Effect of Vallecular Ballooning in Stroke Patients With Dysphagia
Article information
Abstract
Objective
To investigate the improvement of dysphagia after balloon dilatation and balloon swallowing at the vallecular space with a Foley catheter in stroke patients.
Methods
This study was conducted between May 1, 2012 and December 31, 2015, and involved 30 stroke patients with complaints of difficulty in swallowing. All patients underwent videofluoroscopic swallowing study (VFSS) before and after vallecular ballooning. VFSS was performed with a 4 mL semisolid bolus. For vallecular ballooning, two trainings were performed for at least 10 minutes, including backward stretching of the epiglottis and swallowing of a balloon located in the vallecular space, by checking the movement of the Foley catheter tip in real time using VFSS.
Results
After examination of the dysphagia improvement pattern before and after vallecular ballooning, laryngeal elevation (x-axis: pre 2.62±1.51 mm and post 3.54±1.93 mm, p=0.038; y-axis: pre 17.11±4.24 mm and post 22.11±3.46 mm, p=0.036), pharyngeal transit time (pre 5.76±6.61 s and post 4.08±5.49 s, p=0.043), rotation of the epiglottis (pre 53.24°±26.77° and post 32.45°±24.60°, p<0.001), and post-swallow pharyngeal remnant (pre 41.31%±23.77% and post 32.45%±24.60%, p=0.002) showed statistically significant differences. No significant difference was observed in the penetration-aspiration scale score (pre 4.73±1.50 and post 4.46±1.78, p=0.391).
Conclusion
For stroke patients with dysmotility of the epiglottis and post-swallowing residue, vallecular ballooning can be considered as an alternative method that can be applied without risk of aspiration in dysphagia treatment.
INTRODUCTION
Swallowing involves the passive movement of the epiglottis by the force of the muscles attached to it, pulling the tip posteriorly so that it assumes a horizontal tilt and bends the tip downward [1].
The tip and sides of the epiglottis are primarily attached to the hyoid bone, while the base of the epiglottis is attached to the thyroid cartilage ligament. As the hyoid and thyroid cartilage are elevated during swallowing, the epiglottis moves to a horizontal and then inverted position, covering the arytenoids and vocal folds. The base of the tongue then presses against the lingual surface of the epiglottis, helping to squeeze out the contents of the valleculae [2].
Any deterioration of the epiglottis movement leads to the development of dysphagia. According to Garon et al. [3], the deterioration of epiglottic movement appears in stroke and Parkinson disease, chronic obstructive pulmonary disease (COPD), Alzheimer disease and muscular dystrophy, etc. Many epiglottic movement patterns have been described in the literature by earlier swallow researchers. The descriptions of abnormal epiglottic physiology includes no functional movement, incomplete inversion to a horizontal position, delayed tilt, oblique movement, and inconsistent neural innervation-epiglottic dysfunction during deglutition in patents with dysphagia [4].
Perlman et al. [5] mentioned that in their study that deterioration in the movement of the epiglottis was associated with the vallecular residue and increased aspiration risk. They also reported that epiglottis dysfunction is associated with reduced hyoid elevation. Several techniques have been suggested to alleviate the deteriorated movement of the epiglottis and hyoid bone movement, including the Shaker exercise and Mendelsohn maneuver. Recently, an attempt was made to induce hyoid bone elevation by attaching Kinesio Tape to the chin and neck [6]. These methods improve the mobility of the epiglottis by promoting the laryngeal elevation.
A study by Kim et al. [7] reports the improvement of the swallowing parameters, including reduction of the vallecular remnant and decrease in pharyngeal transit time, after backward stretching of the epiglottis through a ballooning procedure using a Foley catheter at the vallecular space in a patient with deteriorated kinetic movement of the epiglottis after intubation. The unique feature of this paper was that a swallowing improvement effect was obtained by imposing direct passive backward stretching using ballooning to the epiglottis, unlike other previous papers that focused on improving the hyoid bone movement.
This study was conducted in stroke patients with dysphagia, and investigated the improvement of the epiglottis rotation angle, laryngeal elevation, post-swallowing remnant, and pharyngeal transit time, which were caused by the increase in the motility of the epiglottis after the ballooning procedure, using a Foley catheter at the vallecular space.
MATERIALS AND METHODS
The study was approved by the Myongji Hospital Ethics Committee. The Institutional Review Board number is MJH-16-033.
Subjects
This study involved 30 stroke patients with complaints of difficulty in swallowing. They were admitted to the rehabilitation medicine department, and underwent vallecular ballooning between May 1, 2012 and December 31, 2015. The inclusion criteria were neurogenic dysphagia patients with cerebral hemorrhage and cerebral infarction with vallecular ballooning procedure. The exclusion criteria were as follows: (1) patients with anatomical abnormality in the epiglottis, as observed on laryngoscopy conducted before the procedure; (2) patients with a treatment history that might affect the epiglottis mobility, such as head and neck radiation therapy; and (3) patients with a history of epiglottitis.
Procedure
Videofluoroscopic swallowing study (VFSS) was performed before and after vallecular ballooning, with a 4 mL semisolid bolus. The semisolid paste was prepared as a 2:1 volumetric mixture of dysphagia formula level 1 (food should be pudding-like without lumps, chunks, or pulp) and contrast barium solution (Solotop-HD; Taejoon Pharm Co. Ltd., Yongin, Korea). For the contrast solution, 375 g barium sulfate powder was mixed with 90 mL water. The VFSS test was done in the chin-tucked position for all the patients while they were sitting in a reclining wheelchair.
For the vallecular balloon procedure, contrast medium was injected to the Foley after placement of a 16 F urethral catheter tip in the epiglottis vallecular space. Stretching and spreading of the epiglottis 10 times for 10 seconds per time, was done by ballooning up to 6 mL, while checking the balloon size with a VFSS image. Next, the patients had a 10-second break, and the same procedure was repeated three times. Additionally, the patients swallowed the balloon located at the vallecular space more than 20 times, which lasted for at least 10 minutes (Fig. 1). For the patients who were unable to follow the instructions due to cognitive decline, the swallowing reflex was induced by manual stimulation with the index and middle fingers after palpating the upper hyoid bone, after which the balloon swallowing was conducted.
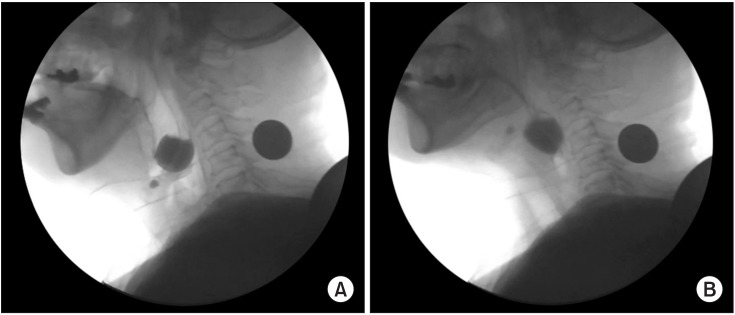
Vallecular ballooning. Contrast medium was injected into the balloon after inserting the tip into the vallecular space by checking the movement of the tip of the Foley catheter in real time using videofluoroscopic swallowing study. Two kinds of training were performed: backward stretching of the epiglottis (A) and swallowing of a balloon located in the vallecular space (B).
Every VFSS was recorded using a camcorder at a rate of 30 frames per second. All images were saved on a personal computer, and were analyzed with a multimedia player (Gretech, Seoul, Korea). Additionally, the laryngeal elevation, post-swallow pharyngeal remnant, and epiglottis rotation angle were measured with 2D screen AutoCAD (Autodesk, San Francisco, CA, USA). As the forward, backward, left and right movements of the patient during the VFSS test might affect the measurements of the remnant and width, to minimize the error the image size was readjusted based on the maximum length of a 100-won coin (23 mm in diameter) attached to the neck of a patient.
Laryngoscopic evaluation of the epiglottis
To identify any complications at the site where vallecular ballooning was imposed (including mucosal injury), evaluation was conducted with a fiberoptic rhinolaryngoscope (ENF-GP; Olympus Medical Systems, Tokyo, Japan) after the procedure.
Outcome measures
The swallowing parameters were measured as described in a previous study by Kim et al. [8]. For laryngeal elevation, the y-axis was a straight line drawn from the anterior-inferior margin of the 4th vertebral body to the anterior-inferior margin of the 2nd vertebral body. The x-axis was set perpendicular to the y-axis to measure the change (mm) in the location of the hyoid bone before and after swallowing (Fig. 2). The pharyngeal transit time was measured as the time (second) that it took for food to pass from the posterior nasal spine to the pharyngoesophageal sphincter. The post-swallow pharyngeal remnant was represented as the difference between the initial remnant and the remnant after swallowing the food once (Fig. 3). The degree of semisolid aspiration was measured using the penetration-aspiration scale (PAS). After the epiglottis rotation angle was checked with an imaginary line connecting the root and tip of the epiglottis, the angle change in the imaginary line before and after swallowing was measured. To reduce error, the angle change was measured based on a straight line connecting the anterior-inferior margin of the 4th vertebral body and the anterior-inferior margin of the 2nd vertebral body (Fig. 4).

Laryngeal elevation. The zero point was defined as the anterior-inferior margin of the 4th cervical vertebral body, the y-axis as the straight line connecting the zero point with the anterior-inferior margin of the second cervical vertebral body, and the x-axis as the line perpendicular to the y-axis. Hyoid bone at the position of the resting state (A) and most highly raised position during swallowing (B).

Post-swallow pharyngeal remnant. The difference in the remnant (%) was measured before and after swallowing, using an AutoCAD 2D screen. Remnant before swallowing (A) and remnant after swallowing (B).
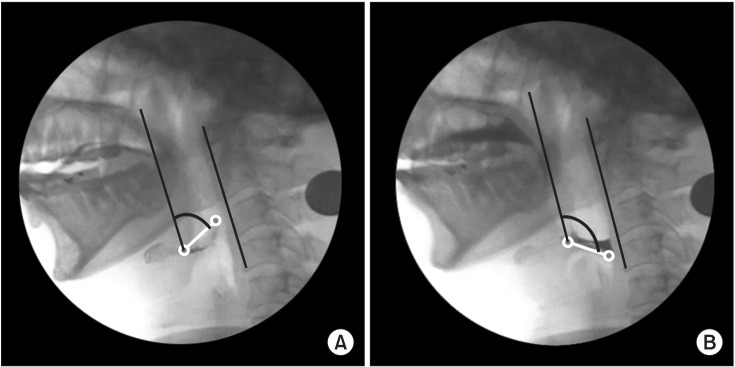
Epiglottis rotation. The maximum angle change in the line connecting the root with the tip of the epiglottis before and after swallowing was measured. To reduce error, a straight line linking the anterior-inferior margin of the 4th vertebral body and the anterior-inferior margin of the 2nd vertebral body was used as a baseline. Before swallowing (A) and maximum angle during swallowing (B).
Statistical analysis
All statistical analyses were performed with the SPSS ver. 18.0 (SPSS Inc., Chicago, IL USA). Statistical significance was confirmed with the paired t-test for comparing the results before and after the balloon treatment. A p-value <0.05 was considered to be statistically significant.
RESULTS
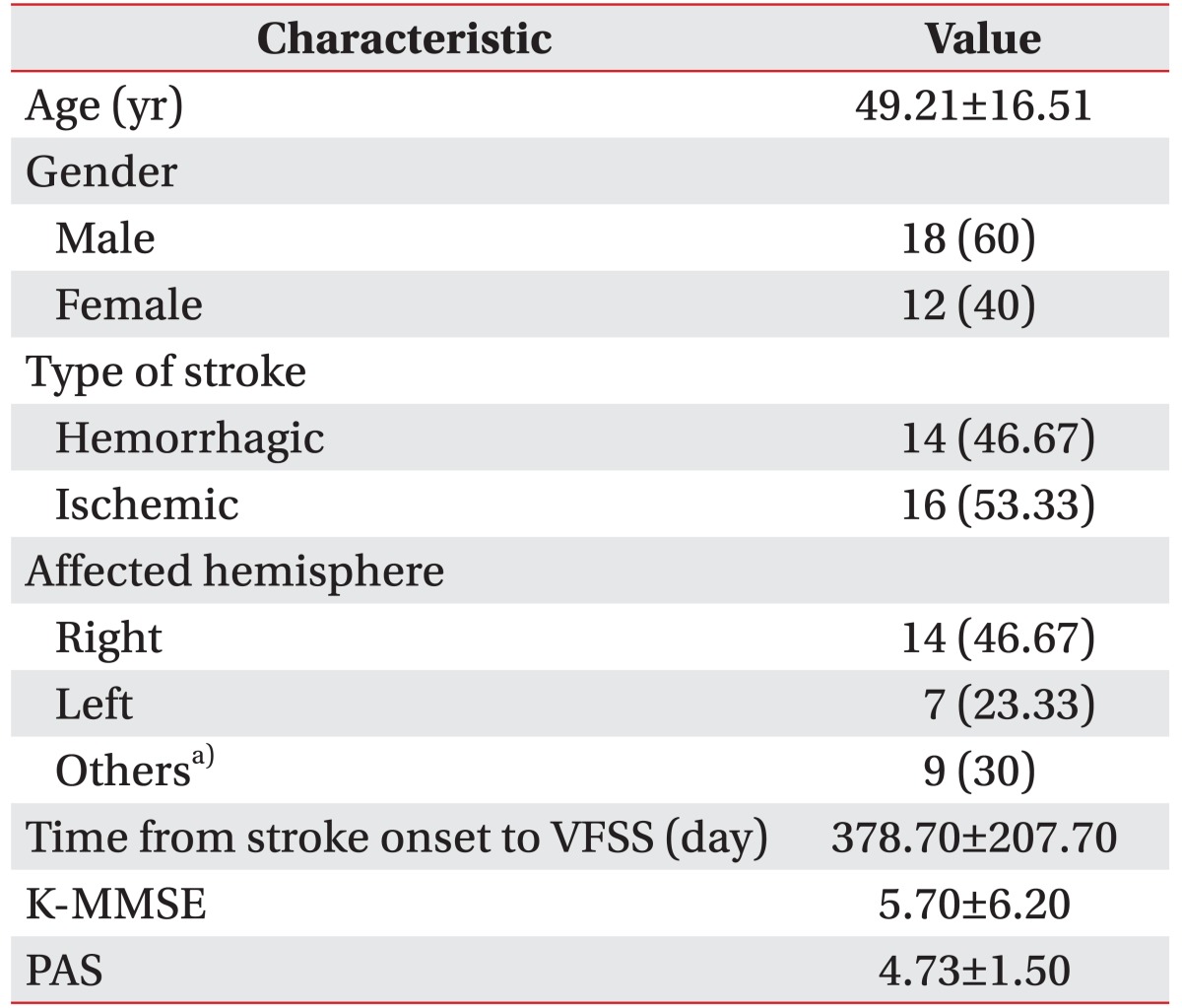
The subjects included 18 males (60%) and 12 females (40%) with mean age of 49.21±16.51 years. The type of stroke was hemorrhage for 14 patients (46.67%) and infarction for 16 patients (53.33%). With regards to the involved side, the right hemisphere was affected in 14 patients (46.67%), left in 7 patients (23.33%), and others for 9 patients (30%). Other areas include the brain stem, cerebellum, and multiple areas. The time from stroke onset to VFSS was 378.70±207.70 days and the mean K-MMSE (Korean version of Mini-Mental Status Examination) score was 5.70±6.20 points. The PAS score was 4.73±1.50 points (Table 1).
Observation of improvement pattern of dysphagia after vallecular ballooning revealed laryngeal elevation (x-axis: pre 2.62±1.51 mm and post 3.54±1.93 mm, p=0.038; y-axis: pre 17.11±4.24 mm and post 22.11±3.46 mm, p=0.036), pharyngeal transit time (pre 5.76±6.61 seconds and post 4.08±5.49 seconds, p=0.043), rotation of the epiglottis (pre 53.24°±26.77° and post 32.45°±24.60°, p<0.001), and post-swallow pharyngeal remnant (pre 41.31%±23.77% and post 32.45%±24.60%, p=0.002) had statistically significant differences before and after the procedure. No statistical significance was observed for semisolid aspiration (PAS score: pre 4.73±1.50 and post 4.46±1.78, p=0.391) (Table 2).
DISCUSSION
Foods are delivered safely and effectively to the stomach through the complex process of swallowing, which involves the elaborate adjustment of movements from the mouth to the esophagus within a short period of time, and requires well-coordinated and sequential contraction and relaxation of the mouth and pharyngeal muscles [9].
Logemann [10] divided the normal swallowing process into 4 steps: the oral preparation, followed by the oral, pharyngeal, and esophageal steps. In the pharyngeal step, the epiglottis backward stretching is achieved through the rise of the hyoid bone. Movement occurs when the epiglottis covers the larynx, and consequently, the airway is complexly closed.
Garon et al. [3] investigated the abnormal epiglottic movement pattern in patients with dysphagia, and reported that epiglottic dysmotility can be caused by several factors such as COPD, Parkinson disease, amyotrophic lateral sclerosis (ALS), and dementia, and including stroke as one of the factors. The abnormal epiglottic movement pattern is not a functional movement, incomplete inversion to a horizontal position, delayed tilt, oblique movement, mix pattern, etc.
Epiglottis is a cartilage not attached to the muscles, but attached to the hyoid bone, and is reported to be immobile by itself, moving passively through the hyoid bone movement, namely laryngeal elevation [11]. In addition, Perlman et al. [5] reported that epiglottis dysfunction, reduced hyoid elevation, and deteriorated oromotor function affects the vallecular residue. Also, the hyoid elevation was associated with epiglottis dysfunction.
Compensation techniques for laryngeal elevation include the Shaker exercise and Mendelsohn maneuver, effortful swallowing, and multiple swallowing. Efforts to solve abnormal epiglottis movement have been made with the help of above procedures [12].
Shaker exercise narrows the space between the tongue base and the posterior wall of the pharynx. It increases the pharyngeal pressure so that the bolus can easily pass to the pharynx [13]. Additionally, in patients with weakened laryngeal elevator muscles and late swallowing reflex, it reduces the risk of immediate aspiration of the bolus to the airway before swallowing, by inducing laryngeal elevation and epiglottis backward stretching [14]. The Mendelsohn maneuver maintains swallowing for 2–3 seconds, slowly relaxing when the pharynx is elevated at maximum. It helps the remnants in the piriformis space to move to the esophagus, by helping in clearing the remnant in the vallecular space through laryngeal elevation and opening of the cricopharyngeal muscle [12].
A recent study showed that the aspiration rate was lowered through the hyoid elevation, and reduced the pharyngeal residue by inducing an increase in the oromotor function and swallowing pressure through lingual exercise [15]. In addition, Heo and Kim [6] investigated the changes in the hyoid bone elevation and epiglottis angular variation before and after the attachment of Kinesio Tape to the chin and neck, and reported an improvement in the vertical movement of the hyoid bone and rotation angle of the epiglottis, before and after the taping procedure. These methods, however, only induced epiglottis movement and were not direct epiglottis exercise methods.
Our institution had previously reported a case of improvement in the swallowing parameters, including reduction of the vallecular remnant and decrease in pharyngeal transit time, after epiglottis backward stretching through the ballooning procedure with a Foley catheter in the vallecular space in patients with lowered kinetic movement after intubation [7]. The subject of the previous study was not a patient of neurogenic dysphagia, and did not have disorders in the swallowing parameters, except for deteriorated epiglottis mobility.
This study was the first to examine the improvement of dysphagia by performing a direct procedure, using ballooning in the vallecular space in stroke patients with neurogenic dysphagia. Two kinds of training were performed for vallecular ballooning: backward stretching of the epiglottis, and swallowing of a balloon located in the vallecular space. Contrast medium was injected into the balloon after putting the tip into the vallecular space, by checking the movement of the tip of the Foley catheter in real time using VFSS.
Two outcomes were expected after the above procedures. One was improved motility by stretching of the epiglottis, and the other was strengthening of the geniohyoid, mylohyoid, and thyrohyoid muscles, which experienced laryngeal elevation caused by the swallowing of the balloon located in the vallecular space.
An increase in epiglottis angular movement was expected to be induced due to the stretching, with a subsequent increase in the bolus transit into the pyriformis space and improvement of the protection of the vocal cord of the epiglottis. With strengthening of the geniohyoid, mylohyoid, and thyrohyoid muscles, the effort for swallowing the balloon located in the vallecular space improves the laryngeal elevation and increases the swallowing pressure through the isometric contraction exercise of these muscles. Hence, an overall effect of reduced post swallowing remnant and decreased pharyngeal transit time were expected. In this study, the laryngeal elevation (anterior and vertical movement), angular rotation of the epiglottis, pharyngeal transit time, and post-swallow remnant decreased after performing the ballooning procedure in the vallecular space. Also, the PAS score showed improvement, but was not statistically significant, the reason for this being the various causes of aspiration. Aspiration is observed not only in patients with epiglottic dysmotility or post-swallow remnants, but also in patients with vocal cord palsy protecting the airway during swallowing [16] or in patients in whom the upper esophageal sphincter is not sufficiently relaxed or contracted during swallowing, such as in patients with cricopharyngeal dysfunction [17]. Therefore, if the subject group for vallecular ballooning is limited to patients complaining of dysphagia caused solely by epiglottis dysmotility, the aspiration is expected to improve. Further studies are required in this area.
The side effects expected after vallecular ballooning include vomiting, mucosal injury, and pain. During the procedure, no patient experienced vomiting. After the procedure, 26 of the 30 patients were evaluated. On laryngoscopy, no lesions were observed, including mucosal bleeding and erosion, and no patient complained of discomfort in swallowing after ballooning. Yoon's previous study that performed piriformis ballooning using a Foley catheter had also not reported observations of any adverse side effects [18]. Our hospital has conducted the piriformis and vallecular ballooning procedures using a Foley catheter since 4 years without reports of any side effects. However, this procedure may be affected by the practitioner and by the material of the Foley catheter, and long-term studies for safety are required.
The advantages of vallecular ballooning are as follows. First, there is no risk of aspiration. As training is conducted not with actual food but with a balloon, the risk of aspiration pneumonia is small. Second, the procedure can be conducted without any influence from the cognitive function. If the patients cannot follow instructions due to lowered cognitive function, the procedure can be performed by inducing the swallowing reflex through manual stimulation with the index and middle fingers after palpating the upper hyoid bone. Third, it can be conducted with minimal cost, using only a Foley catheter and VFSS.
The limitations of this study are as follows. Although improvement of the laryngeal elevation was observed, but it would have been beneficial if the changes in the direct values on the geniohyoid, mylohyoid, and thyrohyoid muscles had been examined using an electromyogram. The implementation of post-treatment VFSS right after balloon training is the easiest way to investigate the effect of balloon treatment. This study had the advantage of excluding the confounding factors, but it had limitations in investigating the changes that can be shown after long-term training. Since the evaluation is performed immediately after the intervention, there is a limitation that there is no study on the training effect. This study reflected the treatment performed in the first VFSS after admission, and investigated the short-term effects of balloon treatment. However, if the training is repeated for longer period of time, significant changes may be found in the other parameters. In future, a study to confirm the long-term effects needs to be designed.
In stroke patients with dysphagia, improvements in the laryngeal elevation (anterior and vertical movement), angular rotation of the epiglottis, pharyngeal transit time, and post-swallow remnant were observed after vallecular ballooning. In particular, vallecular ballooning for patients in whom epiglottic dysmotility and post-swallow residue are observed, can be considered as an alternative method to be applied without an aspiration risk in swallowing rehabilitation treatment.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.