Effects of Resistance Circuit Training on Health-Related Physical Fitness in People With Paraplegia: A Pilot Randomized Controlled Trial
Article information
Abstract
Objective
To evaluate the efficacy and safety of 8 weeks of resistance circuit training in people with paraplegia due to spinal cord injury.
Methods
Participants were randomized into experimental and control groups. Although the intensity and sequence of movements of the exercise programs were identical in both groups, the resting time between sets was limited to 1 minute in the experimental group. In the control group, the participants were allowed to rest until they were comfortable. Both groups received 8 weeks of training twice per week. Before and after the program, muscle mass, body fat percentage, fat mass, blood pressure, heart rate, muscle strength and muscular endurance were evaluated, and 6-minute propulsion test was conducted. Additionally, the safety of the program was assessed.
Results
Twenty-two individuals with paraplegia were enrolled (11 in each group). After the training program, the experimental group showed a significant decrease in the resting blood pressure and improvement in the upper extremity muscle mass, strength, and endurance (p<0.05). Each variable showed significant inter-group differences (p<0.05). Furthermore, none of the participants showed autonomic adverse events, musculoskeletal side effects, or discomfort.
Conclusion
The results show that resistance circuit training programs with short resting intervals are superior to the usual resistance exercise programs in improving the blood pressure and physical strength and are safe for people with upper thoracic level injuries at T6 or higher.
INTRODUCTION
The prevalence of chronic diseases such as hypertension and diabetes are increasing in people with disabilities. They are less mobile in daily life and have few opportunities to exercise. This results in obesity, which further increases the incidence of metabolic syndrome and cardiovascular diseases [1-3]. According to the 2017 National Survey of Persons with Disability (Ministry of Health and Welfare, Korea), the number of people with disabilities is increasing. Among them, 79.3% have chronic diseases, and the number is increasing [4]. Paraplegic people with activity limitation move very little in daily life and have fewer opportunities to undertake physical activities unlike those without disability. These factors make them even more vulnerable to chronic diseases [5].
Although many people with spinal cord injury are aware of the importance of physical activity for maintaining health, almost no effective exercise program exists for them. Moreover, due to the belief that people with spinal cord injury cannot engage in physical activities due to diminished physical strength, they are only offered lowintensity exercise programs at most gymnasiums.
Recent research has shown the positive effects of moderate- to high-intensity exercise in improving exercise capacity in people with spinal cord injury. One research group applied 6 weeks or more of a moderate- or highintensity exercise program, three times per week, 50–60 minutes per session in patients with spinal cord injury (C4–L2) and reported reduction in the body weight and body mass index (BMI) and improvement in the physical capacity including oxygen consumption [6]. Similarly, other researchers implemented 12 weeks of a complex exercise program three times per week, ≥30 minutes per session, in patients with spinal cord injury (T5–T12) and found improved upper extremity muscle strength [7].
Circuit training sets a target time for exercise and gradually improves muscle strength, respiration, and circulation [8]. No rest is allowed between exercises to promote cardiopulmonary improvement. It is known to promote higher metabolic rates than those with other resistance exercise programs [9]. Therefore, circuit training may serve as an optimal moderate- to high-intensity exercise program for people with spinal cord injury who have diminished muscle strength and respiratory function. However, in reality, there are no standardized circuit training programs specifically for people with spinal cord injury, and relevant previous studies are also lacking.
Furthermore, exercise programs for individuals with spinal cord injury-related disabilities must be evaluated for potential autonomic adverse events, and skin and musculoskeletal injury, to establish the safety of the programs [10].
We hypothesized that resistance circuit training program would have a greater effect on body composition, blood pressure and heart rate (HR), muscle mass and strength, muscular endurance and cardiopulmonary endurance than typical resistance exercise program with different resting interval as one of the safe exercise program applicable to individuals with spinal cord injury. Therefore, this study aimed to analyze and compare the efficacy and safety of a resistance circuit training program to a typical resistance exercise program.
MATERIALS AND METHODS
Participants
Between June and December 2019, individuals with paraplegia due to spinal cord injury volunteered to participate in the study. The inclusion criteria were as follows: adults aged >19 years who were able to ambulate with manual wheelchair independently in indoor and outdoor environment, could understand the researcher’s instructions, understood the study, and voluntarily consented to participate. The exclusion criteria were: individuals who had cardiovascular abnormalities or musculoskeletal diseases that may affect physical activity, had severe lower extremity spasticity (Modified Ashworth Scale 3 or higher), and were deemed unfit by the researchers. Sample size was calculated using G*Power 3.1 (Heinrich-Heine-Universität Düsseldorf, Germany), with two-way repeated measures ANOVA, alpha error of 5%, power of study 80%, effect size of 0.25, 1:1 allocation ratio of two groups, the calculated sample size was 34 (17 in each group).
The study was approved by the Institutional Review Board of National Rehabilitation Center (No. NRC-2019-04-031). All participants provided written informed consent before inclusion in the study.
Experimental design
Participants were randomized into experimental and control groups. Baseline homogeneity between the groups was examined after randomization, and double blinding was applied such that the participants and assessors were blinded to the group assignment. The experimental group received the resistance circuit training program, while the control group received the usual resistance exercise program with no time limit. Both groups participated in the respective exercise programs for 8 weeks, twice per week, and evaluations were performed pre- and post-training (Fig. 1).
Training intervention
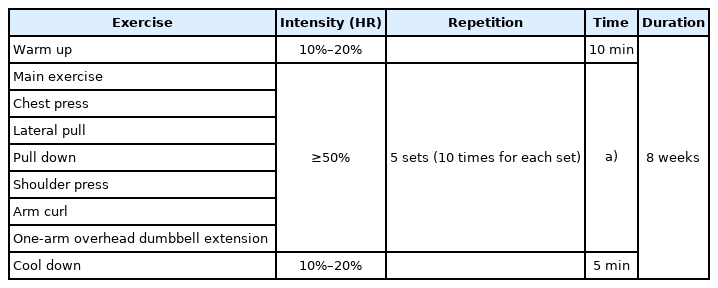
The resistance circuit training program applied to the experimental group comprised warm-up, main exercise, and cool-down. Warm-up and cool-down exercise involved 5–10 minutes of low-intensity wheelchair propelling and stretching activities of neck and shoulder girdle muscles. There were six main exercises in the following order: chest press, lateral pull, pull down, shoulder press, arm curl, and one-arm overhead dumbbell extension (Fig. 2). Resistance was set to ≥50% of one repetition maximum (RM) and measured at each exercise equipment. Five sets of 10 repetitions were performed for each movement and resistance was increased each week by 5%. There was no rest between movements, and the resting time between sets was limited to 1 minute. The total exercise duration per session was 30 minutes (Table 1).

Six main exercises that were included in the circuit resistance training program of exercise group: (A) chest press, (B) lateral pull, (C) pull down, (D) shoulder press, (E) arm curl, (F) one-arm overhead dumbbell extension.
The exercise intensity was set based on the HR measured during exercise and rate of perceived exertion (RPE). The target HR was calculated using the Karvonen formula. The target was set at 10%–20% of maximum HR during warm-up and cool-down and at ≥50% of maximum HR during the main exercises. RPE 11–13 was set as the upper limit for all exercises.
The exercise sequence and intensity were identical in both groups, but the control group had no limit on the resting time between movements and sets and was allowed to rest until comfortable. The total exercise duration per session varied for individuals but took approximately 50 minutes (Table 2).
Assessment
The participants were evaluated for each outcome variable before and after the exercise programs (Supplementary Table S1). The participants’ muscle mass, fat mass, and body fat percentage were measured using bioelectrical impedance analysis (InBody S10; Biospace Co., Seoul, Korea). Using isometric test equipment (HUR, Kokkola, Finland), participants’ pull-up, pull-down and bilateral chest press strength was measured. Muscles for these movements are important in people with paraplegia to move their wheelchairs and should be trained to prevent shoulder injuries [11]. Muscular endurance was measured using an arm-curl machine designed for people with disabilities (Kaesun Sports, Goyang, Korea). The participants were asked to sit on the equipment in an upright posture, and the maximum weight that the participants could lift at a time (1RM) was measured. The load was then set to 60% of measured RM, and the participants were asked to perform elbow flexion and extension for 1 minute with this load. The maximum number of arm curls performed was documented before and after the intervention with the load of initial assessment. To measure the participants’ endurance, the maximum distance moved for 6 minutes was measured before and after the intervention. This test was used to assess aerobic fitness in people with disabilities who use wheelchairs. It is easy to use in the clinic, and a 6-minute propulsion distance is a highly reliable and valid tool that reflects and predicts the fitness level (high vs. low) [12,13]. Wireless MIO GO (MIO, Beijing, China) was used to monitor the HR during exercise. The participants were asked to wear MIO GO on their wrists, and their HR was monitored to measure HR changes during exercise. The HR data were saved automatically every 15 seconds, and the data saved on MIO GO were transferred to a PC after the exercise.
Statistical analysis
All statistical analyses were conducted using SPSS software (21.0 version; IBM Corp., Armonk, NY, USA), and the means and standard deviations of all variables were calculated. Two-way repeated measures analysis of variance was used to detect differences in efficacy between the two groups and paired-sample t-tests were performed to assess within-group differences (pre-and post-intervention). The level of significance was set as p<0.05 for all statistical analyses.
RESULTS
The participants were recruited in April and May, and a pre-study evaluation was performed between June 10 and June 30, 2019. Twenty-two individuals who satisfied the selection criteria (18 male and four female) were recruited. The participants were randomly assigned to the experimental and control groups (n=11 each). None of the participants showed any adverse reactions during the study.
General characteristics
Demographic and baseline characteristics of the participants are listed in Table 3. Age, time since injury, height, body weight, BMI did not differ between the two groups.
Body composition
The muscle mass, fat mass, and body fat percentage did not differ significantly between the two groups. Although muscle mass increased significantly in the right (p=0.028) and left (p=0.028) arms after the intervention in the experimental group (Table 4), no significant difference was noted in either leg. Moreover, the control group did not show significant differences in any of the variables. The change in muscle mass in the right (p=0.017) and left (p=0.018) arms demonstrated significant inter-group differences, but no significant difference was observed for either leg.
Blood pressure and heart rate
Significant within-group differences in the systolic blood pressure (p=0.001) and diastolic blood pressure (p=0.002) were noted in the experimental group (Table 5). However, no significant within-group differences were observed in the control group. Although there was no significant inter-group difference in the systolic blood pressure, the difference in diastolic blood pressure was significant (p=0.009). There were no significant withingroup or inter-group differences in the resting HR before and after the intervention.
Muscle strength
Pull up and down
Pull-up weight increased from 52.12±20.23 kg to 62.56± 20.28 kg after 8 weeks in the experimental group (p=0.005). For pull-down, the weight increased from 35.11±15.39 kg to 44.86±15.40 kg (p=0.001).
Pull-down weight decreased from 37.24±16.38 kg preintervention to 33.28±13.70 kg post-intervention (p=0.031), but no significant difference was noted in pull-up weight in the control group. There were significant inter-group differences in the pull-up weight (p=0.003) and pulldown weight (p=0.001) (Table 4).
Chest press
In the experimental group, chest press weight on the right side significantly increased from 46.06±18.00 kg pre-intervention to 55.55±18.96 kg post-intervention (p=0.042). Chest press weight on the left side also increased from 43.46±24.78 kg to 55.87±27.15 kg post-intervention (p=0.039). In the control group, the chest press weight did not change significantly on either side. Intergroup differences in the chest press weight were significant for the right (p=0.024) and left (p=0.019) sides (Table 4).
Muscular endurance
In the experimental group, the number of arm curls on the right side increased from 35.90±9.06 pre-intervention to 51.09±12.19 post-intervention (p=0.003). On the left side, the number increased from 38.90±11.22 to 50.81±12.55 (p=0.001). The number of arm curls did not change significantly on either side in the control group. Inter-group differences in arm curls were significant for the right (p=0.010) and left (p=0.001) sides (Table 4).
Cardiopulmonary endurance (6-minute propulsion test)
No significant within-group difference in the distance moved was noted in either group (Table 5). Differences between the groups were not statistically significant.
Safety
None of the participants showed autonomic adverse events (hypotension, autonomic dysreflexia), musculoskeletal side effects, or discomfort during exercise.
DISCUSSION
The main finding of this study was that resistance circuit training program resulted in significant decrease in resting blood pressure and improvement in upper extremity muscle mass, strength, and endurance. In addition, significant differences were noted compared to conventional resistance exercise program. Also, during exercise, HR and RPE were monitored, and no adverse effects were observed.
In this study, resistance circuit training was selected as an exercise modality for patients with paraplegia as it can have both aerobic and anaerobic effects. Moreover, since the sequence of movements is interesting, circuit training can offer a solution for lack of interest. Because the rest between exercises is short in circuit training, it is highly time-efficient. For people with spinal cord injury who simultaneously experience decrease in the number of active muscles, strength of muscle contraction and cardiopulmonary endurance, a circuit training program comprising resistance movements can effectively improve physical health.
The exercise programs applied to the experimental and control groups were different only in terms of the resting interval between sets, which helped us understand how differences in the resting interval influence general physical capacity, including aerobic capacity.
A previous study divided 66 non-spinal cord injury individuals aged >65 years into two groups and applied 12 weeks of resistance circuit training (three times per week) only to the experimental group, while the control group did not receive any exercise training [14]. Compared to the control group, the experimental group showed a significant increase in the lean body mass and significant decrease in the fat mass. In another study, 35 non-spinal cord injury participants were divided into experimental and control groups and 12 weeks of concurrent aerobic and resistance circuit exercise training (three times per week) was applied to the experimental group, while the control group did not receive any exercise intervention [15]. When both groups were compared, the experimen tal group showed a significant reduction in body fat (16%, p<0.01). However, in the present study, no significant change in the fat mass and body fat percentage was noted in either group. This may be because the total program duration and exercise time in the present study (8 weeks, twice per week) were shorter than those in the previous studies (12 weeks, thrice per week). It has been suggested that although studies which applied exercise programs twice per week did not observe changes in body weight or composition, a study that applied the programs three times or more per week found significant changes [16]. They reasoned that exercise programs offered twice per week do not provide sufficient continual stimulation for inducing changes in the body composition. A meta-analysis reported that the overall effects of exercise programs in obese individuals were observed when programs were offered four times or more per week for ≥12 weeks. Furthermore, the effects increased with increasing duration and most studies applied the intervention for 12 weeks [17].
Similar to body composition, changes in overall muscle mass were not observed in our study. However, although there was no change in the lower extremity, muscle mass increased significantly in both arms in the experimental group, and inter-group differences were also significant. Exercise provides the main anabolic stimulus to skeletal muscle, and acute bouts of resistance exercise induce protein synthesis that exceeds protein breakdown, improving the net protein balance [18]. The exercise program in our study comprised movements targeting the upper extremity muscles. Through adequate load delivery to the exercising muscle fibers, a net protein balance was created, which may have improved muscle strength and mass in the upper extremities. Nevertheless, no significant change in the overall muscle mass was observed, which can be explained by the difference in the muscle mass between the upper and lower extremities. Muscle mass in the lower extremities was found to be 2- to 2.5- fold higher than that in the upper extremities. Therefore, although the upper extremity muscle mass increased significantly in our study, these changes may not have significantly increased the overall muscle mass.
The experimental group showed significant reductions in the systolic and diastolic blood pressure pre- and postintervention. A significant decrease in the diastolic blood pressure was also noted in the inter-group comparison. However, no significant difference was noted in the resting HR. A previous study also reported no significant changes in the resting HR, systolic blood pressure, and diastolic blood pressure in the experimental and control groups pre- and post-intervention [15]. Conversely, another study reported that the brachial blood pressure and central blood pressure decreased significantly, while vascular structure and function improved in participants following 4 weeks of circuit training. The authors concluded that a decrease in the central blood pressure decreased vascular resistance, thereby affecting the improvement in endothelial function and structure. They also reported that these changes can delay the progression of cardiovascular diseases, including atherosclerotic diseases, and have a positive impact on cardiac-related mortality [19]. The present study also observed significant reductions in systolic and diastolic blood pressure in the experimental group after the exercise program. Consistent with previous studies, such reductions in blood pressure could decrease vascular resistance and improve endothelial function and structure, thus contributing to a decreased risk of cardiovascular diseases.
The results of assessing pull up, pull down and chest press, which assess muscle strength; and arm curl, which assesses muscular endurance, showed that all variables increased significantly in the experimental group. One research group previously applied 12 weeks of circuit training three times a week and reported a 12%–30% increase in the muscle strength for all movements [20]. Similarly, another group applied 6 weeks of resistance circuit training and reported significant improvements in elbow flexion and extension strength in the experimental group [21]. In another study, women over 60 years of age received 10 weeks of circuit training (three times per week) and significant improvement in the participants’ muscle strength and muscular endurance (27.8%–40%) was observed [22]. Following resistance circuit training, muscle strength and endurance improves through neural adaptation in the first 3–5 weeks and muscular hypertrophy thereafter. The present study demonstrated significant improvement in the muscle strength, muscular endurance, and upper extremity muscle mass after 8 weeks. After 3–5 weeks, neural adaptation and hypertrophy of the targeted muscles occur, which may lead to significant increases in the muscle strength and muscular endurance.
In the 6-minute propulsion test assessing cardiopulmonary endurance, no difference was noted in both groups pre- and post-intervention. Although previous studies [20,23] applied resistance circuit training in people with paraplegia and observed improvement in cardiopulmonary endurance (10.4%–29.7% in peak oxygen uptake), the present study did not observe significant changes in the 6-min propulsion test. Previous studies limited the resting interval between sets to 10–15 seconds and set the intensity to 50% of 1RM or higher. The intensity was increased by 5% each week, and 1RM was reevaluated every 4 weeks to reset the intensity accordingly. In the present study, the resting interval between sets was relatively long at 1 minute. Moreover, although the intensity was increased by 5% each week, the upper limit of intensity was set to RPE 11–13 (light to somewhat hard). If the resting interval between sets and exercise intensity are modified, the results may be similar to those of previous studies.
We also evaluated potential autonomic adverse events and skin and musculoskeletal injuries during exercise, as well as other adverse events. Exercise prescriptions and guidelines for individuals with spinal cord injuryrelated disabilities recommend 5–15 minutes of warm-up exercise before the main exercise to prevent cardiac and musculoskeletal injuries and emphasize that the exercise should be prescribed and implemented cautiously after considering factors such as myocardial atrophy, HR and blood pressure abnormalities, pressure ulcers, and musculoskeletal anomalies which restrict exercise in people with spinal cord injury and increase the risk of secondary safety incidents [24].
This study had several limitations. First, clinical meaningfulness should be supported by studies with larger sample sizes. Second, the duration (8 weeks) and total number of sessions (16 sessions) were insufficient. Third, there were no anthropometric measurements. Fourth, cardiopulmonary endurance was only assessed based on the 6-minute propulsion distance, and the VO2 peak value was not measured. Subsequent studies should also assess the oxygen consumption. Fifth, we suggest future studies combining diet plans with exercise programs for body weight loss. These issues should be addressed to develop standardized exercise programs and home training programs for community-dwelling individuals with paraplegia caused by spinal cord injury.
In conclusion, the present study showed that compared to the usual resistance exercise program, resistance circuit training demonstrated significant beneficial effects including decreases in the resting blood pressure and increases in the muscle mass, strength, and endurance of the upper extremities, despite the same exercise duration excluding the resting interval. Furthermore, considering that no notable adverse events were observed despite applying moderate- to high-intensity circuit exercise program in people with upper thoracic cord injury, resistance circuit training exercise programs may be considered safe for people with paraplegia from spinal cord injuries regardless of the level of injury.
Notes
No potential conflict of interest relevant to this article was reported.
Conceptualization: Lee HJ. Methodology: Son MK, Lee HJ, Lee BS. Formal analysis: Son MK, Kim EY, Yun HY, Kim SJ, Kim JH, Jin SM, Eun SD. Funding acquisition: Lee HJ. Project administration: Kim SJ, Kim JH, Jin SM. Visualization: Son MK, Lee HJ, Kim EY, Yun HY. Writing - original draft: Son MK. Writing - review and editing: Son MK, Lee HJ, Lee BS. Approval of final manuscript: all authors.
Acknowledgements
This study was supported by a grant (No. 19-TB-04) from the Rehabilitation Research & Development Support Program, Korea National Rehabilitation Center, Ministry of Health and Welfare, Korea.
SUPPLEMENTARY MATERIALS
Supplementary Materials can be found via https://doi.org/10.5535/arm.22012.
Information about the assessment devices