- Search
| Ann Rehabil Med > Volume 41(5); 2017 > Article |
This article has been corrected. See Ann Rehabil Med. 2019 Feb 28; 43(1): 118.
Abstract
Objective
To perform a translation and cross-cultural adaptation of the Cardiac Rehabilitation Barriers Scale (CRBS) for use in Korea, followed by psychometric validation. The CRBS was developed to assess patients' perception of the degree to which patient, provider and health system-level barriers affect their cardiac rehabilitation (CR) participation.
Methods
The CRBS consists of 21 items (barriers to adherence) rated on a 5-point Likert scale. The first phase was to translate and cross-culturally adapt the CRBS to the Korean language. After back-translation, both versions were reviewed by a committee. The face validity was assessed in a sample of Korean patients (n=53) with history of acute myocardial infarction that did not participate in CR through semi-structured interviews. The second phase was to assess the construct and criterion validity of the Korean translation as well as internal reliability, through administration of the translated version in 104 patients, principle component analysis with varimax rotation and cross-referencing against CR use, respectively.
Results
The length, readability, and clarity of the questionnaire were rated well, demonstrating face validity. Analysis revealed a six-factor solution, demonstrating construct validity. Cronbach's alpha was greater than 0.65. Barriers rated highest included not knowing about CR and not being contacted by a program. The mean CRBS score was significantly higher among non-attendees (2.71±0.26) than CR attendees (2.51±0.18) (p<0.01).
Cardiovascular disease is one of the leading causes of death, and in Korea, deaths attributed to coronary artery disease are rising [1]. Cardiac rehabilitation (CR) is prescribed for patients with cardiac disease for secondary prevention, based on evidence that participation in CR reduces cardiovascular mortality when compared with patients not participating in CR [2]. Although the benefit of CR is well established, many cardiac patients do not attend CR [3]. Patient, provider, and health system-level barriers to CR utilization have been identified in the literature [4].
The English-language CRBS was developed to assess barriers to participation and adherence [5]. The items were developed based on literature review of multilevel barriers, and administered in a sample of cardiac patients to establish psychometric properties. The final version consists of 21 items, of which CR candidates are asked to rate their level of agreement with each item on a 5-point Likert scale, with response options ranging from 1 ‘strongly disagree’ to 5 ‘strongly agree’. Higher scores indicate stronger barriers to CR participation or adherence. The CRBS consists of four subscales: perceived need for CR/health care factors (9 items), logistic factors (5 items), conflict with work schedule/time (3 items), and comorbidities/functional status (4 items).
The CRBS has also been validated in the Brazilian Portuguese language [6], and translated but not validated in French, Spanish, Punjabi and Chinese [7]. To the authors' knowledge, the CRBS has not been translated into Korean. The purpose of this study is to perform a translation and cross-cultural adaptation of the CRBS for use in Korea, followed by psychometric validation.
This study is comprised of two parts: (1) translation and cross-cultural adaptation of the original English version of CRBS instrument into the Korean language and (2) the test of the psychometric properties of CRBS Korean language version (CRBS-K). The process of translation and cross-cultural adaptation of the CRBS to Korean was based on the 10 steps as described in the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Patient-Reported Outcomes Translation and Linguistic Validation Task Force guidelines [8]. The Institutional Review Board (IRB) of Seoul National University Bundang Hospital (IRB No. B-1508/312-119) and Kangwon National University Hospital (IRB No. KNUH-2016-09-014-001) approved this study protocol.
The first step was translation. The original version of the CRBS was initially forward-translated from English into Korean. The translations were performed independently by two translators that were native speakers of the Korean language. One of the translators had no medical background and the other translator was part of the medical team that participated in the study. These two translations were reviewed, and few discrepancies were reconciled by consensus. A synthesis version was created. The reconciled Korean version was back-translated into English by two bilingual native English speakers, that were Korean-Americans fluent in Korean (one translator was medical personnel, and the other translator was non-medical personnel), blinded to the original English version. An expert committee consisting of health professionals, translators, and linguists reviewed the source version and the back-translation for inequivalences, and adapted them to the most fitting meaning in Korean. This version was reviewed relative to linguistic and cultural qualities, by the expert committee. Discrepancies were resolved by consensus to achieve conceptual equivalence with the original questionnaire.
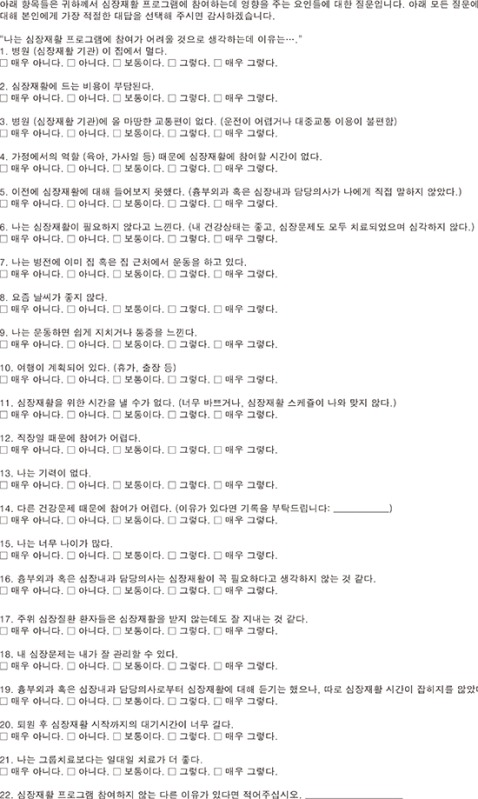
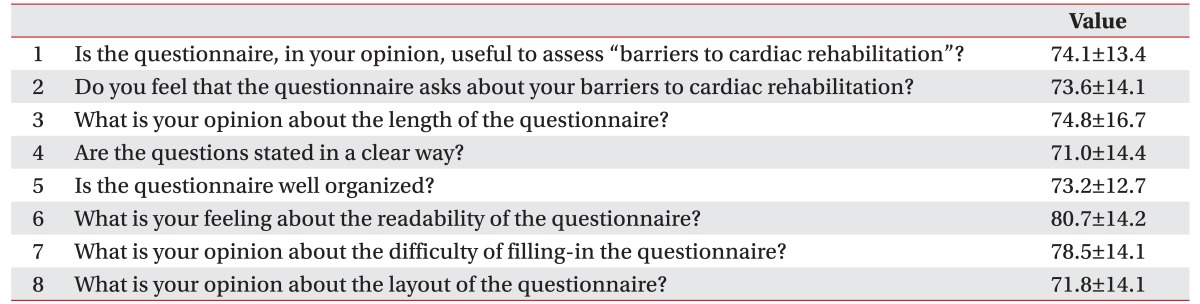
This pre-final version was field-tested in 53 Korean patients at Kangwon National University Hospital, for the cognitive debriefing phase. The authors used qualitative semi-structured interviews to ask patients about the questionnaire and their understanding of the questions. Interviewees were patients admitted because of acute myocardial infarction, underwent percutaneous coronary intervention (PCI) and had no problems with communicating (e.g., severe cognitive impairment, unstable medical condition). They were educated about CR by the coordinator according to the clinical pathway for acute myocardial infarction and interviews for cognitive debriefing were conducted after CR education during the admission period. Gender and age were recorded, as well as time necessary to complete the questionnaire. The semi-structured interview was based on eight questions (as listed in Table 1). All the questions were answered on a visual analogue scale (VAS) of 100 mm: ‘0’ means not useable at all and ‘100’ means very useable [9]. After cognitive debriefing, ambiguous expressions were modified via discussion. This final CRBS-K was reviewed by the expert committee.
Psychometric analyses were performed to assess the Korean version of the CRBS in a Korean sample (n=104 from Seoul National University Bundang Hospital). Participants consisted of cardiac inpatients diagnosed with acute myocardial infarction that underwent PCI. Patients were automatically referred to the department of rehabilitation medicine during the admission period and educated for CR program by the designated coordinator. CRBS was checked in patients referred for CR by the CR coordinator during admission. If patients agreed to participate in phase II of the CR program, they visited the outpatient clinic and were educated about the CR program a second time by the physiatrist one week after discharge. The symptom-limited cardiopulmonary exercise test (CPET) was arranged in 2 to 3 weeks, if participants did not have contraindications for symptom-limited CPET. After the symptom-limited CPET, patients visited the outpatient clinic the same day and an adequate exercise program was prescribed. Waiting time for monitored hospital-based phase II CR program after symptom-limited CPET was usually within 1 week and the start of CR program was delayed due to the patient's situation and not due to a limit in availability of the CR facility. Patients that attended one or more phase II hospital based monitored CR sessions within three months of discharge were considered CR attendees. Patients usually had to pay costs for CR and costs were not covered by the national insurance system. Home-based CR program was not provided to the subjects in our study.
Information about age, sex, education level, body mass index, ejection fraction, smoking status, work status, family history of coronary heart disease, past medical history of diabetes, hypertension and hypercholesterolemia was collected from subjects using interviews during admission or from the medical chart review.
The psychometric properties tested were as follows: (1) factor structure/construct validity through factor analysis, (2) internal consistency of identified factors, (3) criterion validity relative to CR participation. The construct validity was assessed through principle components analysis, and the factor structure rotated using orthogonal rotations (varimax). The suitability of factor analysis was determined by the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy, and Bartlett's sphericity test was also conducted. KMO values greater than 0.6 were acceptable. Factors with eigenvalues greater than 1.0 were extracted according to the Kaiser-Guttman criterion [10]. After factors were selected, a correlation matrix was generated using varimax rotation with Kaiser normalization. Factor loadings greater than 0.40 on only one factor were interpreted [11]. If an item loaded on multiple factors, then the factor with the highest loading was considered for interpretation. The internal consistency of the subscales was tested with Cronbach's alpha. Values ≥0.7 were considered satisfactory. To assess the criterion validity of the CRBS, independent samples t-tests were used to assess differences in mean total CRBS scores between CR attendees and non-attendees. Baseline characteristics were compared between CR attendees and non-attendees using independent t-test for continuous variables and chi-square test for categorical variables. SPSS ver. 21 (IBM, Armonk, NY, USA) was used for analysis. The level of significance for all tests was set at 0.05.
During the harmonization process for cross-cultural adaptation, all barrier items were applicable for the Korean context, therefore the Korean version of the CRBS also consisted of 21 items. During the translation and cross-cultural adaptation process, some items of CRBS required careful discussion to ensure the meaning was accurately translated. During face validation, many Korean patients considered ‘my doctor’ to be the resident in charge or consulting rehabilitation doctor. Therefore, we modified the term ‘my doctor’ to read ‘my cardiologist or thoracic surgeon’ in item CRBS_16. In both hospitals, CR referral is automatically conducted during the admission period in accordance with the established institutional pathway between the cardiac and rehabilitation departments, and there is minimal delay from admission to referral. Therefore, we modified the CRBS_20 to “it took too long to start the outpatient program after referral.” These translation and adaptation issues were discussed to achieve consensus. In the cognitive debriefing phase, 53 patients (38 [71.7%] male; mean age, 67.0±12.6 years) were asked to fill in the CRBS-K and the questionnaire assessing their understanding of the questions. The CRBS-K took less than 10 minutes to complete. Patients found the length, the readability, and the clarity of the CRBS-K satisfactory. The questionnaire was considered by patients to have a good layout and to be clearly organized (Table 1). In summary, 21 items were translated and validated (see Appendix 1).
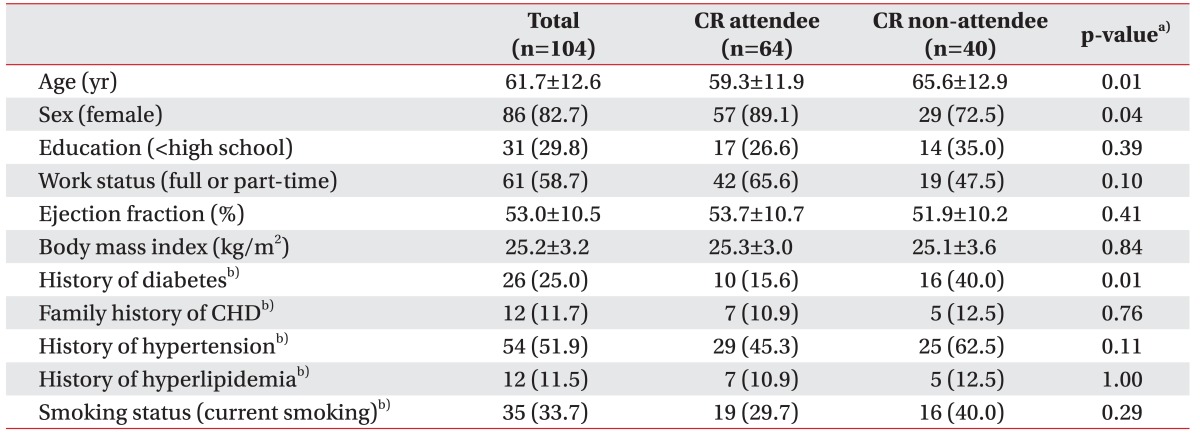
A total of 104 patients participated, of which 64 (61.5%) patients attended one or more CR sessions after discharge (i.e., attendees). CR attendees were significantly more often male and younger than non-attendees (Table 2).
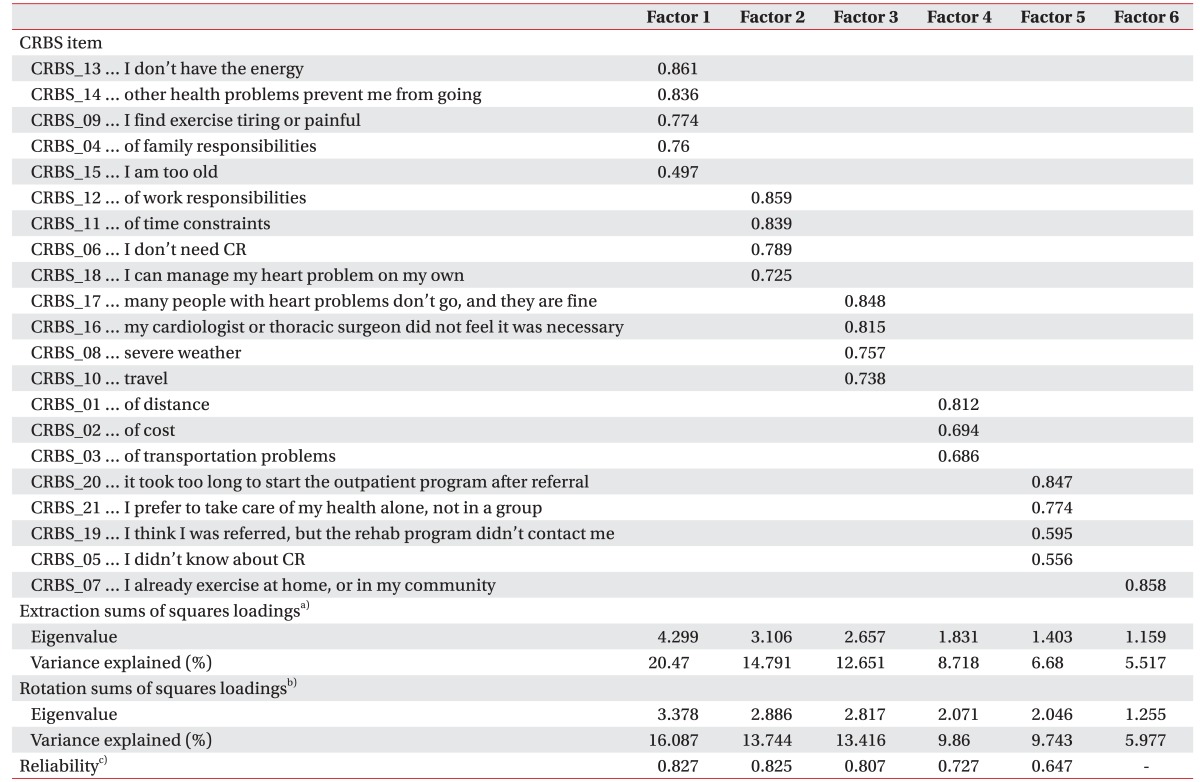
Construct validity was assessed using principle components analysis. The KMO value was 0.628 and Barlett's test was significant (p<0.05). Six factors with eigenvalues greater than 1.0 were extracted, that explained 68.8% of total variance. Eigenvalue and percent of variance explained by each factor are listed in Table 2. The first factor reflects comorbidity/functional limitations. The second factor reflects perceiving other aspects of life as more significant than CR (i.e., work/time conflicts). The third factor consists of external factors impacting a patient (physician advice, weather). The fourth factor reflects logistical aspects such as distance, cost, and transportation. The fifth factor reflects health care system issues. The sixth factor consists of a single CRBS item: “I already exercise at home, or in my community.”
Internal consistency of most subscales (factor 1 to 4) of the CRBS-K revealed satisfactory internal consistency (Cronbach's alpha ≥0.7), except factor 5 (Cronbach's alpha 0.647). Factor 6 consists of a single CRBS item and therefore internal consistency is not applicable (Table 3).
Table 4 displays mean item, total and CRBS-K factor scores. As shown, the most commonly reported barriers were not knowing about CR and not being contacted by a CR program. More patient-related barriers that were commonly reported included preferring to care for their health independently, already exercising, and logistical factors (distance, cost transportation). The least commonly reported barriers were not needing CR and travel. The fifth factor (health care system issues) represented the most critical barrier to CR participation.
Criterion validity was assessed by testing differences in the total and subscale CRBS-K scores in CR attendees versus non-attendees. Total scores were significantly higher among non-attendees. Mean scores for three of the six subscales, namely comorbidity/functional limitations (factor 1), work/time/needs conflicts (factor 2), and logistical aspects such as distance, cost, and transportation (factor 4), were significantly higher among nonattendees than attendees, with a trend for the health care system factor (factor 5).
In this study, translation and cross-cultural adaptation of the CRBS into the Korean language was conducted in accordance with internationally-established guidelines [8]. The structure of the CRBS-K was identical to the original English version, and all 21 items were retained. Subsequently, the psychometric properties of the final Korean version were assessed, and the CRBS-K was a valid and reliable questionnaire to assess barriers to attending CR.
The CRBS was developed in Canada, and has been validated in English [5] and translated and validated in Brazilian-Portuguese [6]. This is the second study in which the scale was translated and validated outside Canada and the first study to conduct the psychometric validation outside Canada. In the original validation, four factors were identified (perceived need/health care factors; logistical factors; work/time conflicts; and comorbidities/functional status) [5]. In the Brazilian-Portuguese version, there were five factors [6]. In this study, principal component analysis revealed six factors, namely comorbidities/functional limitations; perceived need; external factors (similar to work/time conflicts); logistical factors; healthcare system factors; and already exercising. There are similarities in subscales between the original English and Korean version. However, “many people with heart problems don't participate and they are fine”, “my doctor did not feel it was necessary”, “severe weather”, and “travel” were included in subscale 1 to 3 in the English version, but these items were included in the additionally extracted factor 3 (Table 3) in the Korean version. This suggests that cardiac patients in this study perceived those external factors as separate barriers to CR participation. The difference between the number of factors may be attributable to the different medical systems and cultural differences between Canada, Brazil and Korea. However, overall, the factors were consistent across versions (i.e., comorbidity/functional limitations; work/time conflicts; logistical factors), suggesting the factor structure of the scale is viable.
In addition to satisfactory construct validity, internal consistency was satisfactory for all subscales, except somewhat low internal consistency for factor 5 (health care system factors). The mean CRBS-K score among CR non-attendees was significantly higher than that among CR attendees, establishing the criterion validity of the scale. Although not assessed herein, the test-retest reliability was acceptable in both previous validation studies (intra-class correlation coefficient = 0.64 [5] and 0.68 [6]). Overall, the results of this study are consistent with those presented in the original validation [5].
Cardiovascular diseases are the leading cause of death worldwide, and have significantly risen in Korea [1]. CR reduces mortality and morbidity. Despite these benefits, participation in phase II CR is low. In Korea, regional cardio-cerebrovascular centers have been established in 11 areas, and CR units comprise an essential part of all these regional centers. To ultimately improve CR participation, more investigations are needed to establish the key CR barriers across all centers. If the same barriers are identified in a more generalizable sample, mitigation strategies may be used, such as improving patient education about CR at bedside, as well as allocating CR staff personnel to contact newly-referred patients.
Limitations of this study need to be addressed. First, some sociodemographic characteristics were not equivalent between CR attendees and non-attendees, and this may be an alternative explanation for the differences in CRBS scores between attendees and non-attendees. Not many sociodemographic or clinical characteristics were collected, given the purpose of the study was chiefly development and validation, and there may be unmeasured differences between groups that can explain the differences in CRBS scores. However, this is not likely, since the English version of the scale differentiated between CR attendees and non-attendees. Second, this study did not investigate barriers to CR adherence, although CRBS was developed to identify barriers to participation and adherence to CR programs. Finally, CRBS was only checked during the admission period. This timing of the CRBS interview may explain the higher mean scores in the item of “I didn't know about CR” and “I think I was referred, but the rehab program didn't contact me”. Barriers of CR use were assessed during admission because this assessment was needed for CR attendees and non-attendees. However, barriers may be differently identified after discharge. There is a need for further investigation of the CRBS interview after discharge or initiation of phase II CR to assess barriers in the outpatient setting.
In conclusion, the CRBS Korean version (CRBS-K) was developed through a rigorous translation and crosscultural adaptation process, and is demonstrated as valid and reliable for assessing for barriers to CR utilization in Korea. In Korean patients early after discharge, the most significant CR barriers included lack of awareness about CR, preferring to care for their health independently, already exercising, and logistical factors. Given the low rates of CR use in Korea, the broad administration of CRBS-K may assist in identification and mitigation of major barriers to CR.
CONFLICT OF INTEREST:
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
1. Statistics Korea. Cause of death statistics in Korea. Daejeon: Statistics Korea; 2014.
2. Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016;(1): CD001800PMID: 26730878.



3. King KM, Teo KK. Cardiac rehabilitation referral and attendance: not one and the same. Rehabil Nurs 1998;23:246-251. PMID: 10067639.


4. Grace SL, Krepostman S, Brooks D, Jaglal S, Abramson BL, Scholey P, et al. Referral to and discharge from cardiac rehabilitation: key informant views on continuity of care. J Eval Clin Pract 2006;12:155-163. PMID: 16579824.



5. Shanmugasegaram S, Gagliese L, Oh P, Stewart DE, Brister SJ, Chan V, et al. Psychometric validation of the cardiac rehabilitation barriers scale. Clin Rehabil 2012;26:152-164. PMID: 21937522.



6. Ghisi GL, Santos RZ, Schveitzer V, Barros AL, Recchia TL, Oh P, et al. Development and validation of the Brazilian Portuguese version of the Cardiac Rehabilitation Barriers Scale. Arq Bras Cardiol 2012;98:344-351. PMID: 22426990.


7. Shanmugasegaram S, Tang C, Tan Y, Chow CM, Oh P, Tomlinson GA, et al. A comparison of cardiac rehabilitation barriers in North American and Chinese-Canadian outpatients In: Toronto Rehab's 9th Annual Research Day; 2013 November; Toronto, Canada. Toronto, Toronto Rehabilitation Institute. 2013.
8. Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for Patient-Reported Outcomes (PRO) measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005;8:94-104. PMID: 15804318.


9. Timmerman H, Wolff AP, Schreyer T, Outermans J, Evers AW, Freynhagen R, et al. Cross-cultural adaptation to the Dutch language of the PainDETECT-Questionnaire. Pain Pract 2013;13:206-214. PMID: 22776283.


10. Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas 1960;20:141-151.

11. Field A. Discovering statistics. 2nd ed. London: Sage; 2005.