The Additive Effects of Hyaluronidase in Subacromial Bursa Injections Administered to Patients with Peri-Articular Shoulder Disorder
Article information
Abstract
Objective
To evaluate the additive effects of hyaluronidase combined with steroids in patients with peri-articular shoulder disorder.
Method
Thirty patients with peri-articular shoulder disorder were given subacromial bursa injections once a week for three consecutive weeks. Fifteen patients (Group A) underwent subacromial bursa injections with hyaluronidase 1,500 IU, triamcinolone 40 mg and 0.5% lidocaine (total 6 ml). Another fifteen patients (Group B) underwent the same injections with triamcinolone 40 mg and 0.5% lidocaine (total 6 ml). We examined the active range of motion (AROM) in the shoulder, used a visual analogue scale (VAS) for measurement, and administered a shoulder disability questionnaire (SDQ) at the commencement of the study and then every week until one week after the third injection.
Results
There were no significant difference between group A and B before the injections took place (p>0.05). Statistically significant improvement was seen in the VAS, SDQ, and AROM of flexion, abduction, internal rotation at one week after the first and second injections compared with the parameters measured at previous visits in both groups (p<0.05), except the SDQ between one week after the first and second injections in group B (p>0.05). Improvement in all parameters measured at one week after the third injection compared with the measurement values at one week after the second injection were not statistically significant in both groups (p>0.05). However, group A (the hyaluronidase group) showed significantly greater improvements than group B in terms of their SDQ and AROM of internal rotation scores one week after the three injections had taken place (p<0.05).
Conclusion
Peri-articular shoulder disorder patients who underwent subacromial bursa injections using hyaluronidase and steroids showed greater functional improvements than those who were given only steroid injections.
INTRODUCTION
Peri-articular shoulder disorder refers to a range of diseases, including subacromial-subdeltioid bursitis, calcific tendinitis and rotator cuff tendinopathy or tear. It typically causes shoulder pain and a limitation in terms of range-of-motion (ROM).1,2 A subacromial bursa injection is commonly used to relieve pain and to improve joint function in patients with periarticular shoulder disorder, and an injection of steroids and lidocaine is the most widely used.2-5 Yoon et al.2 suggested that, compared to a group of patients with peri-articular shoulder disorder who were administered with low dose steroids, the high dose group showed significant improvement in pain control, shoulder ROM and shoulder function. However, the higher dose group did also experience greater degeneration changes and more adverse events in metabolism and endocrine system function.2,6 There is some research related to the substitution of steroids with hyaluronic acid or combining them with adjuvants, but arguments about the effect of this still remain.7-9 It was shown that compared to steroid monotherapy, a combination of hyaluronidase and steroids, when injected into scar tissue, the nerve root, or injected intraspinally in patients with tuberculous arachnoiditis or with failed back surgery syndrome, achieved better treatment results.10-13 Seo et al.13 who specifically studied the shoulder joint, injected hyaluronidase and steroids into the articular cavity in patients with adhesive capsulitis and reported that there were significant improvements in pain relief and ROM, when compared to steroid monotherapy. However, there has been no research addressing subacromial bursa injections of hyaluronidase and steroids in patients with peri-articular shoulder disorder. This study therefore conducted subacromial bursa injections of steroids and hyaluronidase, a combination which is known to increase the local anesthetic absorption rate by modifying the permeability of the connective tissue, when compared with steroid monotherapy. We then, examined whether this combination therapy has further effects in the treatment of patients with peri-articular shoulder disorder.
MATERIALS AND METHODS
Subjects
Our study group comprised of patients who complained of shoulder pain and who came to our rehabilitation center from January to June 2011. The inclusion criteria were patients (1) who had a painful arc with Hawkin's sign or Neer's impringement sign; (2) who showed full or partial thickness rotator cuff tear or subacromial/subdeltoid bursitis in ultrasonographic testing, with definite lesions in the rotator cuff; and (3) who had limitations in terms of their active ROM with stiffness, but not to the extent that they met the exclusion criteria of having adhesive capsulitis. This condition is diagnosed when the patient has normal radiographic findings and when the active and passive elevation of arm are measured as being less than 100 degrees when the patient raises his arms over his head to the maximum possible extent; and, when the passive external rotation of the glenohumeral joint, which is measured while the examiner holds the patient's wrist and twists his elbow up to 90 degrees, is decreased by 50% or more compared to the less affected side. Other excluded patients were those who have had previous shoulder surgery; who have already had injections of steroids or hyaluronic acid for the current condition; who suffered from hemiplegic shoulder pain syndrome; and, who showed a suspected fracture in the radiologic findings. The selected eligible patients were randomly placed into A and B groups.
Subacromial bursa injections
We conducted physical examination and assessment of patients' shoulder pain and function. Specifically, we used ultrasound to examine lesions. We asked the patient to move the applicable arm for internal rotation and for hyperextension of the arm at a sitting posture placing the lower arm on the back. Then, we disinfected the area to be injected and performed subacromial bursa injections under ultrasonographic guidance. We injected a total of three times at one week intervals in both groups. The A group received 40 mg (1 ml) of triamcinolone acetonide (Dong Kwang Pharm., Seoul, Korea) and 3 ml of 1% lidocaine with 1ml of hyaluronidase H-lase® (Kuhnil Pharmaceutical, Seoul, Korea) and 1ml of normal saline. The B group received 40 mg (1 ml) of triamcinolone acetonide and 3 ml of 1% lidocaine with 2 ml of normal saline; there was a total of 6ml of injection material with an 0.5% lidocaine level for each group. One week prior to injection, patients were asked to suspend their administration of painkillers or anti-inflammatory drugs. They were taught to perform scapular stabilizer strengthening exercises and range of motion exercises at home after the injections; we continuously trained and recommended such exercises at every follow-up. There was no other physical therapy or drug treatment involved in this study.
Evaluation of injection effect
We evaluated subjects four times: once before their first injection, and one week after their first, second, and third injections. These evaluations were conducted by one examiner. This examiner asked patients to report the mean value of their degree of pain for the 24 hours prior to injection and measured with a visual analog scale (from zero to 10 points). He then measured the active ROM of patients' shoulder joints and did not limit scapula motion. For shoulder flexion and abduction measurement, he asked the patient to extend their elbow joints while sitting down and then measured the ROM of the upper limb in the sagittal and coronal planes. To assess internal and external rotation, the examiner measured the range of internal and external rotation that the patients had while in a sitting posture and externally rotating their shoulders at 90 degrees. The normal range of shoulder flexion and abduction was 180 degrees for both; for internal and external rotation, it was 90 degrees. To evaluate the shoulder function of our patients, we used a shoulder disability questionnaire (SDQ). This is a tool that can assess the degree of shoulder disorder that a patient reports. SDQ's validity and reliability have been verified. It is composed of 22 self-reporting items, with results scores ranging from zero (no disability) to 22 (greatest possible disability).14
Statistical analysis
We compared age, gender and lesion between two groups by using Chi-square and independent t-tests. We also compared measures before patients' first injection and one week after their first, second, and third injections in both the combination and monotherapy groups. We used Wilcoxon signed rank testing to compare the two groups at each timepoint. SPSS 12.0 was used, at the 0.05 level of significance.
RESULTS
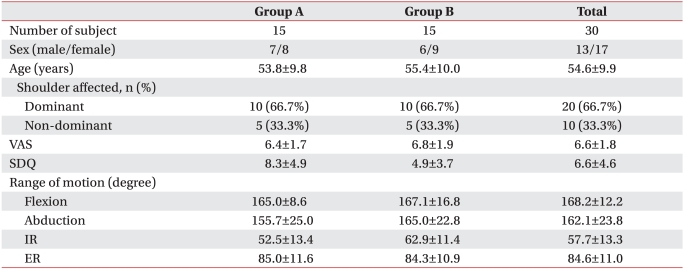
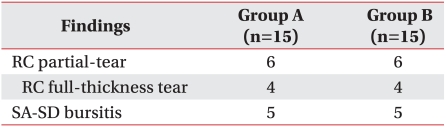
Characteristics and ultrasonic findings of subjects
The study examined 30 people; 15 patients in each group. There was no significant difference in patients' age, gender and lesion or in individual measures between the two groups before injections (Table 1). In addition, there was no significant difference in our pre-injection ultrasonographic findings (Table 2).
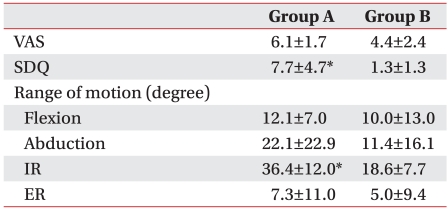
Changes in visual analog scale (VAS) of pain
In both groups, a significant improvement in VAS was observed after the first injection. Both groups also showed significant improvement after the second injection, as compared to their status after the first injection. There was no statistically significant improvement after the third injection compared to the point after the second injection (Table 3). However, the results after third injection showed that there were significant improvement in both groups, compared to pre-injection results, but that there was no statistically significant difference in improvement between the two groups (Table 4).
Changes in SDQ
In both groups, significant improvement in SDQ scores after first injection was observed. After the second injection, the A group showed statistically significantly improvement, but the B group did not. After third injection, there was no statistically significant improvement in either groups, compared to after the second injection (Table 3). However, the results after the third injection were significantly improved compared to pre-injection results for both groups, more so for group A than group B (Table 4).
Changes in the active ROM
Both groups showed statistically significant improvements in terms of flexion and internal rotation after the first injection, compared to their pre-injection results. Abduction was significantly improved only in the A group after the first injection. Both groups presented significant improvements in abduction after the second injection compared to their status after the first one; however, only the A group showed significantly improved in flexion. After the third injection, there was no statistically significant difference between the two groups, relative to their status after the second injection.
When comparing post-third injection results with pre-injection results, both groups showed statistically significant improvements in their flexion, abduction and internal rotation (Table 3). The A group showed better results in terms of their flexion, abduction and internal rotation after the third injection compared to their results before treatment. The degree of improvement in internal rotation was more statistically significant in the A group than it was in the B group (Table 4).
DISCUSSION
Subacromial bursa steroid injections are commonly repeated in patients with peri-articular shoulder disorder; however, there have been multiple debates about the appropriate number of injections, intervals and the correct dosage to be used.15-17 To examine appropriate doses of steroid, Yoon et al.2 conducted 1 subacromial bursa injection using 10 mg and 40 mg of triamcinolone and observed the results after 1, 3 and 6 weeks. This work found no difference in efficacy between the 1- and 3-week results; however, it reported significant improvements in pain, ROM and function when using 40 mg compared to 10 mg. To examine the optimum number of injections, Tillander et al.16 performed subacromial bursa injections using saline and triamcinolone, injecting these into healthy mice a total of eight times (three times at oneweek intervals and five times at two-week intervals) and examined histologic alterations in rotator cuff activity. They reported that after three injections of triamcinolone, there was no histological change in rotator cuff activity, but that there was fragmentation of collagen, necrosis, and local inflammation after eight repeated injections. In addition, Byun et al.6 studied the effect of repeated steroid injection in patients with hemiplegic shoulder pain and diabetes and concluded that the ideal method was to conduct three 40 mg triamcinolone injections at one-week intervals. Considering both stability and efficacy, this study therefore used three 40 mg triamcinolone injections administered at one-week intervals for our control group. However, there has been concern about potential degeneration changes or adverse metabolism and endocrine system events caused by high-dose steroids,2,6 which has led to new methods being developed that substitute steroids with hyaluronic acid or combine them with an adjuvant.7-9 This study conducted combination therapy using steroids and hyaluronidase, which is known to be an effective combination when used as a spinal root injection or for patients with adhesive capsulitis or peri-articular shoulder disorder, when compared to using steroid monotherapy. This study therefore aimed to examine whether or not the effect of hyaluronidase as an adjuvant increased when decreasing the number of steroid injections or whether there were adverse events caused by the injections.10-13
Hyaluronidase, which is a mammalian water-soluble enzyme secreted by the testis or the intestinal canal, hydrolyzes the glucosamic bond between hyaluronic acid and connective tissues so as to remove the interstitial barrier, thereby modifying the permeability of connective tissues and reducing the viscosity of intercellular interaction.18 As an absorption enhancer, it is subcutaneously injected into tissues with edema so that it relieves swelling and edema. Alternatively, it can be injected together with local anesthesia or steroids to increase permeability, and is therefore widely used in ophthalmology, gynecology and anesthesiology.19,20 Seo et al.13 injected hyaluronidase and steroids into the articular cavity in patients with adhesive capsulitis, comparing this to steroid monotherapy. They reported that there was no significant difference in VAS scores two weeks after injection, but that there were statistically significant improvement in abduction and external rotation among passive shoulder ROM. The current study differed in its subjects and methods compared to this study, because its focus was on patients with periarticular shoulder disorder and because it examined subacromial bursa injections. In addition, our study used 3 consecutive injections at 1-week intervals. However, in this study, no significant difference in VAS was also observed between the two groups; however, combination therapy did show statistically significant improvement of internal rotation measured by the shoulder function scale and active shoulder ROM than did the monotherapy. This suggests that hyaluronidase combined with steroids increases capillary permeability, which in turn facilitates the absorption of bursa fluid in subacromial bursitis and enhances the permeability of steroids into rotator cuff lesions in order to suppress the inflammation of the tendon around the lesion.
Between the second and third injections, both groups presented no statistically significant improvements in their VAS, on the shoulder function scale or in terms of their active ROM. When deciding on the appropriate number of steroid injections, further studies that observe various diseases and have a larger sample will be necessary. However, according to our results, patients with peri-articular shoulder disorder will benefit most from subacromial bursa injections of 40 mg triamcinolone administered two times.
As we studied patients with peri-articular shoulder disorder, we excluded patients with a capsular pattern. It is, however, difficult to identify early adhesive capsulitis because it is similar to shoulder impingement syndrome. Therefore, this study might be limited because it did not completely exclude patients who had early adhesive capsulitis. On the other hand, we selected patients who had definite lesions shown by ultrasonic findings and who experienced stiffness; these measures should have meant that patients with early adhesive capsulitis were likely to be excluded. Recently, methods for distinguishing early adhesive capsulitis through ultrasonographic testing have been developed,21,22 which may be useful for further studies such as ours when selecting eligible subjects. Another limitation may be that long-term effect of combination therapy is not clear due to our small sample size and short follow-up period. Therefore, further study in this area should have a larger sample size and extend the follow-up period.
CONCLUSION
Subacromial bursa injections of steroids (40 mg triamcinolone) and hyaluronidase in patients with periarticular shoulder disorder may have an additive effect in causing improvement of internal rotation active ROM and improving shoulder joint function.