performed under sterile conditions.8 Each facet joint (left L4-5, L5-S1 or right L4-5, L5-S1 or bilateral L4-5 and L5-S1 levels according to symptoms) was infiltrated with a mixture containing 10 mg of triamcinolone and 2 ml of 1% lidocaine.
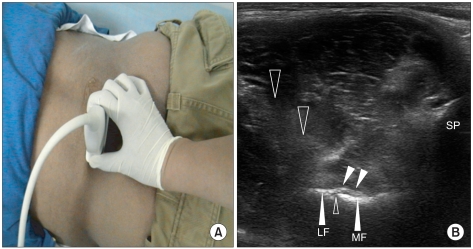
US-guided injections were performed by one expert. Patients were placed in a prone position. Posterior paravertebral parasagittal sonograms were obtained to indentify of the different spinal levels (Fig. 1). The spinous process and adjacent structures (lamina of the vertebral arch, facet joint, accessory process, and mamillary process) were delineated by transverse sonograms at the target level, and the midpoint of the facet joint space was established.9 All procedures were performed under sterile conditions. If the joint was clearly or partially visible, a spinal needle was advanced under US guidance into the joint space of each lumbar facet joint. The needle was inserted 1-2 cm laterally from the midline at the lateral end of the transducer and precisely positioned in the US plane at an angle of approximately 45┬░ with respect to the axial plane until the needle tip reached the target and bony contact was felt.9 This enabled visualization of the needle, which appeared as a bright line-shaped echo pattern on the transverse sonogram (Fig. 2). If the needle placement was correct, a mixture containing 10 mg of triamcinolone and 2 ml of 1% lidocaine was administered intraarticularly (until resistance was encountered) and injected around the posterior facet joint capsule, in the same manner as for the FS-guided injections.
For comparison of improvements between the two groups, the following outcome measures were selected and evaluated; before injections and at a week, a month, and three months after injections. Pain regarding the facet joints was assessed using a visual analogue scale (VAS), and activities of daily living (ADL) were assessed using physician's global assessment (PhyGA) (subjective), patient's global assessment (PaGA) (objective), and the modified Oswestry Disability Index (MODI). Each assessment was evaluated when patients visited our outpatient department or completed a telephone survey. Procedure time was recorded for both groups. Elapsed time was measured from the moment of placing the patient in the prone position. If all injections were performed, the elapsed time was stopped and recorded.
SPSS (version 16.0 for Windows) was used to compare differences in outcome measures (SPSS Inc., Chicago, USA). For nonparametric variables, the Wilcoxon signed-rank test was used for pairwise multiple comparisons. The Mann-Whitney U test was used for multiple comparisons between the two groups. A p-value<0.05 was considered significant.
Among the fifty-seven subjects, thirty-two subjects received FS-guided injections, and twenty-five subjects received US-guided injections. The demographic characteristics of the groups are shown in Table 1.
No clinically relevant differences in outcome measures were observed between the two groups at baseline. Both groups that received FS- and US-guided injections showed significant improvement on the VAS, PhyGA, PaGA, and MODI at a week (p<0.05), a month (p<0.05), and three months (p<0.05) after injections (Table 2).
However, no significant differences in the VAS, PhyGA, PaGA, and MODI were observed between the groups at a week, a month, and three months after injections (Table 2). Statistically significant differences in procedure time were observed between the groups (FS: 248.7┬▒6.5 sec; US: 263.4┬▒5.9 sec; p=0.023).
Facet joint injections are preferentially performed as CT-controlled or FS-controlled interventions. But, most practitioners prefer FS-guided injections in clinics, rather than CT, as a guide for facet joint injections.
Galiano et al.9 recently described the US approach for administering lumbar facet joint injections. To simulate joint infiltration, on an embalmed cadaver, a spinal needle was advanced under US guidance into the space of each lumbar facet joint. Placement of the needle tip was verified by CT. Therefore, the described technique of a US-guided approach to the joint space of the lumbar facet joint articulation has been demonstrated to be feasible and accurate.10 The fact that US-guided facet joint injections can be rapidly performed in clearly visible cases is not surprising. Because of the immediate availability of information on the feasibility of US imaging of target structures, once visualized, the needle can be advanced to the target structure in just a few seconds and under safe, real-time-controlled conditions. In this study, the needle placement was correct in almost all cases in which the target could be precisely identified and visualized. No additional roentgenological control is required, if the target structures are exact using US. Therefore, US-guided injections could be performed simply in an outpatient clinic. Additionally, US is not associated with radiation exposure. Potential biological effects of high X-ray doses have been reviewed, and deterministic and stochastic effects on skin, bone, parotid glands, and lung were discussed.11 Kim et al.12 reported pigmentation on the fingernail and hand after repeated performance of FS-guided procedures.12
In our study, the FS-guided and US-guided injection groups showed significant benefit on the VAS, PhyGA, PaGA, and MODI at a week, a month, and three months after injections. We used the VAS as a pain scale, and PhyGA, PaGA, and MODI as an ADL scale. In a previous study, the benefits of injections were assessed only by VAS, and the follow-up period after injections was only six weeks.7 We diversified the evaluation tool and expanded the follow-up period to three months. Other activities in daily life appeared to show improvement according to pain reduction. Therefore, the effectiveness of facet joint injections for treating low-back pain corresponded with the results of earlier studies.13 No significant differences in the VAS, PhyGA, PaGA, and MODI were observed between the groups. In this regard, US-guided facet joint injections were not inferior by comparison with FS-guided injections for pain relief and improvement of ADL.
A significant reduction of procedure time was observed for the FS-guided facet joint injections (248.7┬▒6.5 sec) and for US-guided injections (263.4┬▒5.9 sec) when the level of injections was limited to both the L4-5 and L5-S1 levels (FS: 21; US: 16). This procedure time was only from the time the patient was lying in the prone position to receive the injections. Therefore, this time did not include a preparatory period, such as entry into the procedure room and adjustments of the equipment before injections. Although the time for the FS-guided injections was shorter than that for the US-guided injections, conducting the FS-guided injections required additional time because of the arrangement of injection reservations, movement to the radiology center, and a longer preparatory period, including adjusting fluoroscopic equipment. However, these are not cumbersome procedures. Therefore, the total US-guided procedure time may be shorter than that for FS-guided injections. No major complications, such as hematoma or infection, were observed.
The present study had some limitations, which included a small patient group. Another limitation was that the level of injections was limited to only the lower lumbar spine, at the L4-5 and L5-S1 levels. As the level of facet joint increased, the facet joint became vertical, so the joint could not be well visualized on US, compared with that of lower lumbar levels, such as L4-5 and L5-S1. Therefore, we could not apply a broader lumbar spine level. Additionally, we measured the time only at the L4-5 and L5-S1 levels. Finally, a long-term follow-up evaluation should be included.
In conclusion, US-guided injections in patients with lumbar facet syndrome are as effectiveness as FS-guided injections for pain relief and improvement of ADL. US guidance is a rapid and safe means of ensuring that injections are administered into facet joints. Therefore, it might be easy to perform this procedure in the outpatient department. US-guided injections are a good treatment choice for facet syndrome of the low lumbar spine.
References
1. Boswell MV, Colson JD, Spillane WF. Therapeutic facet joint interventions in chronic spinal pain: a systematic review of effectiveness and complications. Pain Physician 2005;8:101-114. PMID: 16850048.


2. Sehgal N, Shah RV, McKenzie-Brown AM, Everett CR. Diagnostic utility of facet (zygapophysial) joint injections in chronic spinal pain: a systematic review of evidence. Pain Physician 2005;8:211-224. PMID: 16850075.


3. Joy H, Ha SK, Kim SH, Lim DJ, Park JY, Suh JK. Prognostic factors of percutaneous radiofrequency neurotomy on the posterior primary ramus. J Korean Neurosurg Soc 2003;33:51-55.
4. Bogduk N. International Spinal Injections Society guidelines for the performance of spinal injections procedures. Part I: Zygapophysial joint blocks. Clin J Pain 1997;13:285-302. PMID: 9430809.


5. Greher M, Kirchmair L, Enna B, Kovacs P, Gustorff B, Kapral S, Moriggl B. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. Anesthesiology 2004;101:1195-1200. PMID: 15505456.


6. Greher M, Kapral S. Is regional anesthesia simply an exercise in appliedsonoanatomy?: aiming at higher frequencies of ultrasonographic imaging. Anesthesiology 2003;99:250-251. PMID: 12883395.


7. Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med 2007;32:317-322. PMID: 17720116.


8. Manchikanti L, Manchikanti KN, Manchukonda R, Cash KA, Damron KS, Pampati V, McManus CD. Evaluation of lumbar facet joint nerve blocks in the management of chronic low back pain: preliminary report of a randomized, double-blind controlled trial: clinical trial NC T00355914. Pain Physician 2007;10:425-440. PMID: 17525777.


9. Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, Schatzer R, Ploner F. Ultrasound guidance for facet joint injections in the lumbar spine: a computed tomography-Controlled feasibility study. Anesth Analg 2005;101:579-583. PMID: 16037179.


10. Aguirre DA, Bermudez S, Diaz OM. Spinal CT-guided interventional procedures for management of chronic back pain. J Vasc Interv Radiol 2005;16:689-697. PMID: 15872324.


11. Wagner LK, Eifel PJ, Geise RA. Potential biological effects following high X-ray dose interventional procedures. J Vasc Interv Radiol 1994;5:71-84. PMID: 8136601.


12. Kim HS, Ahn KH, Yun DH, Oh JJ, Jeong YS, Kim DH. Skin lesion after repeated fluoroscopically guided procedures: a case report. J Korean Acad Rehabil Med 2001;25:729-733.
13. Nelemans PJ, deBie RA, deVet HC, Sturmans F. Injections therapy for subacute and chronic benign low back pain. Spine 2001;26:501-515. PMID: 11242378.


Fig.┬Ā1
L4-L5 spinous processes demonstrated in a posterior paravertebral parasagittal sonogram using ultrasonography.
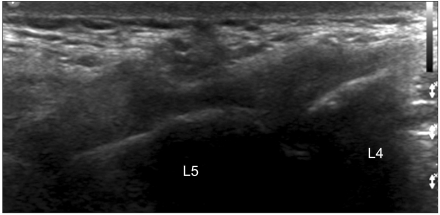
Fig.┬Ā2
(A) Photograph showing the position of the ultrasonography transducer for examining the left L4-5 lumbar facet joint (B) Sonogram corresponding to the transducer position shown in (A). SP: Spinal process, MF: Medial facet, LF: Lateral facet, Big open arrow: Needle, Small open arrow: Joint space, Small closed arrow: Facet joint capsule.
Table┬Ā2
Comparison of Pre- and Post-Injections Outcome Measures within Groups and between Groups
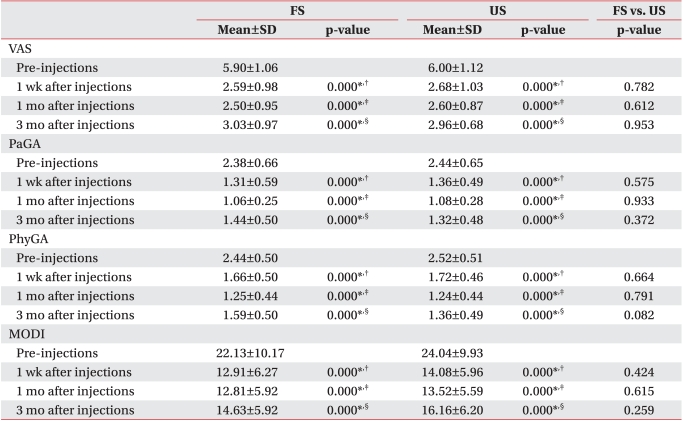
Values are mean┬▒standard deviation
FS: Fluoroscopy, US: Ultrasonography, VAS: Visual analogue scale, PaGA: Patient's global assessment, PhyGA: Physician's global assessment, MODI: Modified Oswestry Disability Index
*p<0.05, ŌĆĀpre-injections vs. 1 wk after injections, ŌĆĪpre-injections vs. 1 mo after injections, ┬¦pre-injections vs. 3 mo after injections
- TOOLS
-
METRICS

- Related articles in ARM
-
The Effect of Spinal Manipulation for Patients with Acute Low Back Pain.1999 August;23(4)
Effects of Intradiscal Steroid Injection in Patients with Lumbar Discogenic Pain.2003 April;27(2)
The Efficacy of Spinal Epiduroscopy in Patients with Low Back Pain.2003 October;27(5)






