3. Straker L, Jones KJ, Miller J. A comparison of the postures assumed when using laptop computers and desktop computers. Appl Ergon 1997;28:263-8.


5. Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int 2014;25:277-9.

6. Norasi H, Tetteh E, Sarker P, Mirka GA, Hallbeck MS. Exploring the relationship between neck flexion and neck problems in occupational populations: a systematic review of the literature. Ergonomics 2022;65:587-603.


8. Kasem SA, Abdel Raoof N, Kattabie O, Moustafa I. Effect of forward head posture on sensorimotor integration. Int J Physiother 2017;4:118-25.

14. Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther 2008;13:2-11.


15. Abdelkader NA, Mahmoud AY, Fayaz NA, Saad El-Din Mahmoud L. Decreased neck proprioception and postural stability after induced cervical flexor muscles fatigue. J Musculoskelet Neuronal Interact 2020;20:421-8.


18. Lin G, Zhao X, Wang W, Wilkinson T. The relationship between forward head posture, postural control and gait: a systematic review. Gait Posture 2022;98:316-29.


19. Salahzadeh Z, Maroufi N, Ahmadi A, Behtash H, Razmjoo A, Gohari M, Parnianpour M. Assessment of forward head posture in females: observational and photogrammetry methods. J Back Musculoskelet Rehabil 2014;27:131-9.


20. Abbasi H, Alizadeh MH, Rajabi R, Mohammadi F. Comparison of static and dynamic postural stability between individuals with and without forward head posture. Phys Treat 2020;10:127-34.

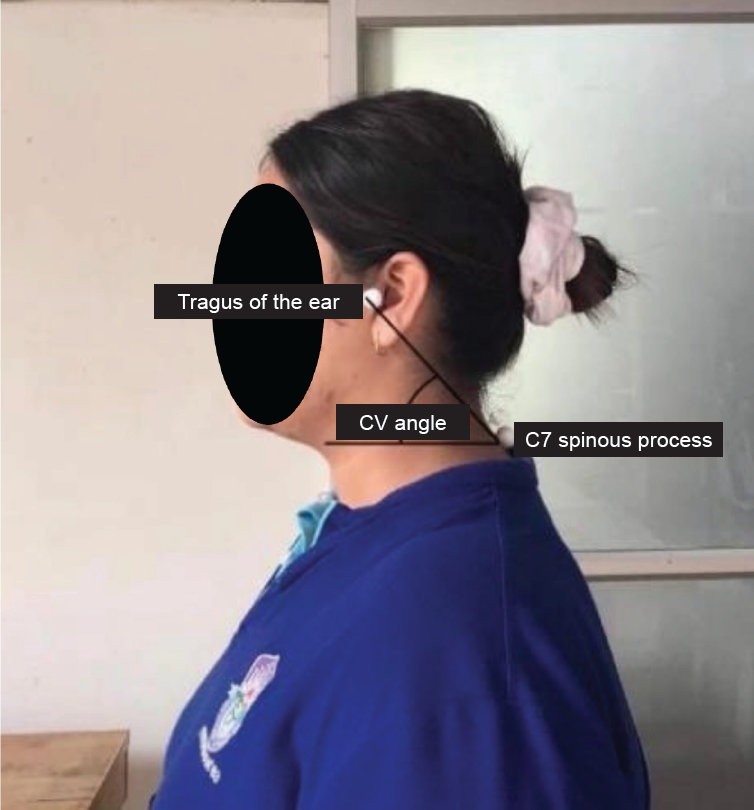
23. Gadotti IC, Magee DJ. Validity of surface measurements to assesscraniocervical posture in the sagittal plane: acritical review. Phys Ther Rev 2008;13:258-68.

25. Xie Y, Szeto GP, Dai J, Madeleine P. A comparison of muscle activity in using touchscreen smartphone among young people with and without chronic neck-shoulder pain. Ergonomics 2016;59:61-72.


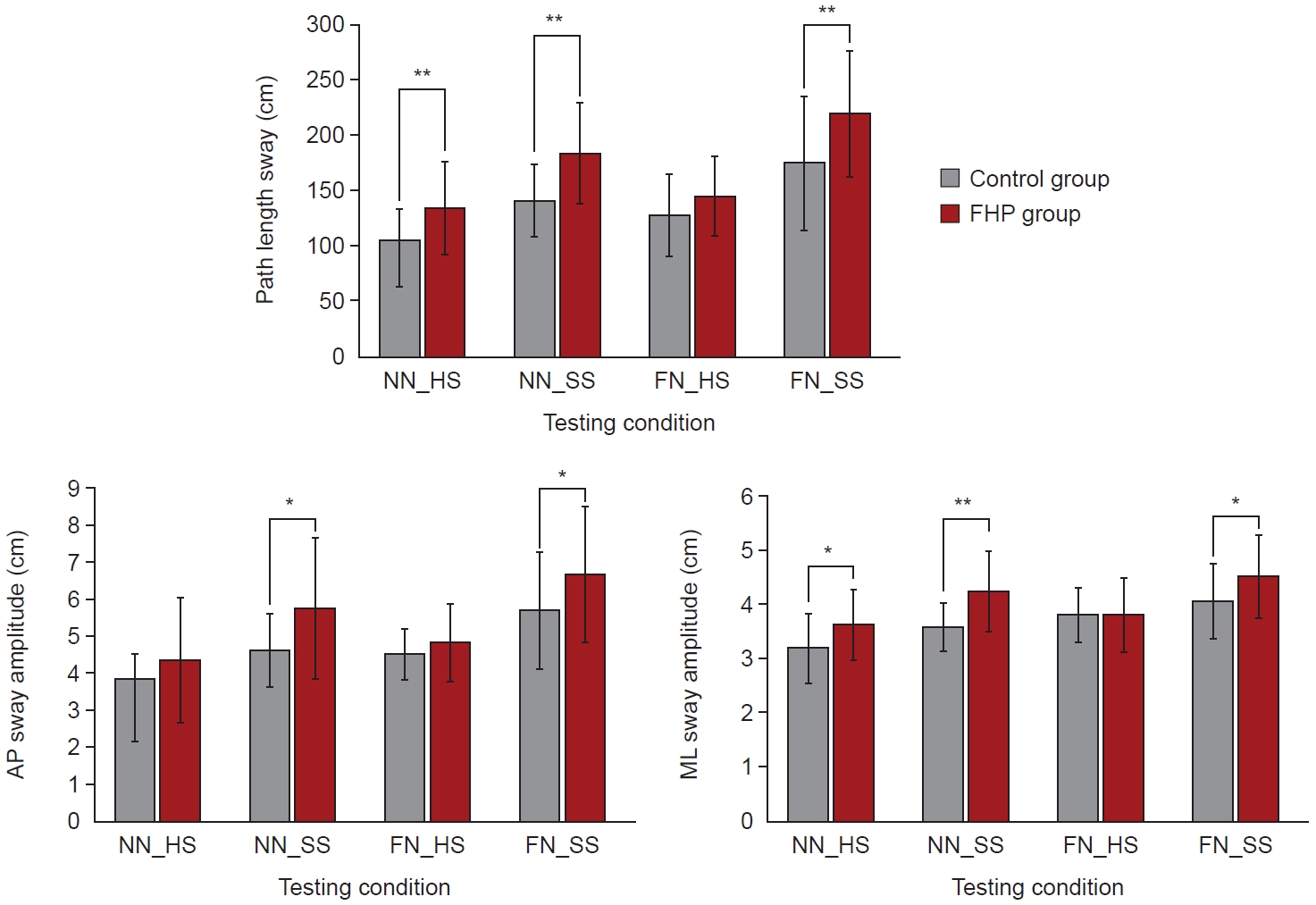
28. Donath L, Roth R, Zahner L, Faude O. Testing single and double limb standing balance performance: comparison of COP path length evaluation between two devices. Gait Posture 2012;36:439-43.


30. Alshahrani A, Aly SM, Abdrabo MS, Asiri FY. Impact of smartphone usage on cervical proprioception and balance in healthy adults. Biomed Res 2018;29:2547-52.

31. McPartland JM, Brodeur RR, Hallgren RC. Chronic neck pain, standing balance, and suboccipital muscle atrophy--a pilot study. J Manipulative Physiol Ther 1997;20:24-9.

32. Fercho J, Krakowiak M, Yuser R, Szmuda T, Zieliński P, Szarek D, et al. Kinematic analysis of the forward head posture associated with smartphone use. Symmetry 2023;15:667.

34. Samaan MN, Elnegmy EH, Elnahhas AM, Hendawy AS. Effect of prolonged smartphone use on cervical spine and hand grip strength in adolescence. Int J Multidiscip Res Dev 2018;5:49-53.
36. Quek J, Pua YH, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther 2013;18:65-71.


38. Shiravi Z, Talebian Moghadam S, Hadian MR, Olyaei G. Effect of cognitive task on postural control of the patients with chronic ankle instability during single and double leg standing. J Bodyw Mov Ther 2017;21:58-62.