The Significance of Transcutaneous Continuous Overnight CO2 Monitoring in Determining Initial Mechanical Ventilator Application for Patients with Neuromuscular Disease
Article information
Abstract
Objective
To reveal the significance of continuous transcutaneous carbon dioxide (CO2) level monitoring through reviewing cases which showed a discrepancy in CO2 levels between arterial blood gas analysis (ABGA) and continuous transcutaneous blood gas monitoring.
Method
Medical record review was conducted retrospectively of patients with neuromuscular diseases who had started home mechanical ventilation between June 2008 and May 2010. The 89 patients underwent ABGA at the 1st hospital day, and changes to their CO2 level were continuously monitored overnight with a transcutaneous blood gas analysis device. The number of patients who initially appeared to show normal PaCO2 through ABGA, yet displayed hypercapnea through overnight continuous monitoring, was counted.
Results
36 patients (40.45%) presented inconsistent CO2 level results between ABGA and continuous overnight monitoring. The mean CO2 level of the 36 patients using ABGA was 37.23±5.11 mmHg. However, the maximum and mean CO2 levels from the continuous monitoring device were 52.25±6.87 mmHg and 46.16±6.08 mmHg, respectively. From the total monitoring period (357.28±150.12 minutes), CO2 retention over 45 mmHg was detected in 198.97 minutes (55.69%).
Conclusion
Although ABGA only reflects ventilatory status at the puncturing moment, ABGA results are commonly used to monitor ventilatory status in most clinical settings. In order to decide the starting point of home mechanical ventilation in neuromuscular patients, continuous overnight monitoring should be considered to assess latent CO2 retention.
INTRODUCTION
In patients with neuromuscular disorders that are characterized by respiratory failure resulting from restrictive pulmonary diseases caused by respiratory muscle weakness, assessing the partial pressure of blood carbon dioxide is crucial to evaluate ventilatory condition.1 Arterial blood gas analysis (ABGA) is known to indicate the partial pressures of blood oxygen and carbon dioxide accurately.1,2 On the other hand, ABGA values are indicated only at the time point of measurement, and further to this, patients feel pain due to the invasiveness of the method, which may lead to hyperventilation or apnea. In such cases, results may not reflect patients' usual ventilatory condition and it is also significant that sleep hypoventilation is a common symptom in patients with neuromuscular disorders.3-5 Thus normal values from ABGA do not necessarily indicate a normal ventilatory condition at all times. As the case stands, there is a need to analyze ventilatory conditions seriately by use of transcutaneous blood gas analysis.6 In the department of rehabilitation medicine at Gangnam Severance hospital, serial measurements were made of the ventilatory conditions of patients with suspected respiratory failure or with underlying diseases, by use of ABGA and a transcutaneous blood gas analysis device, the SenTec Digital Monitor System with V-Sign™ Sensor (Sentec AG, Therwil, Switzerland), on the premise that ABGA does not sufficiently reflect usual ventilatory conditions. The aim of this study is to assess the importance of serial analysis of ventilatory conditions in decision-making about artificial ventilatory support in patients with neuromuscular disorders who have undergone ABGA and serial transcutaneous blood gas monitoring in their sleep before ventilator application.
MATERIALS AND METHODS
Subjects
155 patients with neuromuscular disorders and respiratory failure to whom ventilators were prescribed and applied at Gangnam Severance Hospital Seoul, Korea between June 2008 and May 2010 were studied. From these 155 patients, however, 66 were excluded. In the case of 40 exclusions, breathing patterns in sleep were analyzed by end-tidal carbon dioxide (ETCO2) monitoring instead of transcutaneous monitoring of PCO2. For the other 26, original medical records relating their continuous respiratory patterns in sleep were lost, so accurate analysis of the data was impossible. 89 patients who underwent both ABGA and continuous monitoring of Ptc(trans-cutaneous)CO2 on the same day and whose medical records were preserved were eligible for the study.
Methods
Transcutaneous measurements of oxygen and carbon dioxide are based on the principle that a heating element of the sensor, which is attached to the ear lobe, elevates the temperature of the underlying tissues to 43 degrees Celsius. This increases capillary blood flow and the partial pressure of oxygen and carbon dioxide, and makes the skin permeable to gas diffusion. Chemical values, including the potential of hydrogen (pH), are electrically analyzed through a highly penetrable membrane, wherewith the partial pressures of oxygen and carbon dioxide are calculated.7 The zero point is set automatically when the sensor is connected to the device. Recording of data starts when the sensor is separated from the device for monitoring and stops when the sensor is reconnected to the device for calibration, thus the continuous data are saved as one complete file. The values are displayed in real time on the device. The cumulative data are sent to the device, and time distribution of mean, maximum and minimum values are organized in tables and charts automatically (Fig. 1).
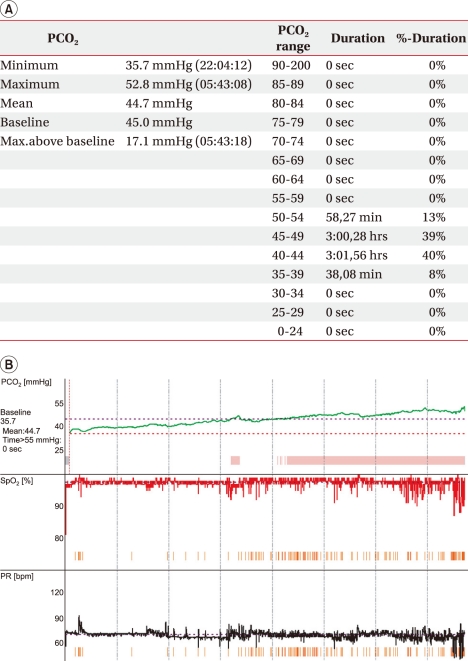
These figures show an example of a patient's data from the transcutaneous blood gas monitoring device. (A) Table and (B) graph of a patient's data from continuous transcutaneous blood gas monitoring. The table shows mean, maximal PCO2 values and portions of PCO2 range, while the graph shows change in PCO2 level through overnight continuous monitoring.
On admission day, all targeted patients underwent both ABGA and continuous overnight monitoring of transcutaneous CO2 during sleep. We defined hypercapnia as partial pressure of arterial carbon dioxide (PaCO2)>45 mmHg,8-10 with ventilators being applied to cases of hypercapnia. In the case of those patients whose PaCO2 were normal on ABGA but were considered to be hypercapnic on overnight transcutaneous blood gas monitoring, medical records were analyzed retrospectively. The maximum and mean values of PaCO2 and the duration of hypercapnia during overnight monitoring were also calculated. The symptoms and signs of hypoventilation caused by pulmonary insufficiency, which include sleep disorder, headache, confusion and lethargy, nightmare and anxiety,11 were evaluated in all targeted patients. We also verified the reduction in hypercapnia and improvement of hypoventilation symptoms after application of the ventilator.
RESULTS
Features of control and experimental groups
The total number of enrolled patients was 89, of whom 53 showed hypercapnia as determined by analysis of both ABGA and overnight transcutaneous blood gas monitoring. Although ABGA was within normal range in the remaining 36 patients (40.45%), hypercapnia was observed on the overnight transcutaneous blood gas monitoring, which represented a marked discrepancy between the two studies.
The control group, who were hypercapic in both intra-arterial and transcutaneous blood gas monitoring, consisted of 37 men and 16 women and the mean age was 44.87±21.56. Their underlying diseases consisted of neuromuscular disease (20), motor neuron disease (14), tetraplegia due to spinal cord injury (1), and Guillain-Barre syndrome (1).
The experimental group consisted of 25 men and 11 women with a mean average age of 36.06±22.08. Their underlying disorders consisted of neuromuscular disease (20), motor neuron disease (14), tetraplegia due to spinal cord injury (1), and Guillain-Barre syndrome (1).
Ventilation in experimental group with normal PaCO2 on ABGA but hypercapnia on overnight transcutaneous blood gas monitoring
The ABGA results of the 36 patients who showed discrepancy between transcutaneous and arterial blood gases were investigated, with the mean PaCO2 being 37.23±5.11 mmHg. On overnight transcutaneous blood gas monitoring, the maximum value and mean value of PaCO2 were 52.25±6.87 mmHg and 46.16±6.08 mmHg respectively. The overnight transcutaneous blood gas monitoring was performed for 357.28±150.12 minutes, during which carbon dioxide partial pressure of over 45 mmHg occupied 198.97 minutes (55.69%).
Hypoventilation symptoms of the experimental group and improved ventilation after the application of mechanical ventilator support
Surveys were conducted on the symptoms of hypoventilation, including insomnia, daytime hypersomnolence, morning headaches, nightmare, and anxiety, for the 89 patients who needed the application of a mechanical ventilator before they underwent ABGA and transcutaneous monitoring. Symptoms of hypoventilation were observed in 20 patients (37.7%) among the 53 who were hypercapnic in both transcutaneous blood gas monitoring and ABGA and in 14 patients (38.9%) among the 36 whose ABGA fell within the normal range but in whom hypercapnia was observed on overnight transcutaneous blood gas monitoring.
Hypoventilation symptoms were eliminated in all 34 patients after the application of mechanical ventilator support
According to the overnight transcutaneous blood gas monitoring which was performed on the last hospital day for the experimental group, PaCO2 showed a maximum value of 38.48±7.41 mmHg and a mean value of 32.73±6.87 mmHg, indicating that, hypercapnia was not observed. In the control group, the maximum value and the mean value of PaCO2 were 58.97±9.41 mmHg and 49.54±8.61 mmHg respectively, before ventilator application. After the application of mechanical ventilator support, hypercapnia was resolved so that the maximum and mean PaCO2 decreased to 40.86±6.68 mmHg, 34.48±6.08 mmHg respectively.
DISCUSSION
Aggravation of pulmonary insufficiency causes a decrease in the total time of spontaneous ventilation without respiratory muscle fatigue in daily living. Likewise, a delay in treatment of pulmonary insufficiency may increase the burden of cardiovascular work, which can increase cardiovascular complications.12,13 In early-stage respiratory failure, mechanical ventilator support can resolve the fatigue of respiratory muscles. Therefore, early detection of respiratory failure and early application of mechanical ventilatory support is important.14 In particular, it is crucial to determine when ventilatory support should be given, because the lifespan of patients with restrictive pulmonary diseases derived from neuromuscular disorder can be lengthened by ventilatory support.14 In the case of such patients, hypercapnia occurs due to alveolar hypoventilation. The problem is that early-stage hypercapnia may occur without subjective symptoms.14 Accordingly, regular evaluation of hypercapnia and the initiation of ventilatory support in case of need is critical.
ABGA is known to be highly effective for measuring the partial pressures of oxygen and carbon dioxide and for evaluate ventilatory conditions.15 However, it is an invasive method that causes pain and thus may lead to hyperventilation, and moreover, it cannot be performed on sleeping patients. Furthermore, the data are indicated only at the time point of measurement. Altogether, it is not a sufficient tool for accurate analysis of respiratory failure.14,16-18 In particular, analysis of respiratory failure by ABGA is not suitable for patients with neuromuscular diseases accompanied by respiratory muscle weakness because in the daytime such patients show a low level of carbon dioxide due to hyperventilation, but overnight, their supine posture decreases lung capacity and weakens spontaneous respiration. Therefore, continuous monitoring of ventilation during sleep is crucial.
The aim of this study was to research the utility of continuous overnight transcutaneous blood gas monitoring, which was conducted in 36 patients whose hypercapnia was not observed on ABGA but was observed on the transcutaneous blood gas monitoring, from a total group of 89 patients with chronic respiratory failure caused by respiratory muscle weakness, such as hypercapnia, who needed ventilators. These 36 patients' differing results might have been because the tests were affected by postures, sleep states, moods and mental states.4
In this study, patients whose hypercapnia was observed only on overnight transcutaneous blood gas monitoring comprised 40.45% of the total subjects. The times at which hypercapnia was observed occupied over 3 hours of the total sleeping time. This result suggests that 4 out of 10 patients who undergo ABGA may miss an opportunity to receive timely treatment. Considering that early-stage hypercapnia may be observed only during sleep, ventilation during sleep needs to be monitored and assessment should consider many factors that could influence ventilation, in order that respiratory failure may be detected early and treatment may be performed in time.
In the study of Storre et al., it was found that the carbon dioxide partial pressure, measured by overnight transcutaneous blood gas monitoring, was significantly related to that of ABGA6 and that the error between ABGA and a transcutaneous blood gas analyzer was 1.0±5.0 mmHg.2,6,19-24 This error is different from that of this study.23 The reason for this might be that values were measured at different times. The difference was not significant, but it is nevertheless very suggestive that hypercapnia lasted (198.97 out of 357.28±150.12 minutes; 55.69%) to the extent that a ventilator needed to be applied.
It is most effective to make a serial analysis of arterial blood gas by puncturing the artery, but this is highly invasive and thus may cause complications such as infection and hemorrhage. This method is hardly used, except in cases for which vital signs should be monitored. Instead, ETCO2 analysis and transcutaneous blood gas monitoring are widely used as measuring instruments.2,6,20 In the case of ETCO2 analysis, air may leak and the reliability may differ according to underlying diseases, leading to the wider usage of transcutaneous methods. Hinkelbein et al. and Bolliger et al. reported that transcutaneous methods were superior to the ETCO2 analysis in terms of reliability.2,19,20 In this study, a transcutaneous blood gas analyzer was used on the authority of the report of Storre et al.6,7,24,25
The limitation of this study is that carbon dioxide partial pressure was analyzed by a retrograde method using medical records, and thus respiratory rates could not be reflected. The respiratory rate is not displayed on the transcutaneous blood gas analyzer, and it was also not recorded during ABGA. As a result, the occurrence of hyperventilation or apnea could not be monitored. Nevertheless, this study confirmed that serial overnight transcutaneous blood gas monitoring could compensate for the shortcomings of ABGA. For the present, however, it was impossible to clarify the reason for which ABGA and overnight transcutaneous blood gas monitoring showed different results. Another problem is that this study was conducted without a control group from the normal population. Changes in body temperature were also not reflected, though the measuring instrument was sensitive to temperature. Mahutte et al. reported that the test became less reliable and that patients might be scalded if it was performed for over 4 hours,26 but other researchers have reported that measuring hours did not affect results significantly.7,21,27
CONCLUSION
The exclusive application of ABGA is insufficient to decide whether to apply mechanical ventilatory support. Considering that respiratory insufficiency may occur in recumbent patients with neuromuscular diseases, serial overnight transcutaneous blood gas monitoring is appropriate to evaluate their ventilatory conditions. Particularly in the case of patients whose diseases are more likely to cause respiratory muscle fatigue, carbon dioxide partial pressure should be periodically monitored in order that respiratory failure can be detected early. A further large-scale study should be conducted with various relevant indexes, including respiratory rates as well as the use of a normal control group.
ACKNOWLEDGEMENTS
This study was supported by a 2010 grant from VitalAire.