Characteristics of Patients Injured in Road Traffic Accidents According to the New Injury Severity Score
Article information
Abstract
Objective
To investigate the clinical characteristics of patients involved in road traffic accidents according to the New Injury Severity Score (NISS).
Methods
In this study, medical records of 1,048 patients admitted at three hospitals located in different regions between January and December 2014 were retrospectively reviewed. Only patients who received inpatient treatments covered by automobile insurance during the period were included. Accidents were classified as pedestrian, driver, passenger, motorcycle, or bicycle; and the severity of injury was assessed by the NISS.
Results
The proportion of pedestrian traffic accident (TA) was the highest, followed by driver, passenger, motorcycle and bicycle TA. The mean NISS was significantly higher in pedestrian and motorcycle TAs and lower in passenger TA. Analysis of differences in mean hospital length of stay (HLS) according to NISS injury severity revealed 4.97±4.86 days in the minor injury group, 8.91±5.93 days in the moderate injury group, 15.46±11.16 days in the serious injury group, 24.73±17.03 days in the severe injury group, and 30.86±34.03 days in the critical injury group (p<0.05).
Conclusion
The study results indicated that higher NISS correlated to longer HLS, fewer home discharges, and increasing mortality. Specialized hospitals for TA patient rehabilitation are necessary to reduce disabilities in TA patients.
INTRODUCTION
Road traffic accident (RTA) is a serious public health problem and a major cause of disability worldwide. According to the World Health Organization, road traffic accidents claim 1.2 million deaths annually and cause up to 50 million non-fatal injuries [1]. In 2004, RTA ranked as the 9th leading cause of death worldwide and is expected to be the 5th by 2030 [2]. Moreover, the economic burden on society is increasing due to disabilities and deaths accompanying RTA, amounting to 518 billion US dollars per year, with the greatest losses especially in the working age population [3]. In 2014, there were a total of 20,117,955 registered automobiles in South Korea, and in 2012, there were 1,133,145 RTA, with 5,392 deaths and 1,777,604 injuries, thus showing the tendency of gradual increase in incidence of RTA. Compared to other Organization for Economic Co-operation and Development (OECD) member countries, of which 68.2% of the OECD average was 64.4 vehicles per 100 people, 43.9 per 100 people in South Korea owned automobiles as of 2010. However, there were 464.2 traffic accidents per 100,000 people, ranking 3rd, following the United States and Japan. In terms of number of traffic accidents, there were 105.8 traffic accidents per 10,000 vehicles, which placed South Korea in the 1st rank. Since the number of traffic accident patients is gradually increasing, identifying their clinical characteristics is important in planning rehabilitation program during acute inpatient treatment.
The Injury Severity Score (ISS), which was proposed in 1974 by Baker et al. [4], reflects deteriorating patients' conditions following trauma and is widely used as an indicator of the severity of anatomic injuries. However, since it only reflects a single injury from each body region, its clinical utility is limited. In order to address this problem, Osler et al. [5] proposed the New Injury Severity Score (NISS) in 1997; the current study used this tool to assess injury severity. This study was designed to assess the clinical characteristics of patients involved in traffic accident (TA) with NISS.
MATERIALS AND METHODS
Subjects
This study was approved by the Institutional Review Board of Uijeongbu St. Mary's Hospital. We retrospectively reviewed medical records of 1,048 patients admitted at three hospitals located in different regions between January and December 2014. Only patients who received inpatient treatments covered by automobile insurance during the period were included; whereas, those who were hospitalized or treated for sequela of accident were excluded. TA were defined as accidents involving personal injuries from vehicle traffic on the road.
Methods
Patients' gender, age, accident type, utilization of rehabilitative medicine or consultation, requirement for surgery, presence of multiple injuries, injury severity, hospital length of stay (HLS), Glasgow Coma Score (GCS) at admission, and type of discharge were investigated. Accidents were classified as pedestrian, driver, passenger, motorcycle, or bicycle, while discharge types included death, home discharge, university hospital, general hospital, rehabilitation hospital, convalescent hospital, and private hospital. In addition, intervening factors of rehabilitation therapy, such as presence of indwelling catheter, nasogastric tube, or endotracheal tube were further investigated.
The NISS was used to assess injury severity. To compute the NISS, each injury was classified according to body regions (head or neck, face, chest, abdominal or pelvic contents, extremities or pelvic girdle, and external) and severity, which was based on an abbreviated injury scale (1, minor; 2, moderate; 3, severe, not life-threatening; 4, severe, life-threatening, survival probable; 5, critical, survival uncertain; and 6, fatal injury). Next, regardless of body regions, the scores from the three regions in order of highest injury severity were squared and summed [6]. For example, a person with multiple injuries to the face, chest, and extremities with injury scale of graded 2, 1, and 3, respectively, had a NISS of 14. According to a study by Stevenson, et al. [7], injury severities in the present study were classified based on NISS score: minor (1–3 points), moderate (4–8 points), serious (9–15 points), severe (16–25 points), or critical (25–75 points).
Statistical analysis
ANOVA test was used to compare subgroups according to accident type, age, NISS, and transfer type, and Scheffe post-hoc test was also performed. Independent t-test was used to compare NISS according to the presence of the catheter or tube. The p-values less than 0.05 were considered statistically significant.
RESULTS
General characteristics of the subjects
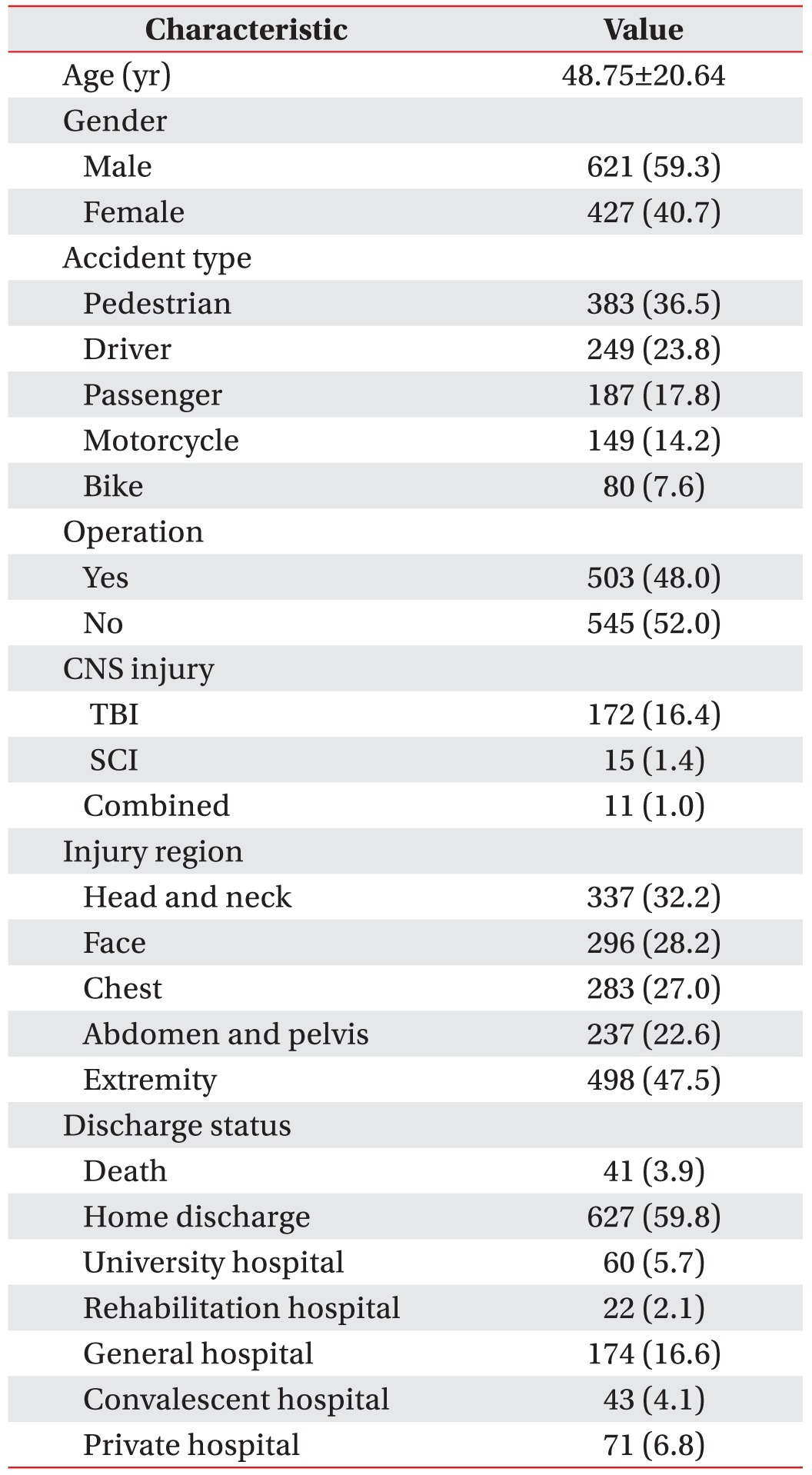
The age of subjects ranged from 1 to 94 years, with a mean age of 48.75±20.64 years; 128 (12.2%) were 20 years or below, 213 (20.3%) were 21–40 years, 381 (36.4%) were 41–60 years, and 326 (31.1%) were 61 years or older. The mean of NISS in 20 years or below was 13.25±13.79, 12.91±13.70 in 21–40 years, 15.08±13.61 in 41–60 years, and 19.03±15.55 in 61 years or older. Post-hoc Scheffe test showed that the mean of NISS was significantly higher in 61 years or older group (p<0.05). There were 621 men (59.3%) and 427 women (40.7%) in the study population.
Most patients (n=871, 83.1%) had a GCS of 15 at admission, while 26 patients (2.5%) had a GCS of 3. A total of 176 patients (16.8%) had central nervous system injuries, including 172 (16.4%) with traumatic brain injury; 15 (1.4%) had spinal cord injuries, and 11 (1.0%) had both. In addition, 141 patients (13.5%) required long-term bed rest due to femur or spine fractures. In terms of the proportion of patients with major injuries, such as central nervous system injuries and femur or spine fracture, according to accident type, bicycle TA comprised 42.5%, while motorcycle, driver, passenger, and pedestrian TAs made up the remaining accidents, at 38.9%, 20.9%, 26.7%, and 34.7%, respectively.
A total of 503 (48.0%) patients underwent surgeries due to TA injury, and 701 (66.9%) incurred multiple traumas. Extremities were most often injured, with 498 cases (47.5%) followed by head and neck (n=337, 32.2%), face (n=296, 28.2%), chest (n=283, 27.0%), and abdomen and pelvis (n=237, 22.6%); 298 patients (28.4%) had upper or lower extremity fractures (Table 1).
Accident types and NISS
Pedestrian TAs were most common, with 383 (36.5%) cases, followed by driver (n=249, 23.8%); passenger (n=187, 17.8%); motorcycle (n=149, 14.2%); and bicycle TAs (n=80, 7.6%). The mean of NISS in pedestrian TA was 18.93±15.33, 17.72±15.53 in motorcycle TA, 15.48±14.75 in bicycle TA, 12.99±13.63 in driver TA, and 10.97±10.26 in passenger TA. Post-hoc Scheffe test showed that the mean of NISS was higher in pedestrian and motorcycle TAs and significantly lower in passenger TAs, which were statistically significant (p<0.05) (Table 2).
HLS and NISS
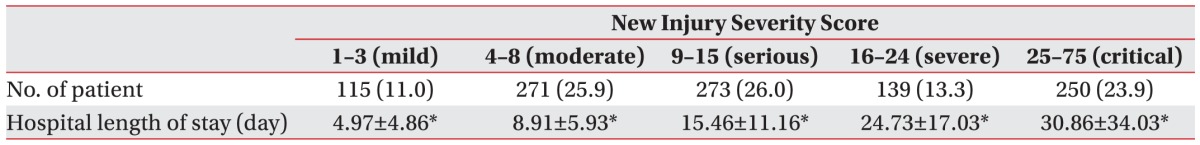
A total of 483 (46.1%) patients were hospitalized ≤10 days, 284 (27.1%) for 11–20 days, 122 (11.6%) for 21–30 days, 58 (5.5%) for 31–40 days, and 101 (9.6%) for ≥41 days. Analysis of injury severity by NISS revealed 115 cases (11.0%) of mild injury (≤3 points); 271 (25.9%) of moderate injury (4–8 points); 273 (26.0%) of serious injury (9–15 points); 139 (13.3%) of severe injury (16–24 points); and 250 (23.9%) cases of critical injury (25–75 points). Analysis of differences in mean HLS according to NISS injury severity revealed 4.97±4.86 days for patients in the minor injury group (NISS, 1–3), 8.91±5.93 days in the moderate injury group (NISS, 4–8), 15.46±11.16 days in the serious injury group (NISS, 9–15), 24.73±17.03 days in the severe injury group (NISS, 16–24), and 30.86±34.03 days in the critical injury group (NISS, 25–75), with statistically significant differences (p<0.05) (Table 3). Post-hoc Scheffe test showed that higher NISS was significantly correlated with longer HLS (p<0.05).
Condition at discharge and NISS
Among study subjects, 41 patients (3.9%) died and 7 (0.7%) were discharged in a comatose state. A total of 713 (68.0%) patients had independent gait without serious complication, while 287 patients (27.4%) were discharged with required assistance in gait and activity of daily living. The mean NISS was 10.21±9.46 in the independent gait group, 24.63±14.86 in the group requiring assistance in gait, 48.71±14.84 in the comatose state group, and 42.02±15.94 in the group of patients who had died, with significant group-wise differences (p<0.05).
Most patients were discharged to their homes (n=627, 59.8%), while 60 (5.7%) and 22 (2.1%) patients were discharged to university and rehabilitation hospitals, respectively; in addition, 174 (16.6%), 43 (4.1%), and 71 (6.8%) patients were discharged to general, convalescent, and private hospitals, respectively. The mean NISS was 9.78±8.67 in the home discharge group, 22.52±15.71 in the transfer group, and 42.02±15.94 in the group of patients who had died. Post-hoc Scheffe test showed that the mean of NISS was significantly higher in the group of patients who had died and significantly lower in the home discharge group (p<0.05).
Rehabilitation therapy
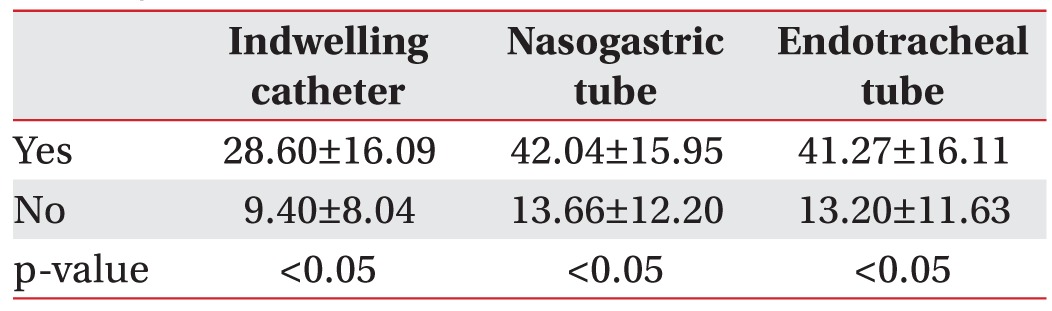
Among patients in this study, 137 (13.1%) underwent rehabilitation consultation, including 13 (1.2%) who were transferred to the department of rehabilitation medicine for intensive treatment. Indwelling catheters were inserted in 342 patients (32.6%); while 74 patients (7.1%) received a nasogastric tube and 92 (8.8%) underwent intubation. NISS according to the presence of the catheter or tube in each group showed a statistically significant difference (p<0.05) (Table 4).
DISCUSSION
The ISS has been considered as the gold standard of assessing injury severity; however, it possesses weakness in the evaluation of multiple skeletal injuries [8]. In a person with multiple fractures, the ISS would be calculated based on the most severely injured site, and the total severity may be overlooked by ignoring other significant fractures [9]. In order to address this problem, Osler et al. [5] proposed the NISS in 1997. The NISS considers the three most severe injuries, regardless of body region. According to Lavoie et al. [68], NISS is not only a more correct predictor of in-hospital mortality than the ISS, but also helpful in forecasting intensive care unit admission and HLS. Moreover, according to Sutherland et al. [9], NISS is helpful in predicting functional outcomes such as mobility, house work or self- care in patients of musculoskeletal trauma. The results of the present study indicated that higher NISS was correlated to longer HLS, fewer home discharges, and increasing mortality. Among accident types, NISS was high in pedestrian and motorcycle TA, which consequently showed higher rates of poor prognosis.
Injuries from TAs result in tremendous personal and social losses. They can diminish quality of life and can lead to functional and occupational activity impairments, as well as psychological problems in road traffic injured patients [1011]. In South Korea, there were a total of 1,133,145 cases, 5,392 deaths, and 1,777,604 people injured from TAs in 2012. As compared to statistics data of the previous year, the number of both, total TA and subsequent death, were increased (26.3% and 3.1% increase, respectively). Hence, the need for systematic rehabilitation therapy to reduce complications is also anticipated to increase.
Receiving appropriate rehabilitation therapy after injury is important for improving functional outcomes. Brooke et al. [12] examined patients with fractures from TAs and reported positive effects on pain and return to work in the patient group that underwent early intervention through rehabilitation consultation. Despite the fact that many TA patients require rehabilitation to achieve improved prognosis, only 13.1% of patients in the present study received evaluation and management by the department of rehabilitative medicine during their hospitalization. There were several possible reasons for this fact. First, injuries that were restricted to face, rib or minor injuries such as laceration were difficult to be considered as indication for rehabilitation. Moreover, some patients that were in life-threatening conditions, such as internal organ damage or septic condition, could not endure the rehabilitation program due to poor general condition. Finally, discharge from the hospital was mandated in some patients due to limited duration of hospital stay. A number of other factors besides rehabilitation therapy can also influence the prognosis of TA patients. Fort et al. [13] reported that severe lower-limb lesions, severe thoracic lesions, and cranial trauma significantly delayed patients' return to work.
Improving functional outcome and preventing disability in TA patients are important from a cost-savings perspective, not only for the patients, but also for the society as a whole. Prolonged time of returning to workplace and loss of work capacity due to TA-related complications reduce quality of life of the patients and family, and can lead to inefficient distribution of limited medical resources. Currently, it is difficult to provide sufficient functional assessment and early rehabilitation therapy to patients with trauma; considering the present medical insurance system, treatment is even more difficult for patients with fractures or internal organ damage since they often require long-term HLS. To reduce patients' disabilities and improve prognosis, management of socioeconomic and psychological factors during the subacute stage is needed; however, as mentioned earlier, adequate care is difficult due to limit in HLS and other issues. Therefore, sufficient hospitals that can provide specialized treatment to TA patients are required, in order to improve the quality of life for patients and their families and reduce the social loss of patients.
The present study has several limitations. Functional and psychological evaluations, which are expected to influence patients' prognosis, were not sufficiently conducted; furthermore, since no follow-up observations were made due to the retrospective nature of the study design, data on complications, such as pain, that can occur after discharge were unavailable. In addition, future investigations on the association between return to work and quality of life would be meaningful.
In the present study, the medical records of automobile insurance patients who were admitted to three hospitals located in different regions in 2014 were investigated to identify clinical trends in TA patients. The prognostic factors for patients included accident type and initial injury severity, while higher NISS showed a pattern of prolonged treatment duration and increased mortality. Although comprehensive rehabilitation therapy is needed to reduce disabilities in TA patients, it is currently difficult to adequately undertake such tasks, and specialized hospitals for TA patient rehabilitation are necessary. The results of the present study may inform development of adequate rehabilitation therapy for TA patients and can be used as fundamental data for more broad-based studies in the future.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.