- Search
| Ann Rehabil Med > Volume 40(6); 2016 > Article |
Abstract
The fabella is a small sesamoid bone generally located in the tendon of the lateral head of the gastrocnemius behind the lateral condyle of the femur. Fabella syndrome is the occurrence of posterolateral knee pain associated with the fabella. It is a rare cause of knee pain that is often misdiagnosed. Fabella syndrome can be managed with conservative or surgical treatment. We applied radial extracorporeal shock wave therapy as a new treatment strategy for fabella syndrome and achieved a successful outcome.
The fabella (little bean) is a small sesamoid bone typically found in the tendon of the lateral head of the gastrocnemius (GCL) behind the lateral condyle of the femur. This bone has an anatomic variation in 10% to 87% cases [1,2,3]. Fabella syndrome, a rare cause of knee pain, is characterized by repeated pain in the posterolateral aspect of the knee. Fabella syndrome can be diagnosed on the basis of clinical symptoms, physical examination, or radiographic or ultrasonographic (USG) findings but tends to be overlooked. As the fabella is a normal anatomic structure, it is not usually considered as the cause of pain. Although the fabella could be a source of atypical knee pain, it is often misdiagnosed as other common causes of knee pain such as intra-articular loose body, meniscal tear, and osteoarthritis or lumbosacral radiculopathy. Such misdiagnosis may delay treatment or result in unnecessary arthroscopic procedures [4].
Treatment of fabella syndrome includes various non-surgical conservative treatment or surgical excision but the outcome is not favorable [3,4].
In this study, radial extracorporeal shock wave therapy (rESWT) was applied as a new treatment strategy for fabella syndrome with good results. To the best of our knowledge, this is the first report of rESWT for treatment of fabella syndrome.
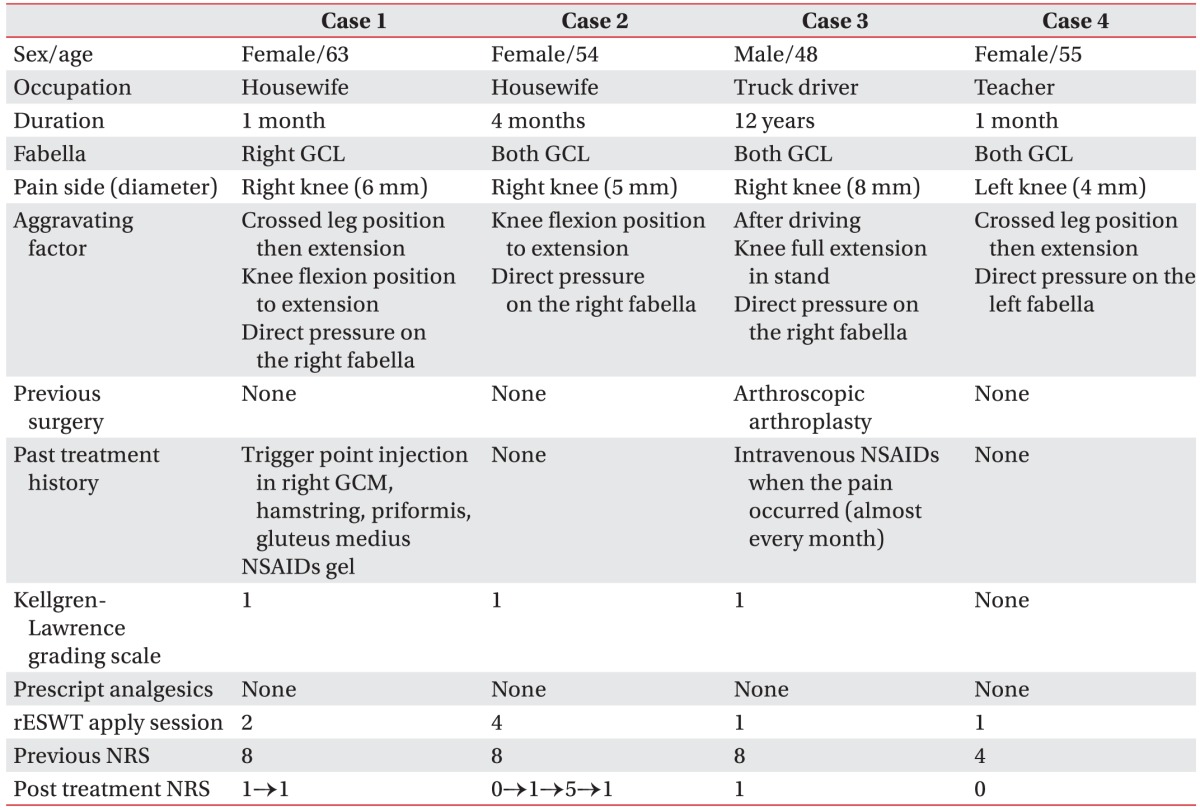
Three middle-aged women (cases 1, 2, and 4) and 1 man (case 3) visited our hospital as outpatients because of intermittent unilateral (right: cases 1, 2, and 3; left: case 4) posterolateral knee pain. Cases 1 and 2 were housewives, case 3 was a truck driver, and case 4 was a teacher. In cases 1, 2, and 4, recent increased activity had caused posterior knee pain; whereas, case 3 had posterior knee pain for 12 years. On physical examination of the patients' knees, there was no swelling in anterolateral or posterior knee area and knee joint motion was smooth with no detectable crepitus in the patellofemoral or tibiofemoral articulations. Manual muscle tests for knee and ankle muscle groups showed normal results in all cases. Range of motion of the symptomatic knee was nearly equal to that of the contralateral knee in cases 1, 2 and 4; while full extension of the knee joint was impossible because of pain in case 3. Examination of the ligaments around the knee joint indicated absence of ligament laxity with normal findings on anterior and posterior drawer, valgus-varus stress, Lachman's, pivot shift, and Apley's tests. In all cases, typical symptoms of fabella syndrome were observed such as pain on direct pressure to the fabella, crossed leg to extension position of knee, knee flexion to extension position, and gait (Table 1).
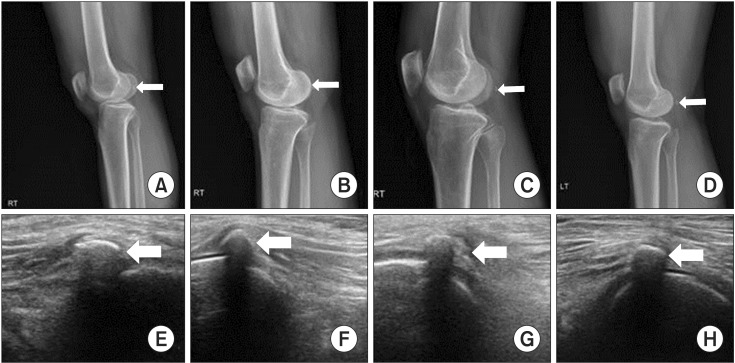
Osteoarthritis was diagnosed on radiography (Kellgren-Lawrence grading scale 1) in cases 1, 2, and 3. Cases 2, 3, and 4 had fabellas in both knees; while case 1 had a fabella only in the right knee that showed pain symptoms (Table 1, Fig. 1).
On USG, there was no joint effusion, synovial thickening, intra-articular loose body, fluid collection in the bursa, ganglion cyst, patellar tendon and ligament tears or tendonitis, and occult fractures (Fig. 1). The fabellas were noted in all cases of painful knees and direct tenderness above fabellas was provoked by compression with USG probe. There was no swelling or tear in the origin of GCL of the lateral condyle of the femur as well as the GCL fibers around the fabellas.
We applied rESWT using MASTER PLUS MP2000 (Storz Medical, Tagerwilen, Switzerland) at the fabella under USG guidance. All patients were prepared in the prone position with extended knee. Three thousand shock waves with 12 Hz were delivered at the intensity of 3 to 5 bar. Total 1 to 4 interventions according to cases were applied at an interval of 2 weeks. An aqueous gel was applied between the probe and skin to reduce the loss of shock wave energy at the interface.
After treatment, pain score was decreased from 8 to 1 in cases 1, 2, and 3 and from 4 to 0 in case 4 on the numerical rating scales (NRS). In addition, in case 3, full extension of the knee joint was achieved. These effects were maintained for 2 months. Booster stimulations were applied in cases 1 and 2 (Table 1). No side effect such as bruising or edema was observed on the treatment area.
The fabella is a sesamoid bone generally located around the posterolateral knee area in the GCL. The fabella can exist in a non-ossified fibrocartilaginous state and is occasionally found in the medial head of the gastrocnemius [2]. Recently, two anatomical studies suggest that the fabella complex is composed of fabella and its surrounding structures including not only the GCL but also plantaris muscle, oblique popliteal ligament, arcuate ligament, fabellofibular, and fabellopopliteal ligaments. The interactions among the fabella complex could result in the development of ossified fabella. The fabella could have a functional role by redirecting the flexion force of knee joint, similar to the patella redirecting extension forces of the knee joint [1,2].
In the general population in Western countries, the fabella is present in approximately 10%–30% subjects and, in most cases, located in the GCL and bilateral knees [3]. However, wide variations were reported in the incidence of fabellas in 61 Chinese cadavers, of which 53 cases (86.89%) had fabellas in the lateral head and 6 (9.84%) in the medial head [2]. Another cadaveric study on 39 Japanese indicated 66.0% cases with fabellas, including bony fabellas (29.3%). Of these bony fabellas, 43 (97.7%) were located in the GCL with its surrounding structures [1].
In our study, cases 2, 3, and 4, had fabellas located on the GCL on both knees; whereas case 1 had a fabella only on the right knee. X-ray and USG indicated ossified fabellas in all cases (Fig. 1).
Posterolateral knee pain due to the presence of a fabella, also referred to as fabella syndrome, may occur [5,6]. Fabella syndrome is associated with position- or activity-related posterolateral knee pain during end-range of knee flexion, knee extension, and various sporting attempts [7]. Posterolateral knee pain on pressing the fabella, is an obvious indicator of the fabella as the underlying cause [8].
While the exact pathophysiology of fabella syndrome is unclear, some hypotheses have been proposed. First, the enthesopathy of fabella complex could be a cause of fabella syndrome. Overall, the fabella itself does not generate pain, however, the ossified fabella can cause increase in tensile force and repetitive mechanical stress of the fabella complex [1,8]. This leads to inflammatory response and pain of fabella complex [2,4,7]. Second, the proximity of the fabella to the lateral condyle of the femur is another potential cause of fabella syndrome through synovial irritation and degeneration of the articular surface [2,6]. The former emphasizes the pathology on fabella complex; whereas the latter on knee joint or the lateral condyle of the femur.
In our cases, the size of the fabellas was <8 mm, which was too small to irritate the synovium or articular surface of the lateral condyle of the femur. However, the patients experienced direct tenderness over the fabella and pain was provoked on stretching the knee joint, as seen in enthesopathy. Acute overloading (increased tensile force) or overuse (repetitive mechanical stress) seemed to trigger the fabella syndrome. In cases 1, 2, and 4, recently increased walking exercise caused posterior knee pain; and case 3 (a truck driver) drove in the knee flexion posture and exerted repetitive pressure on the right ankle by pushing the accelerator and brake pedals. Therefore, in our cases, enthesopathy of fabella complex was considered as the main cause of fabella syndrome.
USG allows dynamic assessment of the exact tender point over the fabella, which can be compared easily with the contralateral side. In addition, other pathologic findings that potentially cause knee pain can be ruled out, such as joint effusion, synovial thickening, intra-articular loose body, fluid collection in the bursa, ganglion cyst, patellar tendonitis, and occult fractures. Fabella-related pain can be misdiagnosed on USG as an abnormal soft tissue calcification or loose body, hence, caution is required in identifying the fabella [9].
Fabella syndrome can be treated with non-surgical conservative methods or surgical treatment [8]. Non-surgical treatment includes steroid injection, immobilization with splinting and casting, temporary restriction of activity, physical modality, manual therapy and analgesic agents. Fabellectomy is a representative surgical treatment [3,4]. Literature reports on surgical treatment include small sample size and uncertain postoperative success rates. Surgical excision should be considered with priority for cases with fabella-induced peroneal nerve injury or articular surface irritation of the lateral condyle of the femur [8].
ESWT is gaining attention as a new treatment strategy for various musculoskeletal problems, because of its effectiveness, noninvasiveness, and applicability. The therapeutic mechanism of ESWT includes destruction of sensory unmyelinated nerve fibers, neovascularization in degenerative tissues, and hyperstimulation analgesic effect. ESWT can be classified into two types including focused ESWT and rESWT. Compared with focused ESWT, rESWT has larger treatment areas with superficial action thus providing potential advantages in treatment of superficial structure pathology such as enthesopathy [10].
We applied rESWT under the assumption that fabella syndrome in our cases was an enthesopathy of fabella complex. The 15 mm-diameter of the transmitter head of rESWT was larger than the size of fabella and sufficient for stimulating the entire fabella complex including fabella and its surrounding structures. Application of rESWT resulted in immediate and dramatic resolution of symptoms that was maintained in the 2-month follow-up.
In conclusion, fabella syndrome should be considered in the differential diagnosis of posterior knee pain. If the cause of the fabella syndrome is thought to be the enthesopathy of fabella complex, it could be managed with rESWT successfully. Larger studies are required to confirm this result, establish a treatment protocol for rESWT, and compare focused ESWT with rESWT.
CONFLICT OF INTEREST:
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
1. Kawashima T, Takeishi H, Yoshitomi S, Ito M, Sasaki H. Anatomical study of the fabella, fabellar complex and its clinical implications. Surg Radiol Anat 2007;29:611-616. PMID: 17882346.


2. Zeng SX, Dong XL, Dang RS, Wu GS, Wang JF, Wang D, et al. Anatomic study of fabella and its surrounding structures in a Chinese population. Surg Radiol Anat 2012;34:65-71. PMID: 21626275.


4. Franceschi F, Longo UG, Ruzzini L, Leonardi F, Rojas M, Gualdi G, et al. Dislocation of an enlarged fabella as uncommon cause of knee pain: a case report. Knee 2007;14:330-332. PMID: 17490883.


5. Zenteno Chavez B, Morales Chaparro IF, De la Torre IG. Fabella syndrome in a high performance runner: case presentation and literature review. Acta Ortop Mex 2010;24:264-266. PMID: 21305764.

6. Weiner DS, Macnab I. The “fabella syndrome”: an update. J Pediatr Orthop 1982;2:405-408. PMID: 6815224.


7. Zipple JT, Hammer RL, Loubert PV. Treatment of fabella syndrome with manual therapy: a case report. J Orthop Sports Phys Ther 2003;33:33-39. PMID: 12570284.


8. Driessen A, Balke M, Offerhaus C, White WJ, Shafizadeh S, Becher C, et al. The fabella syndrome: a rare cause of posterolateral knee pain: a review of the literature and two case reports. BMC Musculoskelet Disord 2014;15:100PMID: 24666711.




9. Friedman L, Finlay K, Jurriaans E. Ultrasound of the knee. Skeletal Radiol 2001;30:361-377. PMID: 11499776.


10. Chang KV, Chen SY, Chen WS, Tu YK, Chien KL. Comparative effectiveness of focused shock wave therapy of different intensity levels and radial shock wave therapy for treating plantar fasciitis: a systematic review and network meta-analysis. Arch Phys Med Rehabil 2012;93:1259-1268. PMID: 22421623.