The Effect of Cardiac Rehabilitation Exercise Training on Cardiopulmonary Function in Ischemic Cardiomyopathy With Reduced Left Ventricular Ejection Fraction
Article information
Abstract
Objective
To observe the effect and safety of cardiac rehabilitation (CR) exercise in ischemic cardiomyopathy and to compare the results between patients with preserved left ventricular ejection fraction (LVEF) and reduced LVEF.
Methods
Patients with ischemic cardiomyopathy with LVEF <50% were included as subjects. The patients were classified into the preserved LVEF (pLVEF; LVEF 41%–49%) group and the reduced LVEF (rLVEF; LVEF ≤40%) group. Patients underwent hourly aerobic exercise training sessions with an intensity of 60%–85% of heart rate reserve, three times a week for 6 weeks. Graded exercise test and transthoracic echocardiogram were performed in all study patients before and after completion of the CR exercise program.
Results
After completion of the CR exercise program, both groups (pLVEF, n=30; rLVEF, n=18) showed significant increases in LVEF and VO2max. In the pLVEF group, LVEF and VO2max increased from 45.1%±4.8% to 52.5%±9.6% (p<0.001) and from 24.1±6.3 to 28.1±8.8 mL/kg/min (p=0.002), respectively. In the rLVEF group, LVEF and VO2max increased from 29.7%±7.7% to 37.6%±10.3% (p<0.001) and from 17.6±4.7 to 21.2±5.1 mL/kg/min (p<0.001), respectively. Both groups completed their exercise program safely.
Conclusion
In both groups, patients with ischemic cardiomyopathy who completed a 6-week supervised CR exercise program demonstrated remarkable improvements in cardiopulmonary function. This result implies that neither of the two groups showed higher efficacy in comparison to each other, but we can conclude that CR exercise in the rLVEF group was as effective and safe as that in the pLVEF group.
INTRODUCTION
Cardiac rehabilitation (CR) is a cost effective intervention for treating coronary heart disease (CHD) that improves the functional capacity and reduces acute hospital admissions, and it can therefore make a valuable contribution to the healthcare management of an ageing population [1]. When the exercise-based CR was carried out, there was a significant decrease in fatal refraction including total mortality, cardiovascular mortality [23], and improvement in cardiopulmonary fitness and psychological profiles [4].
It is already known that the large size of myocardial infarction (MI) causes ischemic heart failure (HF) and leads to left ventricular (LV) remodeling, and finally results in advanced LV dysfunction [5]. Therefore, major MI with a large infarction size was one of the major contraindications to exercise in the past. However, due to improvement in CR nowadays, it has been found that exercise based CR has a positive effect on exercise capacity as well as on LV remodeling in patients with severely impaired LV ejection fraction (LVEF) [6]. Therefore, ischemic cardiomyopathy is one of the diseases that improve after CR exercise.
Maximal oxygen consumption (VO2max) is the best available objective measure of aerobic exercise capacity and it represents the maximum capacity of an individual's body to transport and use oxygen during incremental exercise [7]. Also in general, VO2max is lower in patients with CHD than in age-matched healthy subjects [8], and many of these patients exhibit impaired LV function in response to exercise. However, some of the previous studies have reported a poor correlation between VO2max and LV performance [91011]. Furthermore, pharmacologic interventions that improve LV function in patients with HF may not necessarily result in increased maximal exercise capacity [7]. Therefore, we believe that improvement in both VO2max and LVEF can be a more meaningful outcome regarding the effectiveness of CR exercise than improvement in only VO2max.
Several studies have concluded that exercise training in patients with HF and preserved EF (HFpEF) confers benefit in terms of enhancement in exercise capacity and health-related quality of life and it appears to be safe [1213]. Also, several studies on HF with reduced ejection fraction have recently been reported and they show a positive effect of exercise training [14]. However, there are insufficient studies that compare the effect of CR between the ischemic cardiomyopathy with reduced LVEF (rLVEF) and preserved LVEF (pLVEF) groups.
The objective of this study was to compare the VO2max and LVEF after completion of CR exercise in ischemic cardiomyopathy and to evaluate the differences between the rLVEF and pLVEF groups. Also, to evaluate the safety of CR, we observed the associated adverse effects or a critical event that required urgent medical care in both groups.
MATERIALS AND METHODS
Subjects
Patients with ischemic cardiomyopathy as a result of a recent acute myocardial infarction event (≤2 months) and with LVEF <50% were included as subjects. This study was performed retrospectively, and eligible subjects were selected from among the patients with ischemic HF who were referred for CR to our hospital between January 2009 and December 2013. The average time to CR enrollment since the coronary event was 39.2 days in the rLVEF group and 18.5 days in the pLVEF group. The exclusion criteria included the following: (1) non-ischemic cardiomyopathy, (2) inability to ambulate owing to physical problems (paresis induced by cerebral stroke, spinal cord injury, amputation, severe pain, dyspnea, etc.), (3) recurrent CHD, (4) underlying pulmonary disease (aspiration pneumonia, chronic obstructive pulmonary disease, pneumothorax, etc.), (5) impaired cognitive function (vascular dementia, Alzheimer's dementia, other psychological disease, etc.), and (6) inability to complete the 6-week or the 18-session exercise training program (i.e., geographic or economic factors).
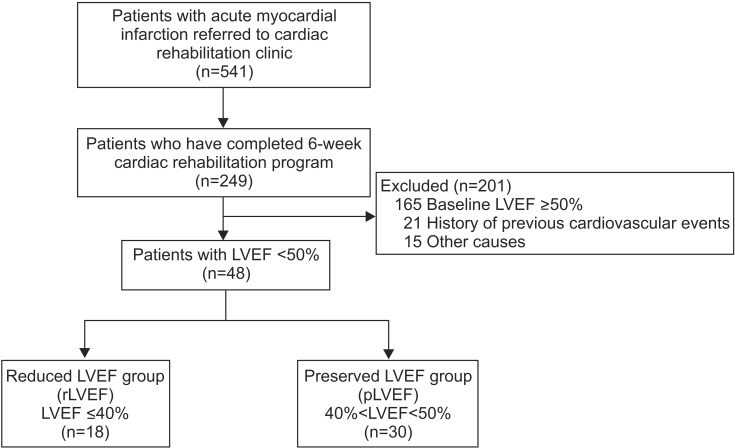
Since this study included acute ischemic heart failure patients, patients with LVEF ≥50% did not have common symptoms of heart failure that are found in chronic heart failure patients. This is the reason why we included patients with LVEF <50% in this study. Patients with LVEF ≤40% with advanced symptoms were classified into the rLVEF group, and patients with 41%<LVEF<50% with relatively mild symptoms were classified into the pLVEF group. It is important to note that the definition of preserved LVEF is different according the American Heart Association (AHA) HF guideline [15], in which LVEF 41%–49% is classified as borderline preserved ejection fraction and LVEF ≥50% is classified as preserved ejection fraction. Because we limited the inclusion criteria to LVEF <50%, we used the term 'preserved' for the group with 40%<LVEF<50% rather than borderline preserved ejection fraction. The pLVEF group comprised 30 patients (24 men and 6 women; mean age, 57.6±14.1 years); the rLVEF group comprised 18 patients (14 men and 4 women; mean age, 63.1±11.6 years) (Fig. 1). The study protocol was approved by the Institutional Review Board of Sanggye Paik Hospital (IRB No. 2014-12-001-001).
Methods
The CR exercise was performed under supervision at a single CR center using a standardized protocol. The patients were instructed to visit our CR clinic for preliminary examination, including the graded exercise test (GXT) during their first visit.
The GXT with ventilatory gas analysis was performed twice at baseline and at the 6-week follow-up by using the modified Bruce protocol according to the AHA guideline. The purpose of this exercise test was to measure VO2max and objectively monitor real-time electrocardiogram (ECG), heart rate (HR), blood pressure (BP), and Borg's 6-to-20 subjective rating of perceived exertion (RPE) during the test. For the GXT, a 12-channel real-time ECG tester for exercise load testing (Q4500; Quinton Instrument Co., Boston, MA, USA), a respiratory gas analyzer (True-One 2400; Parvo Medics Inc., Sandy, UT, USA), automatic blood pressure and pulse measuring instrument (Model 412; Quinton Instrument Co.), and treadmill for graded exercise testing (Medtrack ST55; Quinton Instrument Co.) were used.
Patients underwent hourly aerobic exercise training sessions, three times a week for 6 weeks. Each exercise session included a 10-minute warm-up, a 30-minute main exercise, and a 10-minute cool-down. Exercise intensity of a 30-minute main exercise was 60%–85% of heart rate reserve (HRR). HRR was calculated according to the Karvonen formula, with each patient's maximum HR and resting HR obtained by the GXT. All training sessions were supervised by the medical staff and monitored with ECG, HR, and BP using telemetry monitoring system (Q-Tel RMS; Cardiac Science, Bothell, WA, USA), and Borg's RPE scale during and after each training session. The patient was monitored and asked about any adverse event or unexpected discomfort. Transthoracic echocardiography examination was also performed in all patients twice before and after completion of the 6-week exercise. By performing TTE examination, LVEF, stroke volume (SV), left ventricular end-systolic diameter (LVESD), and left ventricular end-diastolic diameter (LVEDD) were measured. The examination was performed under quiet resting conditions, and the findings were analyzed by a single cardiologist.
All patients who participated in the CR program were educated on risk factor management, smoking cessation, and were provided obesity and nutrition consultations. Also, they received a drug prescription at the cardiology outpatient clinic.
Statistical analysis
The data was statistically analyzed with SPSS ver.18 (SPSS Inc., Chicago, IL, USA). In order to compare baseline characteristics of the two groups, student t-test was used. Paired t-test was used for comparing the parameters including LVEF, VO2max, SV, LVEDD, and LVESD before and after the CR program. ANCOVA analysis was used for comparison of outcomes between the two groups since it was necessary to eliminate within group error variance and adjust imbalances in prognostic variables. Statistical significance was defined as p-value of less than 0.05.
RESULTS
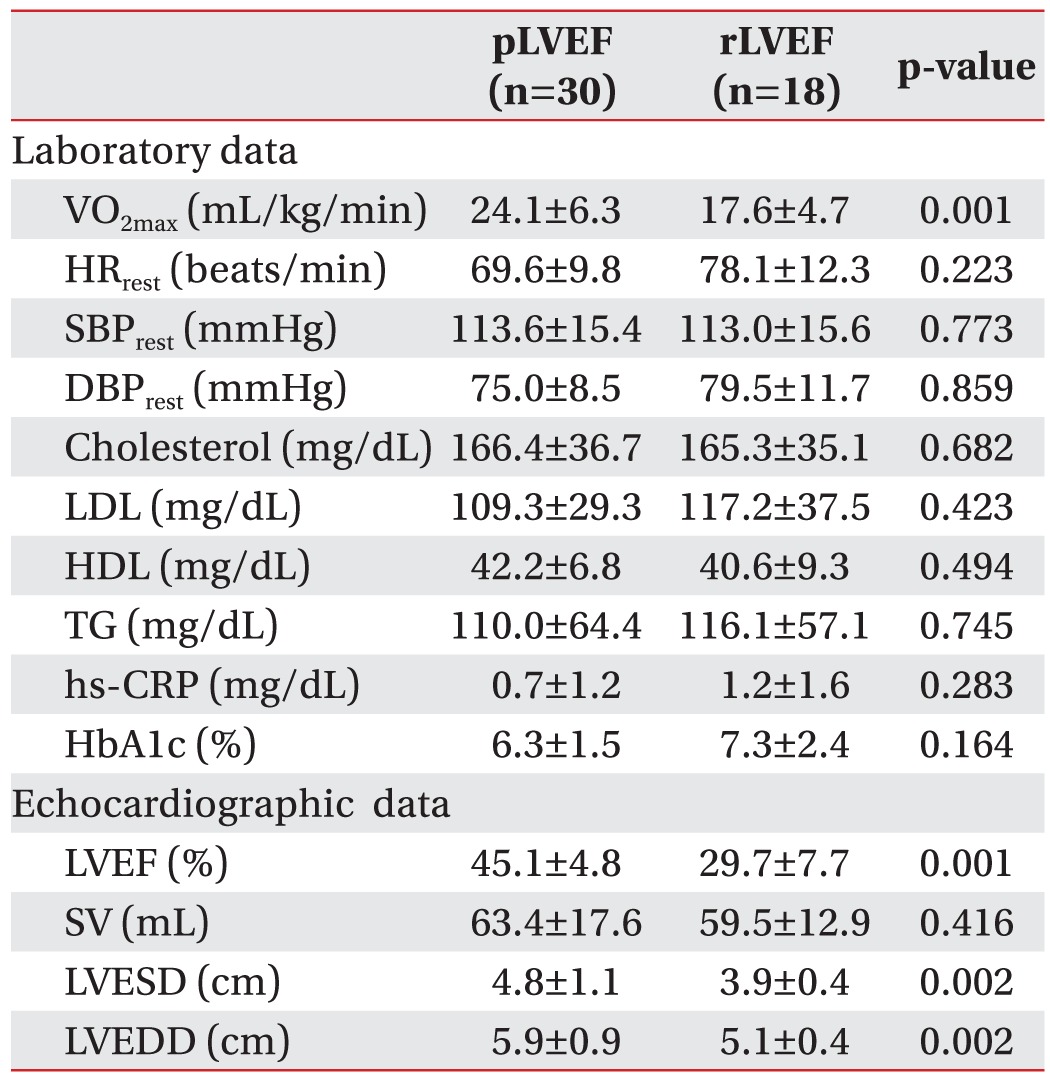
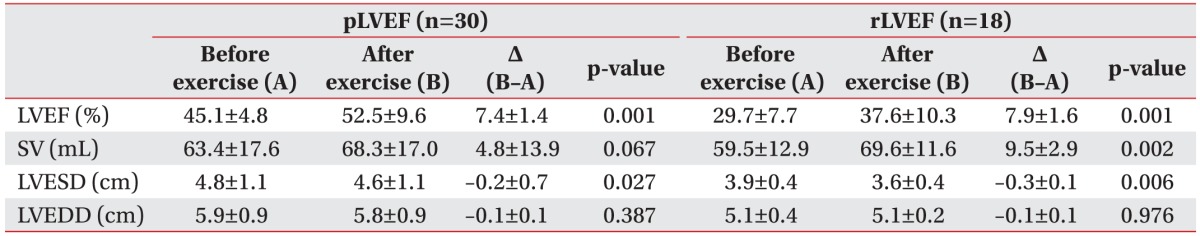
Comparison of demographic data between the two groups did not reveal significant differences (Table 1). Baseline laboratory data also showed no significant differences between the two groups except for VO2max. Among the parameters obtained from echocardiography, LVEF, LVEDD, and LVESD showed significant differences between the two groups, except for SV (Table 2). In the pLVEF group, LVEF increased from 45.1%±4.8% to 52.5%±9.6% (change rate, 16.2%±3.1%) and VO2max increased from 24.1±6.3 to 28.1±8.8 mL/kg/min (change rate, 17.8%±5.0%). In the rLVEF group, LVEF and VO2max increased from 29.7%±7.7% to 37.6%±10.3% (change rate, 30.2%±7.5%) and from 17.6±4.7 to 21.2±5.1 mL/kg/min (change rate, 23.2%±4.8%), respectively. All results were statistically significant in both groups (Tables 3, 4 and Figs. 2, 3).
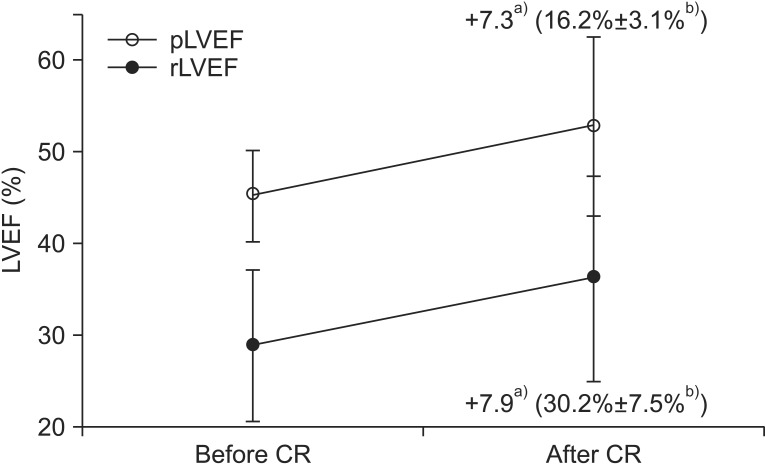
Changes in LVEF after cardiac rehabilitation (CR) exercise. pLVEF, preserved left ventricular ejection fraction; rLVEF, reduced left ventricular ejection fraction. a)Absolute change value, b)rate of change±standard deviation.

Changes in VO2max after cardiac rehabilitation (CR) exercise. pLVEF, preserved left ventricular ejection fraction; rLVEF, reduced left ventricular ejection fraction. a)Absolute change value, b)rate of change±standard deviation.
In both groups, the absolute change value of LVEF seemed to be similar (pLVEF, 7.4±1.4; rLVEF, 7.9±1.6), but since the two groups had different baseline LVEF, we also evaluated the relative change rate instead of the absolute change. Our aim was to observe the improvement rate rather than just comparing the change in values and this evaluation could also be applied for VO2max analysis. Relative changes in LVEF and VO2max, both parameters showed larger differences than those in absolute changes. In order to compare the significant differences between the two groups, we used ANCOVA analysis. The between-subjects effect analysis showed that both LVEF and VO2max showed significant improvement after CR exercise, but we could not conclude that the rLVEF group showed greater statistically significant improvement than the pLVEF group (between-subject effects in LVEF, p=0.61, VO2max, p=0.68). Also, throughout the total 720 hours of exercise (pLVEF, 450 exercise-hours; rLVEF, 270 exercise-hours), there were no adverse effects or a critical event that required urgent medical care or cessation of exercise in both groups.
DISCUSSION
The participation rate for the CR program has increased recently; however, the rate is still low despite evidence that participation in a CR program confers clinically significant benefits for patients diagnosed with cardiovascular disease [16]. One of the main reasons for low attendance is that especially the patients with low LVEF and poor cardiopulmonary function do not actively participate because of misconceptions such as CR is not safe and is relatively contraindicated; therefore, not beneficial [17]. However, findings of recent studies support the claim that patients with poor cardiopulmonary function and reduced LVEF are no longer a contraindication to CR nowadays and attending a CR program more actively has a positive effect on long-term mortality [1819]. The study by Beauchamp et al. [18] provided evidence for the long-term benefits of CR and suggested that a dose–response relationship may exist between the number of sessions attended and long-term mortality. The study comprised a total of 281 men and women eligible for CR following MI, coronary artery bypass surgery or percutaneous interventions. The mortality risk for non-attenders was 58% greater than for attenders. Participants who attended <25% of sessions had a mortality risk more than twice that of participants attending ≥75% of sessions. Therefore, attending a CR program more actively can lead to an anticipated reduction in further coronary events, and hence, it is necessary to encourage ischemic cardiomyopathy patients to participate in CR programs. Since many studies have proven that CR forms an important part of secondary coronary artery disease prevention [18192021], our study provides meaningful results which suggest that CR is safe even in patients with reduced LVEF as well as it is effective in improving their cardiopulmonary function. Our findings can positively influence the awareness and motivation of CHD patients for participation in CR.
Progressive LV enlargement, dilatation, and global or regional LV dysfunction can occur as a result of ischemic HF. These changes can act as important prognostic factors in the clinical course of chronic HF, particularly after a MI. These changes also known as 'remodeling' can precede deterioration in exercise capacity, and LV dilatation is associated with a significant reduction in cardiac performance [222324]. In several previous studies, the benefits of CR exercise training during the recovery period after ischemic heart disease have been well established [25]. Recently, these benefits have been extended to include patients with reduced LV function [262728]. Two previous studies reported abnormal remodeling in some patients; although training did not appear to have any effect on this process [2930]. Also, two recent studies related to the effects of exercise training on LV remodeling showed that exercise training has beneficial effects on LV remodeling and it even reverses LV remodeling in patients with heart failure [3132]. Also, it has been observed that CR has a direct influence on the myocardium, and it increases the myocardial perfusion which in turn increases the exercise capacity. This was confirmed by cardiac magnetic resonance imaging and quantitative positron emission tomography myocardial flow reserve (PET-MFR) assessments [33343536]. These previous studies have shown that CR has a significant benefit in recovery of LV function after LV remodeling.
Positive effects on LV function also support the importance of CR exercise, and therefore, the significance of active participation in CR by patients with reduced LVEF is emphasized and our significant results can support this concept. The effectiveness of CR has been extensively studied and the positive effect of CR is widely known these days. Dubach et al. [6] reported that a high-intensity, 2-month residential CR program resulted in substantial increases in exercise capacity among patients with reduced LV function. The study included 25 patients with reduced LV function and the patients resided in a rehabilitation center for 2 months and underwent a training program consisting of two 1-hour sessions of walking daily, along with four monitored 45-minute sessions of stationary cycling weekly. VO2max increased by 26% in the exercise group, whereas the control values did not change. On comparing with our study, our study included 48 patients and more specifically patients with very low LVEF (<30%) which could lead to a mean EF of 28.9%±8.1% in the rLVEF group while the mean EF in the study by Dubach et al. [6] was 31.5%±6.7%. Patients with ischemic cardiomyopathy who completed a 6-week supervised CR exercise program demonstrated safe sustained improvements in LVEF and VO2max, regardless of the initial baseline EF values. These findings can be supported by studies performed by Nishi et al. [37] and Vanhees et al. [38], which showed that CR in patients with reduced EF (<40%) had as much efficacy as that in cardiovascular disease patients with normal range EF as well as they proposed the safety of CR in both groups. The results of our study show that CR is effective in both groups, implying that neither the pLVEF group nor the rLVEF group showed higher efficacy in comparison to each other. Also, it should be emphasized that in our study, early CR was performed within an average 23.2 days after acute MI, even in patients with very low EF (<30%, n=7), and it was performed without any adverse events.
There are some limitations in this study. We aimed to recruit an equal number of patients in both groups; however, we were unable to include more patients in the rLVEF group within the selected period. A further study including a larger rLVEF group would be more representative and would convey a more significant result. Also, our study evaluated the difference over a 6-week period only; therefore, follow-up evaluation over a longer period should be considered in future studies.
We were able to obtain satisfactory results since the study was performed safely without any unexpected or lethal event in patients with very low LVEF, and this proved that early CR can be performed safely in patients with rLVEF and it has a positive effect on recovery of cardiopulmonary function.
In conclusion, the present study demonstrated two important findings. First, the effects of CR in patients with rLVEF were as significant as those in patients with pLVEF. Second, CR can be performed safely in the rLVEF group and it has a positive effect on recovery of cardiopulmonary function. Given the significant clinical benefits of CR, greater attention should be focused on increasing referrals, reducing barriers to attendance, and achieving reductions in CHD morbidity and mortality after CR completion. We believe that our findings can strongly support the use of CR, and hopefully, wide implementation of such programs may favorably impact patient participation.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.