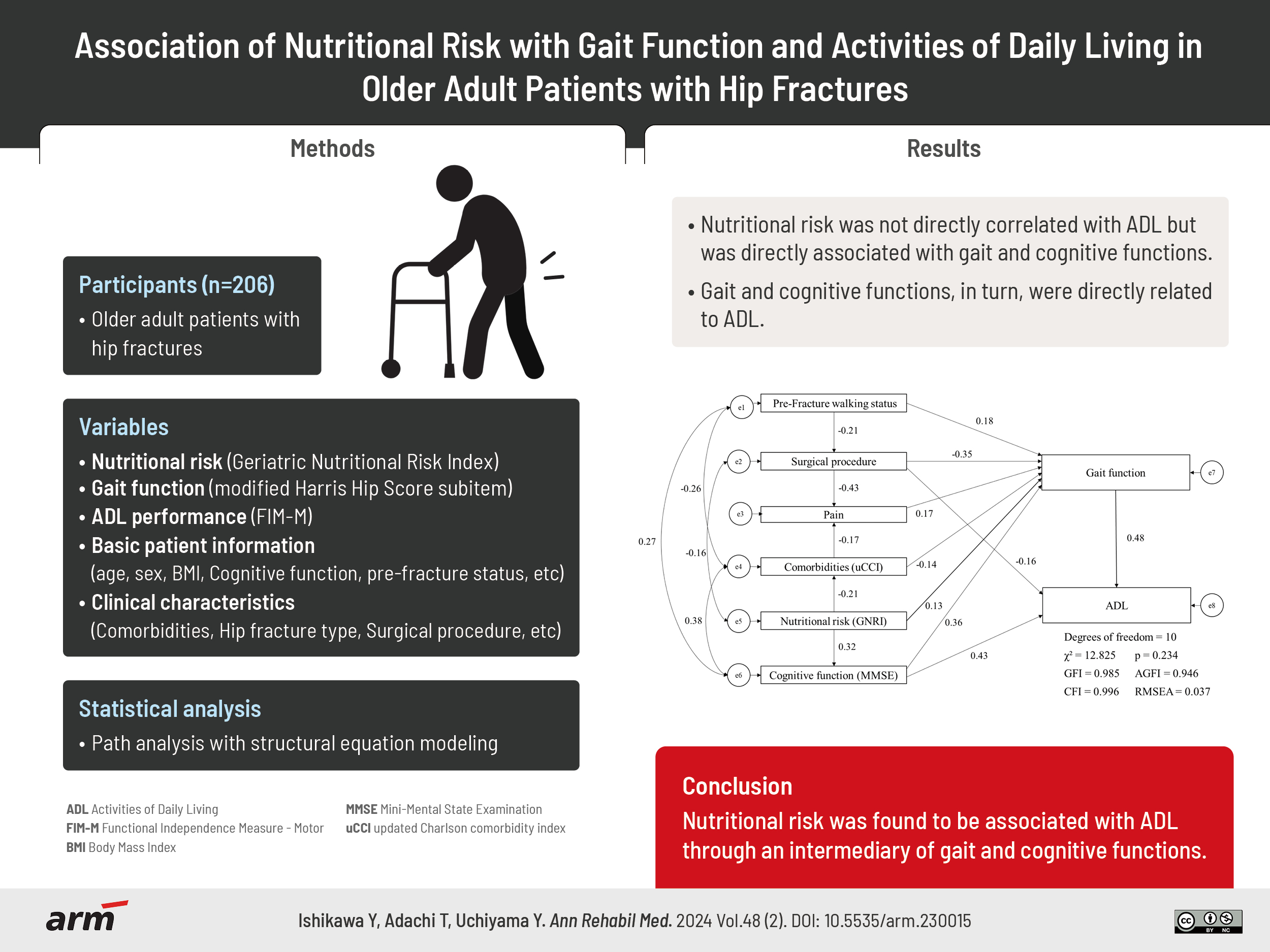
Association of Nutritional Risk With Gait Function and Activities of Daily Living in Older Adult Patients With Hip Fractures
Article information
Abstract
Objective
To investigate the association of nutritional risk with gait function and activities of daily living (ADLs) in older adult patients with hip fractures.
Methods
The retrospective data of older adult patients diagnosed with hip fractures who visited the recovery-phase rehabilitation ward between January 2019 and December 2022 were reviewed. Nutritional risk was evaluated using the Geriatric Nutritional Risk Index; gait function and ADLs were assessed using the modified Harris Hip Score subitem and Functional Independence Measure, respectively. Multivariate linear regression and path analysis with structural equation modeling were used to examine the factors associated with ADLs and the associations among the study variables.
Results
This study included 206 participants (172 females and 34 males; mean age, 85.0±7.3 years). In the multivariate analysis, gait function (β=0.488, p<0.001), cognitive function (β=0.430, p<0.001), and surgery (β=-0.143, p<0.001) were identified as independent factors. Pathway analysis revealed that nutritional risk was not directly correlated with ADLs but was directly associated with gait and cognitive functions. Gait and cognitive functions, in turn, were directly related to ADLs.
Conclusion
Nutritional risk was found to be associated with ADLs through an intermediary of gait and cognitive functions.
INTRODUCTION
Hip fractures are the most prevalent fracture among older adult patients, and their incidence is expected to increase [1,2]. Approximately 20%–40% of hospitalized older adult patients with hip fractures exhibit nutritional risk [3]. The effects of nutritional risk on clinical outcomes after hip fractures include increased mortality [4], complications during hospitalization such as infectious disease and delirium [5,6], and delayed functional recovery [7,8].
Recently, a growing body of literature has focused on the effect of nutritional risk on activities of daily living (ADLs) [9-12]. However, owing to the complex nature of ADLs comprising various factors [13], the influence of nutritional risk on ADLs remains controversial. Previous studies that demonstrated the association of nutritional risk with ADLs commonly used the Mini Nutritional Assessment (MNA) as a tool for nutritional screening [14]. Owing to the inclusion of functional assessments such as gait and cognitive function as subitems in the MNA, there exists a potential for an overestimation in the association between MNA and ADLs. Notably, while ADLs in patients with hip fractures exhibited an association with MNA, other established nutritional screening tools such as the Malnutrition Universal Screening Tool, Nutritional Risk Screening 2002, and the Geriatric Nutritional Risk Index (GNRI) did not demonstrate any such relationship [15]. Furthermore, when assessing the nutritional risk of older adult patients, there is a concern that MNA overestimates nutritional risk with high sensitivity and low specificity [16,17]. Consequently, older adult patients who are at nutritional risk based on the MNA may exhibit gait and cognitive function issues. Therefore, when attempting to elucidate the distinction between nutritional risk, gait function, and ADLs, the MNA is deemed unsuitable.
One of the nutritional indices for hospitalized older adult individuals is the GNRI, which is determined based on the serum albumin level and the ratio of current to ideal body weight. Its distinctive feature is its applicability to patients with cognitive impairment, and it can be easily measured using routine tests [18], making it a user-friendly tool for hip fracture patients. Previous studies evaluating the nutritional risk of patients with hip fractures using the GNRI have revealed its predictive value for postoperative survival rates [19]. However, the association of GNRI with gait function and ADLs has not been examined. Nutritional risk assessment using the GNRI may allow for elucidation of the influence of only nutritional risk on ADLs in older adult patients with hip fractures.
Determination of whether nutritional risk directly or indirectly affects ADLs through gait function can contribute to furthering the understanding of nutritional risk, gait function, and ADLs in hospitalized older adult patients with hip fractures, potentially supporting the development of effective physical therapy.
METHODS
Study design and participants
This retrospective observational study included patients discharged from the recovery phase rehabilitation ward of Nishio Hospital between January 2019 and December 2022. Inclusion criteria involved patients with hip fractures aged ≥65 years. Exclusion criteria included patients who died, those discharged because of deterioration in their condition by the onset of acute illnesses, or those who had missing data. In Japan, patients who cannot be discharged from acute care hospitals after acute hip fractures are admitted to a recovery phase rehabilitation ward for functional recovery. This policy was introduced in 2000 under Japan’s National Health Insurance system to provide ongoing rehabilitation in a hospital setting.
The study was conducted in accordance with the Declaration of Helsinki and the Strengthening the Reporting of Observational Studies in Epidemiology statements. This study was approved by the Bioethics Committee of Nagoya University (approval number: 23-512) and the Ethics Committee of Nishio Hospital (2023-001). Owing to the retrospective nature of this study, the requirement for informed consent was waived. Instead, participants were provided with the option to opt-out: information regarding the study was posted on the hospital notice board and the university’s webpage, allowing patients to withdraw their participation at any time.
Variables
Nutritional risk
This study used the GNRI as a nutritional risk indicator [18]. The formula for calculating GNRI is as follows:
GNRI=(1.489×serum albumin value)+[41.7×current weight (kg)/ideal weight (kg])
Calculation of ideal weight (Lorenz formula):
For male: Height (cm)-100-[(Height (cm)-150)/4]
For female: Height (cm)-100-[(Height (cm)-150)/2.5]
The GNRI calculations used the serum albumin level, height, and weight assessed upon admission to the rehabilitation ward.
Gait function
Gait function was assessed using the modified Harris Hip Score (mHHS) [20], a disease-specific instrument that assesses hip disabilities and is often used by healthcare workers to evaluate functional outcomes or interventions [21]. The mHHS comprises eight questions divided into subsections on pain, gait function, and ADLs. The pain subsection measures pain severity, its effect on activity, and the need for analgesics (one item, 0–44 points). The gait function subsection assesses limp, support needed, and distance walked (three items, 0–33 points), whereas the ADLs subsection evaluates managing shoes and socks, stairs, using public transportation, and sitting (four items, 0–14 points), with a total score of 91. A higher score indicated less pain and better gait function and ADLs. The mHHS has been used to functionally evaluate patients for the total score and the score of each subsection [22,23]. The assessment was performed at discharge during the recovery phase in the rehabilitation ward. We did not use the mHHS ADLs subsections because ADLs performance was evaluated using the Functional Independence Measure (FIM) described below.
ADLs performance
ADLs performance was assessed using the FIM motor (FIM-M) items, a method with good clinical utility for assessing ADLs in patients with hip fractures [24]. The FIM-M items included 13 domains (eating, grooming, bathing, dressing the upper body, dressing the lower body, toileting, bladder management, bowel management, transfer to bed/chair/wheelchair, transfer to toilet, transfer to tub/shower, locomotion by walking or wheelchair, climbing stairs) and were scored from 1 (complete assistance) to 7 (complete independence), resulting in a total FIM-M score ranging from 13 to 91. The FIM-M was assessed upon discharge from the rehabilitation ward.
Basic patient information and clinical characteristics
Basic patient information included age, sex, body mass index (BMI), Mini-Mental State Examination (MMSE) score, prefracture walking status, and the number of days elapsed from injury to discharge at the rehabilitation hospital. Prefracture walking status was classified into independent walking, walking with a cane, walking with a walker, or using a wheelchair, in reference to the cumulative ambulation score [24]. The number of days elapsed was measured from the time of injury to admission to the rehabilitation ward and from admission to discharge from the rehabilitation wards.
Patient clinical characteristics included the updated Charlson comorbidity index (uCCI) score [25], hip fracture type (femoral neck or trochanteric), fracture side (right or left), surgical procedure (open reduction with internal fixation, hemiarthroplasty, or conservative), blood biochemistry data (serum albumin, total protein, and C-reactive protein), and polypharmacy. Polypharmacy was defined as six or more medications. Basic patient information and clinical characteristics, excluding the number of days elapsed, were assessed at the time of admission to the rehabilitation ward.
Statistical analysis
Patients were classified into four groups using GNRI criteria, ranging from no nutritional risk (>98), low (92–98), moderate (82–92), to major (<82) [18]. Patient characteristics were compared among groups using one-way ANOVA and the chi-square test for continuous variables and categorical variables, respectively.
The relationships between FIM-M and basic information, clinical characteristics, and nutritional indicators were evaluated. Continuous data were analyzed using Pearson’s correlation coefficient and Spearman’s correlation coefficient for categorical data. Additionally, surgical procedures (open reduction with internal fixation and hemiarthroplasty vs. conservative) and prefracture gait status (independent gait vs. walking with a cane, walker, and wheelchair) were categorized into two groups. The GNRI was included as a continuous variable. After correlation analysis, multiple regression analysis (stepwise method) was performed to investigate the factors influencing FIM-M. The independent variables were selected from previously studied factors [13] and variables with significant correlations.
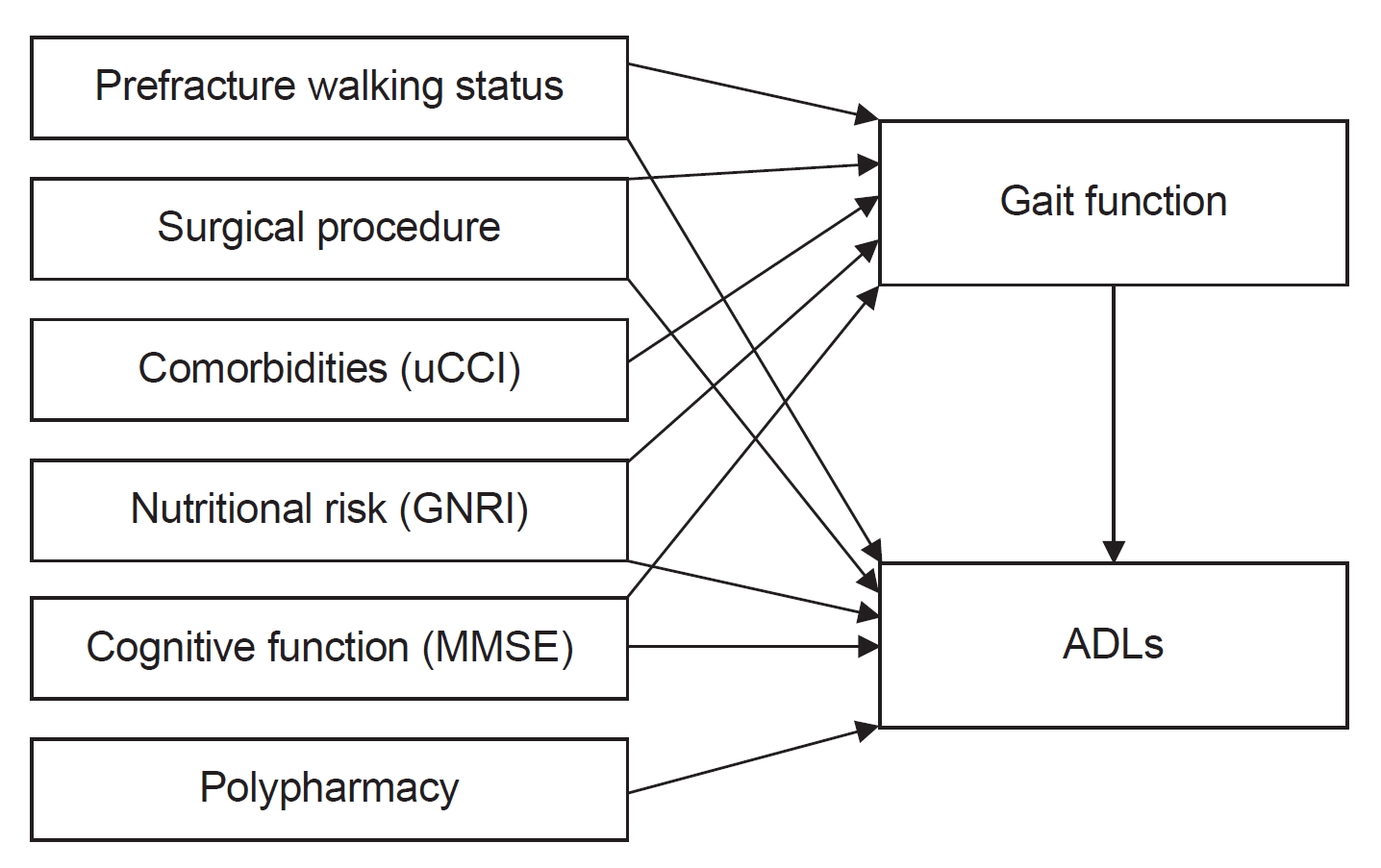
Path analysis was used to elucidate the association between GNRI, FIM-M, gait function, and associated factors. This analysis enabled efficient and direct modeling and testing of indirect or mediated relationships among variables. Fig. 1 shows a hypothetical model based on a previous study. Nutritional risk has been identified as a predictive factor for gait function [8] and ADLs [10,11] through cohort studies. Similarly, factors such as gait function have also been demonstrated as predictive factors for ADLs within the context of cohort studies [13]. The hypothesized model was refined based on the results of the correlation and multiple regression analyses, and path analysis was conducted to assess the model fit. All statistical analyses were performed using IBM SPSS software and Amos (version 26.0; IBM Corp.), with the significance level set at 5%.
RESULTS
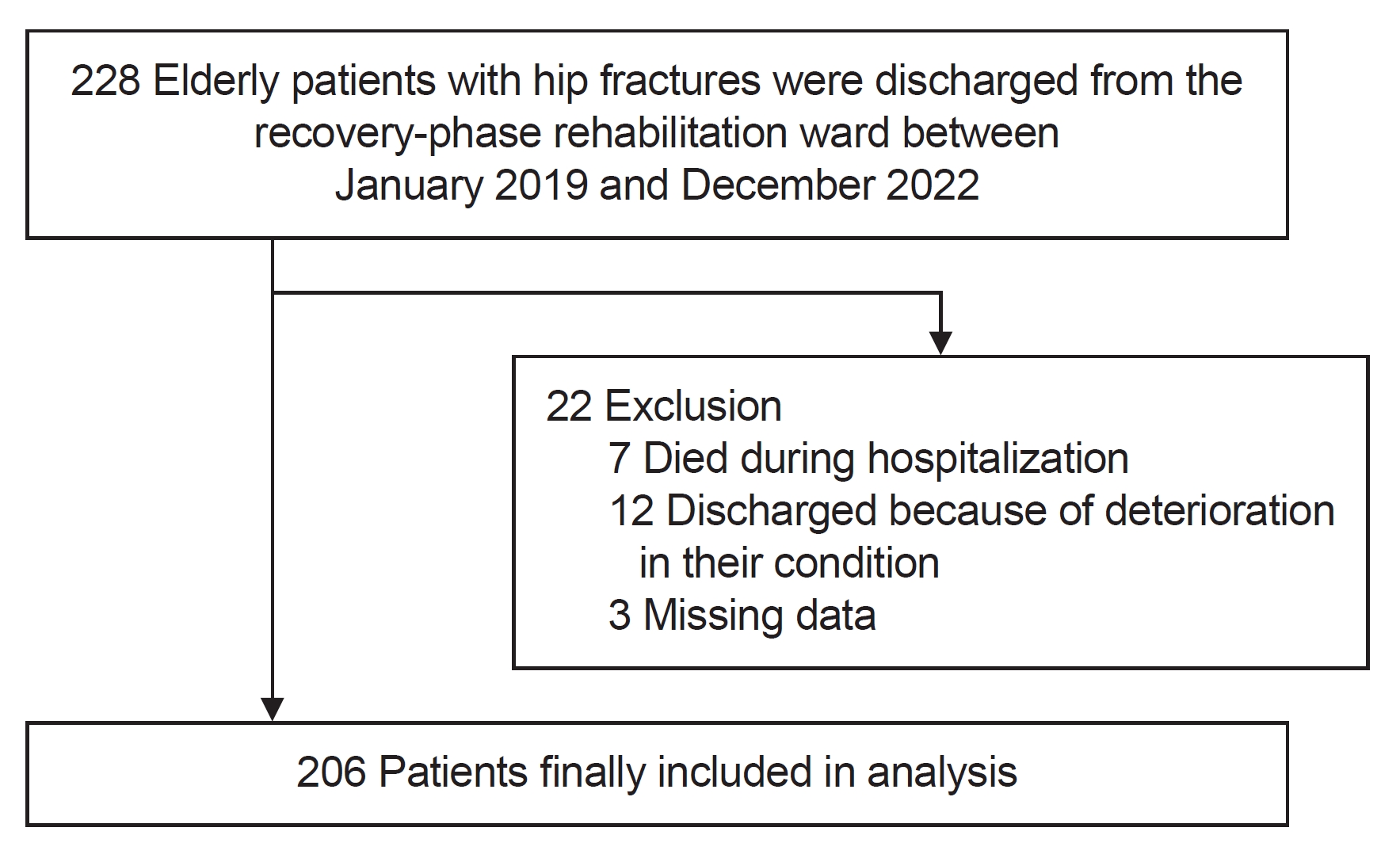
In total, 228 older adult patients with hip fractures were discharged from the recovery-phase rehabilitation ward. Among these, 7 died during hospitalization, 12 were discharged because of deterioration in their condition, and 3 had missing data. The final analysis included 206 patients (Fig. 2).
Basic information and clinical characteristics of the total patient cohort and of the four nutritional risk groups are shown in Table 1. Of the 206 patients, 172 (83.5%) were females and 34 (16.5%) were males. The mean age was 85.0±7.3 years and the MMSE score was 17.1±8.7 points. Among the patients, 98 (47.6%) had femoral neck fractures and 108 (52.4%) had trochanteric femoral fractures. The mean mHHS pain score was 36.5±9.0 points, and the mean gait function score was 10.1±9.9 points. The mean FIM-M score was 52.3±24.6 points. The GNRI assessment indicated that 51 patients (24.8%) had no nutritional risk, 31 (15.0%) had low risk, 74 (35.9%) had moderate risk, and 50 (24.3%) had major risk. The mean GNRI was 89.5±10.5. Patients with no nutritional risk were significantly younger and had higher MMSE, gait function (mHHS), and FIM-M scores (p<0.001).
Table 2 shows the results of the correlation analysis between ADLs (FIM-M), basic information, clinical characteristics, and the GNRI. ADLs (FIM-M) was significantly correlated with age, BMI, MMSE, prefracture walking status, uCCI, surgical procedure, albumin level, C-reactive protein level, mHHS (pain and gait function), and GNRI score. Table 3 shows the results of the multiple regression analysis of ADLs (FIM-M). Multiple regression analysis was performed using age and number of days elapsed as adjustment factors and significant items in the correlation analysis as independent variables (MMSE, prefracture walking status, uCCI, surgical procedure, C-reactive protein, pain, gait function, and GNRI). The independent factors for ADLs (FIM-M) were gait function, MMSE score, and surgical procedure. The model explained 78.1% of the variance (adjusted R2) in ADLs (FIM-M).
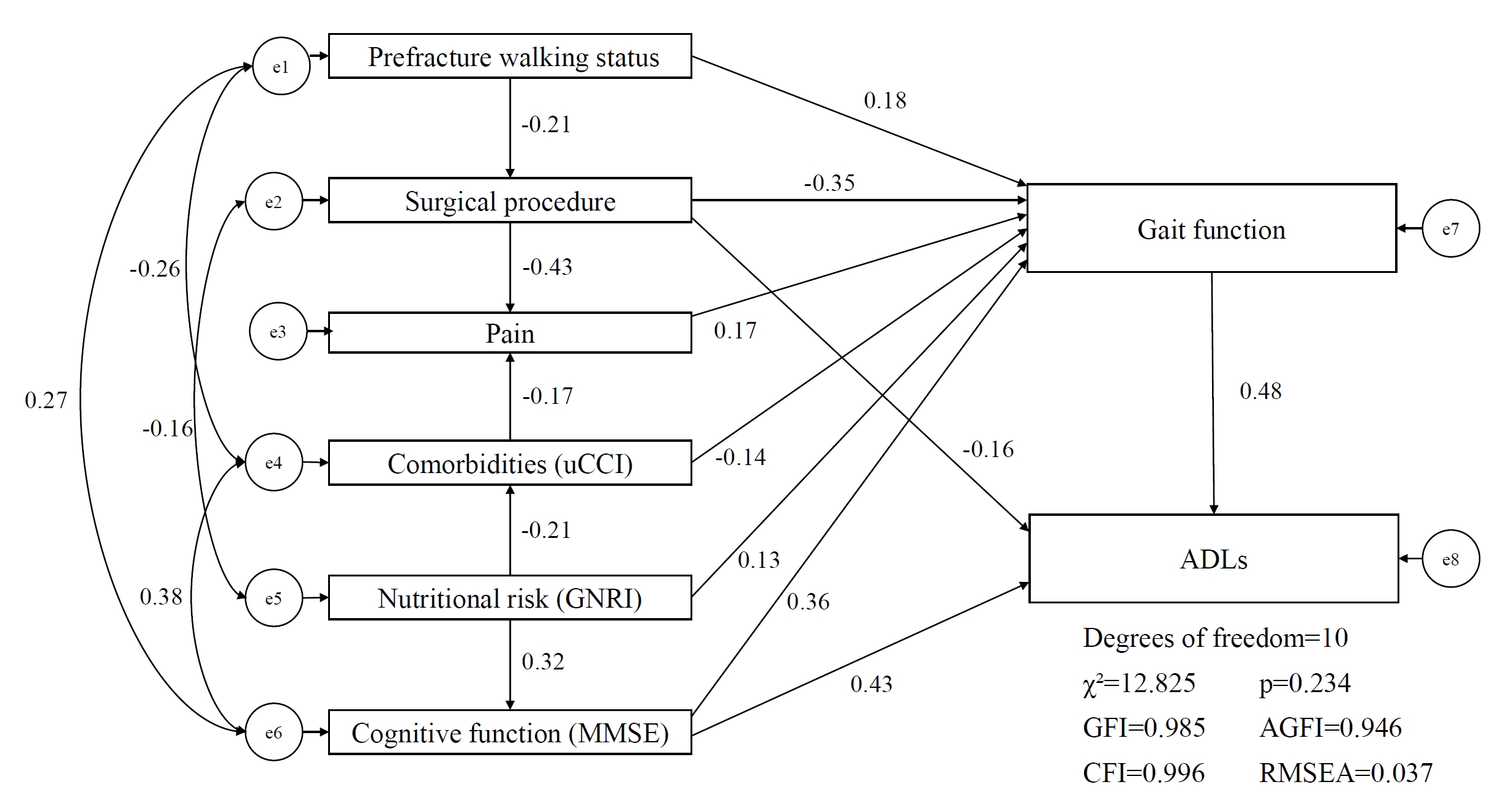
Fig. 3 depicts the path analysis results. Based on the results of the multiple regression analysis, only significant paths were retained, and other significant factors were added. The final path model was an excellent fit for data (χ2=12.825, p=0.234, GFI=0.985, AGFI=0.946, CFI=0.996, RMSEA=0.037). The following significant correlations were identified: Nutritional risk (standardized estimate=0.13) and cognitive function (standardized estimate=0.36) were associated with gait. Gait function (standardized estimate=0.48) and cognitive function (standardized estimate=0.43) were related to ADLs, whereas nutritional risk was not. Furthermore, nutritional risk was associated with cognitive function (standardized estimate=0.32) and comorbidities (standardized estimate=-0.21).
DISCUSSION
The results of this study indicate that nutritional risk was associated with ADLs through gait function in older adult patients with hip fractures. Using path analysis, we traced the complex pathways through which nutritional risk is correlated with gait function and ADLs. The final path analysis model revealed that nutritional risk was directly related to gait function but was not directly associated with ADLs, whereas gait function was directly related to ADLs.
This study revealed that nutritional risk was not directly associated with ADLs, which is inconsistent with the findings of previous research. Most studies that have concluded an independent association between nutritional risk and ADLs have used the MNA to assess nutritional status [9-12]. The utilization of the MNA, including gait function, in nutritional risk assessment might be the causal factor directly related to ADLs. Gait function was the factor most highly correlated with ADLs in the standardized regression coefficients of the path analysis in this study. Furthermore, cognitive function emerged as a variable directly correlated to ADLs following gait function. Therefore, nutritional risk may be associated with ADLs via the intermediary of gait and cognitive functions. The MNA is a comprehensive nutritional risk indicator that has excellent relevance to other assessments, including prognosis prediction of ADLs. In contrast, the GNRI used in this study allowed for the structural separation of nutritional risk, gait function, cognitive function, and ADLs. This feature enabled a clear delineation of each issue.
The association of nutritional risk with ADLs through the intermediary factors of gait and cognitive function among patients with hip fractures can be described with reference to the recovery process specific to this patient group. This recovery process comprises a sequence initiated by pathology leading to impairment, followed by hip fracture repair and healing, in which nutritional risk plays a role in recovery from impairment. Subsequently, recovery from functional limitations, encompassing gait and cognitive function, is achieved, culminating in recovery from disability, including ADLs [26]. Considering the temporal sequencing of the recovery process and the relationship between nutritional status, gait and cognitive functions, and ADLs in patients with hip fractures [13], the path analysis in this study reveals the delineation of such a relationship from nutritional risk through gait and cognitive function, leading to ADLs. Additionally, we clarified the association between nutritional risk on ADLs and gait function in a path analysis that incorporated prefracture walking status, surgical procedures, and comorbidities, which were factors affecting ADLs in previous studies. Our findings will be useful for rehabilitation programs that consider the nutritional risks of older adult patients with hip fractures.
Based on the findings of this and previous studies, the rationale behind the association with nutritional risk on ADLs through gait function is as follows. The relationship between nutritional risk and gait should be considered in frailty and sarcopenia cases. There is a consensus that malnutrition in older adults is associated with frailty and sarcopenia [27], and the malnourished status of patients with hip fractures causes frailty [28] and sarcopenia [29]. The diagnostic criteria for frailty and sarcopenia include a decline in gait function [30,31], making it evident that a close relationship exists between these conditions and gait function. Frailty and sarcopenia affect gait function in patients with hip fractures [32,33]. Therefore, frailty and sarcopenia arising from malnutrition may affect gait function. However, regarding the relationship between nutritional risk and cognitive function, the intricate mechanisms underlying the effect of malnutrition on cognitive function have not been fully elucidated. Nevertheless, clinical evidence has shown many instances linking malnutrition to cognitive function [34,35]. Furthermore, malnutrition in patients with hip fractures results in a more pronounced decline in ADLs when combined with cognitive impairment [12]. Although we were unable to collect indicators related to the skeletal muscle in this study, it is reasonable to assume that the skeletal muscle is a mediating factor between nutritional risk and gait function based on previous research. Future studies should address this issue to elucidate the interrelationships among the nutritional risk, skeletal muscle, and ambulatory function.
This study had some limitations. Path analysis could not establish causal relationships because of the study’s retrospective nature. A prospective research design was essential to explore the temporal relationships between the variables included in this study. Additionally, as the study was conducted at a single institution, there is a potential for selection bias. Notably, the serum albumin included in the GNRI is affected not only by nutritional risk but also by inflammatory states [36].
Despite these limitations, to our knowledge, this study is the first to investigate the relationship among nutritional risk, gait function, and ADLs in older adult patients with hip fractures. The results of this study support the importance of the relationship between nutritional status and gait function in multidisciplinary rehabilitation to improve ADLs in older patients with hip fractures [37].
In conclusion, nutritional risk was associated with ADLs through an intermediary of gait and cognitive functions. This study suggests that older adult patients with hip fractures who exhibit favorable nutritional status and good gait function may experience improved ADLs outcomes.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING INFORMATION
None.
AUTHOR CONTRIBUTION
Conceptualization: Ishikawa Y, Adachi T, Uchiyama Y. Methodology: Ishikawa Y, Adachi T, Uchiyama Y. Formal analysis: Ishikawa Y. Project administration: Uchiyama Y. Writing – original draft: Ishikawa Y. Writing – review and editing: Adachi T, Uchiyama Y. Approval of the final manuscript: all authors.