Fact Sheet on Cardiac Rehabilitation for Cardiovascular Disease in South Korea
Article information
Abstract
Cardiovascular disease (CVD) poses a significant health challenge globally, including in Korea, due to its status as a leading cause of death and its impact on cardiopulmonary function. Cardiac rehabilitation (CR) is a well-established program that not only aids in restoring cardiopulmonary function, but also improves physical and social conditions. The benefits of CR are widely recognized, and it is implemented globally. While the effectiveness of CR has been proven in Korea, it is underutilized. This fact sheet summarizes the current status of CR in Korea, including the prevalence of CVD, the clinical practice guidelines for CR programs, and the challenges of implementing CR in Korea.
INTRODUCTION
Cardiovascular disease (CVD) is the primary global cause of mortality, with ischemic heart disease accounting for approximately 12% of disability-adjusted life-years lost annually worldwide. Korea has a lower mortality rate than other countries, but trends of mortality and incidence vary depending on the type of CVD [1,2].
The number of patients with CVD is increasing, and CVD patients are now living longer with their symptoms due to major diagnostic and therapeutic advances in the past few decades. The extended survival of individuals with CVD is contributing to the growing prevalence of CVD, and the absolute number of CVD-related fatalities is expected to rise as the population ages [3-5].
Dual antiplatelet therapy is typically advised for a 12-month period following the onset of acute coronary syndrome. Secondary prevention measures are crucial to emphasize in order to reduce mortality rates. These include rigorous lipid-lowering therapy, antithrombotic treatment, and lifestyle modifications, which can be included in cardiac rehabilitation (CR) [1].
CR is a complex intervention that aims at enhancing cardiopulmonary function, well-being, and health-related quality of life in CVD patients. There is substantial evidence supporting the clinical and cost-effectiveness of CR for patients with acute coronary syndrome [6]. In Korea, numerous studies have confirmed the effectiveness of CR [7-10].
Although contemporary clinical guidelines strongly recommend referring CVD patients to CR, access to CR programs in Korea remains limited. About 40% of patients participate in CR worldwide, but in Korea, the participation rate is lower [11].
This fact sheet provides an overview of the epidemiology of CVD and the current status of CR programs in Korea, encompassing clinical practice guidelines and the implementation, effectiveness, and underutilization of CR. Since CVD is a very broad term, this fact sheet focuses primarily on coronary heart diseases, such as acute myocardial infarction (AMI), angina, and heart failure.
PATTERNS OF CARDIOVASCULAR DISEASE INCIDENCE, PREVALENCE, AND MORTALITY TRENDS IN KOREA
Incidence and prevalence
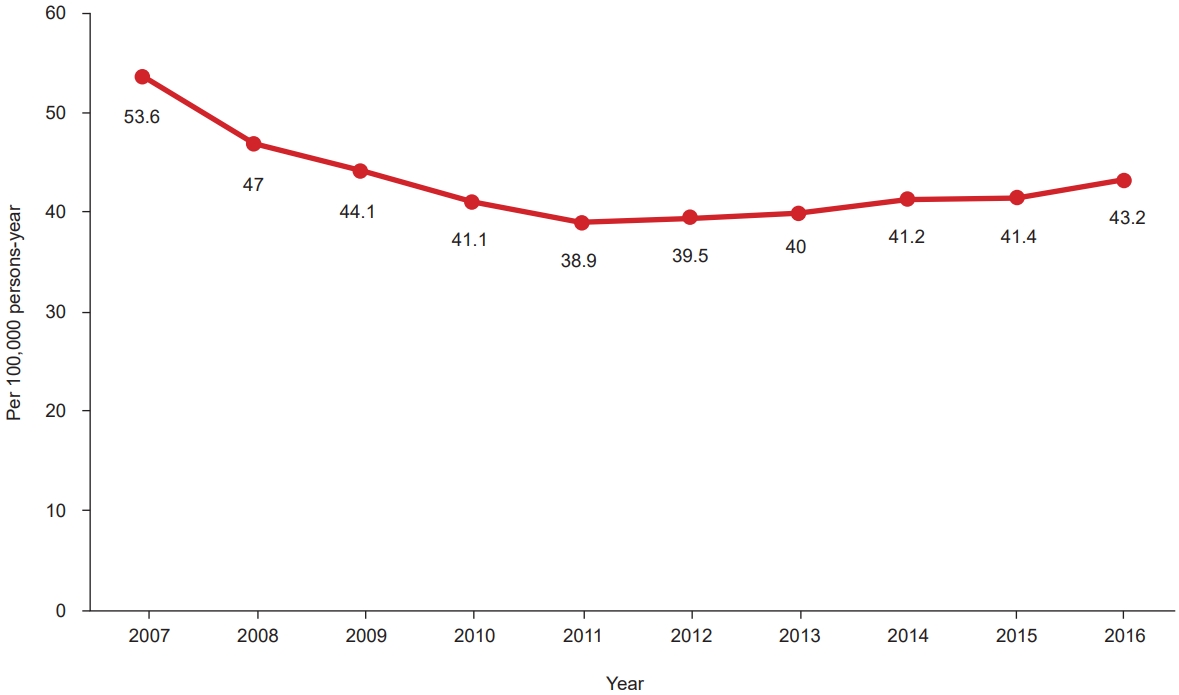
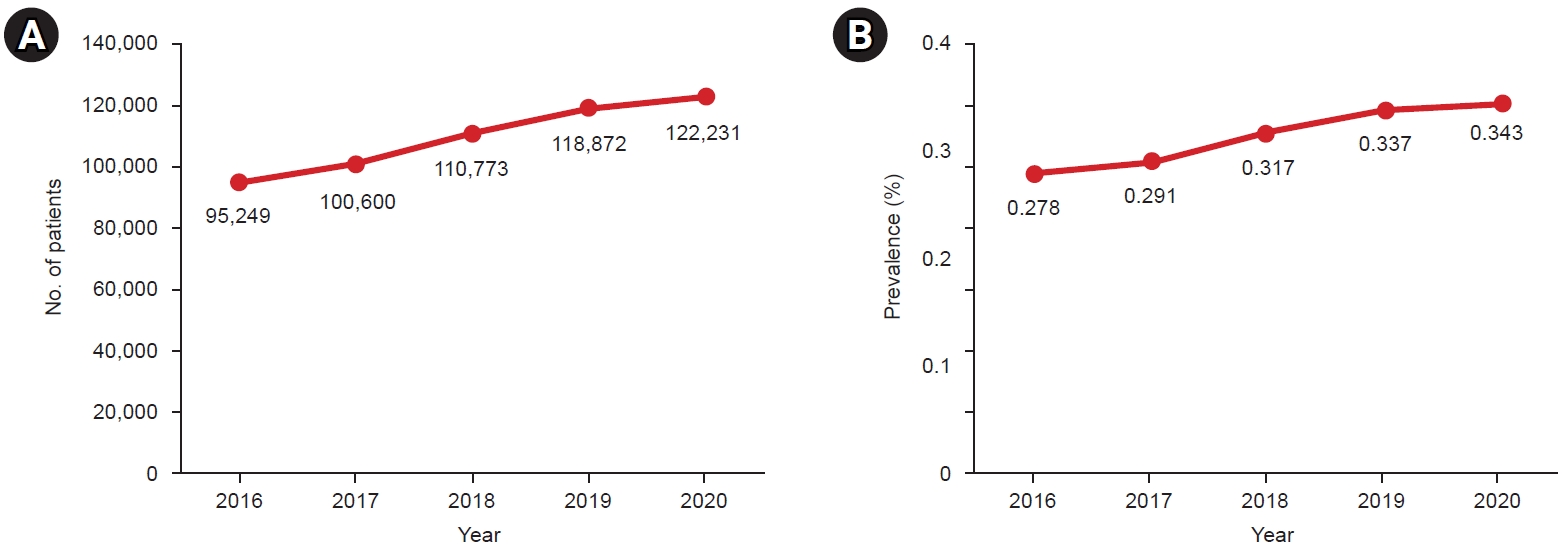
Overall, the prevalence of CVD is increasing [2]. However, the trends in mortality and incidence vary depending on the specific type of CVD. Notably, heart failure is experiencing a rapid increase in both incidence and prevalence. The incidence of AMI peaked in 2006–2007 and has been gradually declining since then. However, it has recently started to rise again. Interestingly, while the incidence of myocardial infarction has not increased in specific age groups, its overall crude incidence seems to be rising due to the growing elderly population (Fig. 1) [12].
In 2016, the age-standardized incidence of hospitalization due to AMI in Korea was 43.2 cases per 100,000 people. When broken down by age group, the incidence of AMI per 100,000 people was as follows: The highest incidence was observed in individuals aged 80 or older, with 321.4 cases per 100,000 people. For those aged 70–79, the incidence rate was 197.4 cases per 100,000. The incidence for individuals aged 60–69 was 117.7 cases per 100,000, while those aged 50–59 had an incidence rate of 66.4 cases per 100,000. Among those aged 30–39, the incidence was 6.9 cases per 100,000. The lowest incidence was recorded for those under 29 years of age, at 0.3 cases per 100,000 [13].
Mortality
Until 1999, CVD was the leading cause of death. However, since that time, cancer has overtaken CVD, making it the second most common cause of death. Data on causes of death from 1983 to 2021, provided by the National Statistical Office of Korea, shows that the mortality rate from all circulatory system diseases decreased from 1982 to 2009, but then increased again from 2009 to 2021. Despite limitations in generalizability due to the inclusion of cerebrovascular disease, these statistics reveal the following trends. The mortality rate was 165.9 per 100,000 population in 1983, dropped to 109.2 per 100,000 population in 2009, and then rose to 121.5 per 100,000 population in 2021. The increase in mortality related to ischemic heart disease was primarily responsible for the overall rise in heart disease mortality in the early 2000s. Conversely, the increase in heart failure mortality was associated with a rise in the 2010s. This recent surge in heart failure mortality in Korea can be primarily attributed to several factors, including an aging population, an increase in CVD survivors, and an improved rate of heart failure diagnoses (Fig. 2) [2,14].
In 2020, there were 9,927 deaths attributed to AMI. The crude mortality rate escalated with age, peaking at 19.3 per 100,000 population (21.8 for males and 16.8 for females). This rate dramatically increased to 260.7 per 100,000 population for individuals aged 80 or older. Importantly, the mortality rate was consistently higher in males across all age groups (Fig. 3) [13,15].
A study analyzing data from the National Health Insurance Service and the National Statistical Office revealed that in 2016, the hospitalization mortality rate (death within 7 days of hospitalization) for AMI patients in Korea who were hospitalized for more than one day was 2.8%. The mortality rates at 30 days, 90 days, 1 year, and 3 years were 6.2%, 8.8%, 13.1%, and 19.7%, respectively. It is notable that inpatient mortality decreased across all these time frames (30 days, 90 days, and 1 year) [13].
CARDIAC REHABILITATION IN KOREA
CR is a multidisciplinary, team-based approach that involves both medical and non-medical professionals. This program is designed to deliver comprehensive, personalized care to patients with CVD. The level of evidence (LOE) is 1++. Typically, the program spans 6–12 weeks and is divided into three phases: inpatient, outpatient, and maintenance. The inpatient phase commences during hospitalization, with a focus on early patient mobilization and complication prevention. The outpatient phase encompasses exercise training, risk factor management, and psychosocial support. The maintenance phase is a lifelong commitment, aiming to sustain the benefits gained during the program and prevent future cardiovascular events. Exercise training is a crucial element of the CR program because exercise enhances cardiopulmonary function, provides symptom relief, and reduces mortality rates in patients with CVD. The exercise regimen usually includes aerobic and resistance training, tailored to individual needs and abilities (LOE: 2++). Risk factor management, including smoking cessation, blood pressure control, and lipid profile management, are also integral parts of the program (LOE: 1++) [6,16,17]. CR is utilized in various countries worldwide, with Western countries in particular having clinical practice guidelines for CR. Each country organizes and applies these clinical practice guidelines for CR according to their specific circumstances [6,18].
Clinical practice guidelines for CR in Korea
In 2019, Korea established clinical practice guidelines for CR. The guidelines contain four main sections: Introduction, Assessments, Exercise Therapy, and Education for Secondary Prevention.
In the Introduction, the guidelines state that CR programs should be an integral component of the treatment approach for individuals recovering from acute coronary syndrome. The initiation of CR exercises should occur promptly following the acute phase of treatment. Additionally, these CR programs should adopt a holistic and interdisciplinary approach to address various aspects of patient recovery and well-being.
In the Assessments section, the guidelines state that customized CR plans should be meticulously crafted to align with each patient’s specific needs. These individualized plans should be based on comprehensive personal assessments of patients who have been referred to CR, including checking for psychological problems. Furthermore, cardiopulmonary exercise testing, which assesses patients’ cardiopulmonary exercise function, is essential for accurately prescribing exercises and predicting outcomes. If implementing a symptom-limited exercise test is challenging, it is advisable to consider using a submaximal exercise test, such as the 6-minute walk test, as an alternative approach.
In the Exercise Therapy section, the guidelines state that CR exercise programs should incorporate aerobic exercise as a fundamental component (or, for better results, high-intensity interval training), as well as resistance (strengthening) exercises. For patient safety during CR exercises, appropriate monitoring should be carried out based on the risk assessment results. Home-based CR programs can be a viable alternative to hospital-based CR programs, especially for low-risk patients. Additionally, it is essential to expand CR programs to include patients aged 65 years or older, as they can benefit significantly from these interventions to improve their cardiovascular health and overall well-being.
In the Education for Secondary Prevention section, the guidelines indicate that a smoking cessation program should be provided. Continuous programs of at least 4 weeks should be considered, and diet programs should also be designed. Food supplements are generally not recommended as a primary or sole strategy for secondary prevention of CVD [7].
Regional cardiocerebrovascular centers in Korea
CR is being implemented through collaboration with the 14 regional cardiocerebrovascular centers (RCCs) in Korea. The locations are as follows: one each in Gyeonggi, Incheon, Gangwon, Daejeon-Chungnam, Chungbuk, Jeonbuk, Busan, Gyeongnam, Ulsan, and Jeju and two each in Gwangju-Jeonnam and Daegu-Gyeongbuk.
RCCs were established to reduce the mortality and morbidity caused by cardiocerebrovascular disease (CCVD) through systematic and efficient operations throughout the entire CCVD cycle, including prevention, early diagnosis, emergency treatment, education, rehabilitation, and management. RCCs actively engage in efforts to narrow healthcare gaps across regions, and their CR programs are expected to serve as examples for post-acute CVD management in Korea.
There are 164 hospitals in Korea that perform percutaneous coronary artery intervention, which include the RCCs (103 are hospitals certified by the Korean Society of Interventional Cardiology). Of these 164 hospitals, 47 (29%) have CR programs (Table 1).
Research on Korean RCCs has indicated that 12 have the equipment, facilities, and medical personnel necessary for CR assessments (two RCCs were excluded from the study due to their short operational period). In addition, patient referral and education are performed relatively well at RCCs, as indicated by the CR referral rate (97%) and the patient education rate (78%). However, the inpatient CR exercise-training participation rate is about 56% and the enrollment rate is 47%, which are lower than the referral rate and the patient education rate. Notably, the outpatient CR program compliance rate is even lower, at around 17% [19,20]. The participation rate refers to the percentage of patients who have undertaken an exercise program for CR. The enrollment rate denotes an outpatient visit for CR following discharge. Finally, adherence refers to the completion of a CR program, which typically lasts between 6 to 12 weeks.
Effectiveness of CR in Korea
As previously noted, CR has numerous beneficial effects. It not only reduces mortality and re-hospitalization rates, but also prevents the recurrence of cardiovascular events and enhances health-related quality of life [6]. The efficacy of CR has been proven by various studies conducted in Korea.
The Eleven Tertiary Hospitals In Korea (ETHIK) study revealed that the 5-year survival rates for participants in CR and non-participants were 96.9% and 93.3%, respectively. The risk ratio for the total 5-year mortality rate among CR participants was approximately 0.41 times that of non-participants. Furthermore, the 5-year survival rate for patients who had suffered an AMI and participated in CR was 59% higher than for those who did not participate [10].
Other reviews have found that the group participating in CR experienced a 28% lower overall mortality rate compared to the group receiving conventional treatment. Additionally, the CR group had lower rates of recurrence and major adverse cardiovascular events compared to the non-CR group. The number of re-hospitalizations was also fewer in the CR group [8]. In Korea, the recovery of cardiopulmonary functions and the improvement of health-related quality of life due to CR have been substantiated. Cardiopulmonary function significantly increased during the initial 12 weeks of CR, and this improvement was sustained for nearly a year [9,18].
UNDERUTILIZATION OF AND BARRIERS TO CARDIAC REHABILITATION
Despite the benefits of CR, its implementation faces several challenges in Korea. CR is strongly recommended, but the actual global CR participation rate is only about 30%–40% [17], and countries are striving to boost participation rates. In contrast, the participation rate in Korea is merely 1.5%, which is significantly lower than in many other countries [21].
There are various reasons for the low participation in CR in Korea. Numerous studies have been conducted to identify the causes, which primarily relate to patient-related factors, hospital-related factors, and factors related to governmental health policies in CR.
Patient factors that reduce participation in CR often include logistical issues or comorbidities/functional statuses. Groups that particularly exhibit low participation rates include the elderly, females, and rural residents. The reduced participation rate among elderly patients can be attributed to mobility challenges related to comorbidities, as well as transportation limitations. The lesser involvement of women in CR programs may be due to their greater family responsibilities and a lack of free time. Furthermore, the self-reliant attitudes common in rural areas, combined with limited access to medical facilities, may lead to lower CR participation among rural residents. The inability of patients to accurately recognize the need for and the importance of CR, along with issues of accessibility, cost, and time constraints, also contribute to the low CR participation rate [21-24]. Factors within hospitals that contribute to reduced participation in CR include limited access to CR services, with only a small fraction of patients participating in CR. This is often due to a lack of physician referrals, as many physicians either lack awareness of the benefits of CR or do not prioritize it within their treatment plans [22,23]. A 2020 study revealed that out of 164 hospitals in Korea performing percutaneous coronary interventions, only 47 hospitals (29%) had implemented CR programs, despite being certified by the Korean Society of Interventional Cardiology [20].
There is a lack of public awareness and education about the benefits of CR because many patients and their families are not aware of the program or do not understand its purpose. Therefore, it is important to raise public awareness and provide education about the benefits of CR, as well as its potential to improve patient outcomes. Home-based CR enables patients to continue receiving CR after their cardiopulmonary function has been evaluated in hospitals. However, this approach also leads to underutilization [22,24,25].
Governmental health policy factors also contribute to low CR participation. In Korea, the National Health Insurance Service began providing insurance coverage for CR in February 2017. A survey study aimed at promoting CR participation revealed that healthcare providers underscore the importance of government-provided patient incentives. They perceive the government as playing a pivotal role in ensuring both the time and the right for patients to participate in CR [24]. There is also a shortage of hospitals that offer CR, indicating a need for government attention and effort to introduce community-based programs that can be managed on an ongoing basis [25].
We propose several strategies to address these barriers. To counter low participation rates due to a lack of understanding about the importance or effectiveness of CR, we recommend promoting education about CR to both patients and healthcare providers. Active recommendations from medical staff, comprehensive education on the need for CR, motivational interviewing, and increased autonomy for participation (e.g., scheduling appointments, setting time schedules, and choosing locations) can all contribute to increased participation in CR. Improvements to the insurance system are also necessary to facilitate the active introduction of CR. Hospitals could offer a range of incentives or implement patient-customized CR programs. Another potential solution is the introduction of an automatic referral system or the strengthening of connections with community-based or home-based CR programs. These programs could be offered to patients who are unable to participate due to travel constraints, and the provision of transportation could be considered. To alleviate the cost burden, expanding insurance coverage could be beneficial. Additionally, various campaigns, studies, and research projects will be necessary to raise awareness about CR and underscore its importance at the government level (Table 2) [21-25].
CONCLUSION
While the mortality rate from CVD has declined in Korea, the overall burden of CVD continues to rise. This increase is primarily attributed to the rapidly aging population and the growing number of individuals diagnosed with CVD, a trend that is expected to continue. CR is being implemented in Korea for CVD patients, offering numerous benefits such as improved cardiopulmonary functions and reduced risks of re-hospitalization and mortality. Additionally, RCCs are striving to bridge the regional disparities in CR access (Table 3). However, compared to other countries, the participation rate in Korea remains relatively low. The implementation of CR continues to face numerous obstacles, including a lack of awareness, system participation, and medical costs. In this review, we provide an overview of CR in Korea, a resource that healthcare professionals and policymakers can use to strategize for CR implementation.
Notes
Jae-Young Han is an Editorial Board member of Annals of Rehabilitation Medicine. The author did not engage in any part of the review and decision-making process for this manuscript. Otherwise, no potential conflict of interest relevant to this article was reported.
None.
Conceptualization: Han JY. Methodology: Kim KH. Formal analysis: Kim KH. Writing – original draft: Kim KH. Writing – review and editing: Han JY. Approval of final manuscript: all authors.