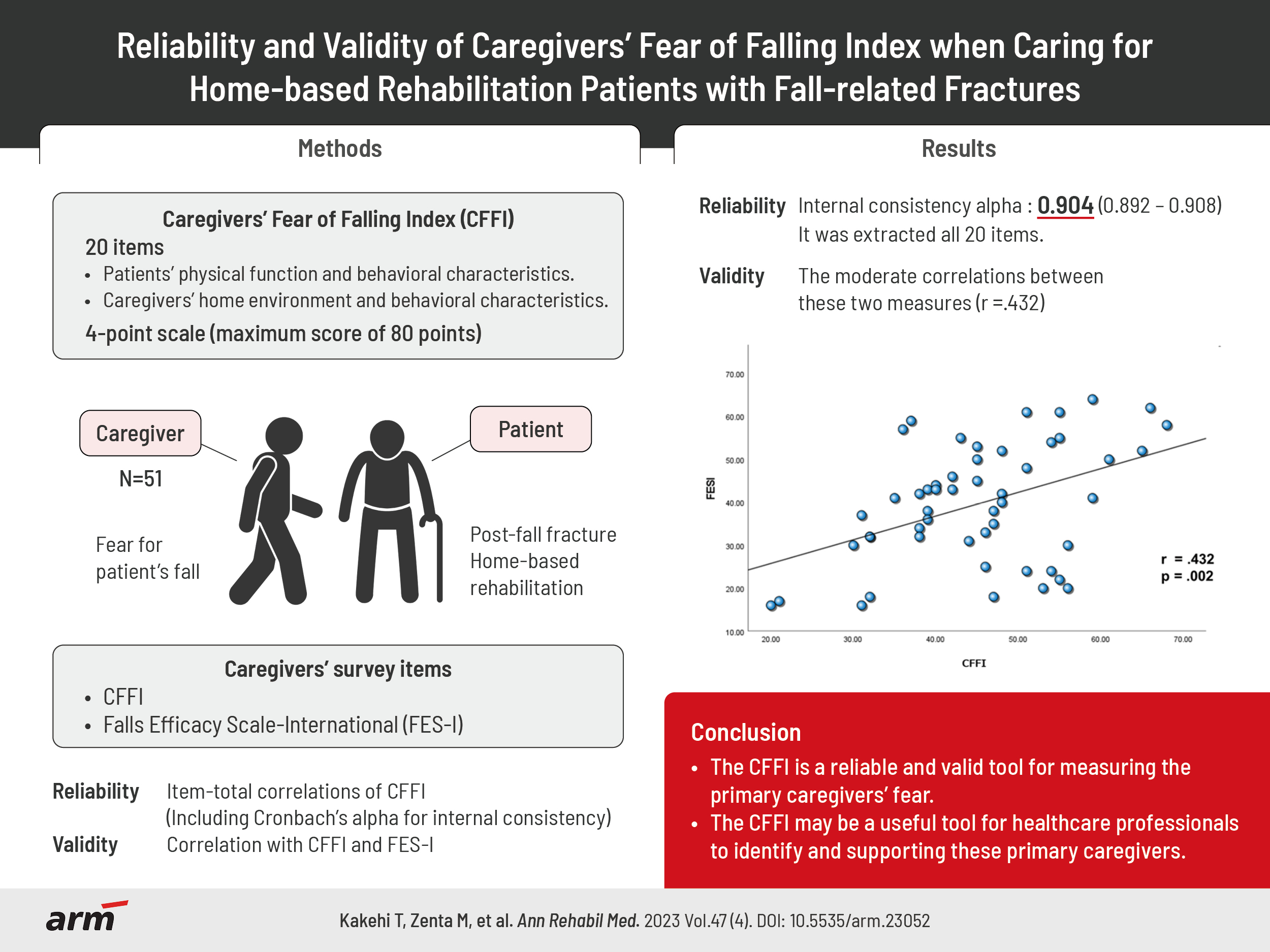
Reliability and Validity of Caregivers’ Fear of Falling Index When Caring for Home-Based Rehabilitation Patients With Fall-Related Fractures
Article information
Abstract
Objective
To evaluate the reliability and validity of this new measure, called the caregivers’ fear of falling index (CFFI).
Methods
The study surveyed home-based rehabilitation patients with fall-related fracture, and their primary caregivers. The characteristics of these patients were evaluated, and the caregivers were surveyed using the CFFI and Falls Efficacy Scale-International (FES-I). The reliability of the CFFI was assessed using item-total correlation, while the validity of the CFFI was evaluated through correlation coefficients calculated between the CFFI and the FES-I.
Results
The participants were 51 patient-caregiver pairs. The internal consistency of the CFFI showed an alpha coefficient of 0.904. No items were excluded in the corrected item-total correlations. The CFFI showed a moderate correlation with FES-I (r=0.432, p=0.002).
Conclusion
This study found the CFFI to be a reliable and valid tool for measuring the primary caregivers’ fear. The CFFI may be a useful tool for healthcare professionals to identify and supporting these primary caregivers.
INTRODUCTION
Fear of falling is a common issue among the elderly, particularly those who have experienced fall-related fractures. It is prevalent in elderly individuals, women, and those with a history of falls. The prevalence can range from 25%–85% [1-4] among community-dwelling elderly [5-8] and is particularly high in patients with femoral neck fractures [9,10]. Fear of falling can decrease physical activity and create a vicious cycle that increases the risk of falling [8], which can lead to a decline in functional abilities [11].
In contrast, there are reports that primary caregivers may also fear that patients with fall-related fractures will fall during activities. In Japan, 66% of primary caregivers are family members residing with care recipients, many of whom are spouses or children [12]. Previous studies of patients with femoral neck fractures and their primary caregivers showed that primary caregivers’ fear may actually be stronger than patients’ fear [13]. Furthermore, it has been suggested that caregivers’ fear of post-fracture patients falling also affects the care burden of primary caregivers [14]. Therefore, while it is important for caregivers to understand their fear of post-fracture patients falling in order for post-fracture patients to continue living at home, no general index exists to evaluate this.
In this context, we developed a scale to measure primary caregivers’ fear [15]. The scale consists of 20 items, including the patient’s physical function and care environment of the primary caregiver. The scale is self-administered, each item is rated on a 4-point scale, and the total score is calculated. Therefore, the aim of the study was to determine the reliability and validity of the measure of a caregiver’s fear of post-fracture patients falling. The scale can be used to evaluate the fear of caregivers and provide them with appropriate support and interventions to alleviate such fear.
METHODS
A cross-sectional study was performed to investigate the psychometric properties of our proposed scale, termed caregivers’ fear of falling index (CFFI). This study was conducted in accordance with the guidelines proposed by Declaration of Helsinki, and the study protocol was reviewed and approved by Institutional Review Board of International University of Health and Welfare (No. 20-Im-027). All participants received verbal and written explanations of the study and provided written consent to participate.
Panel of participants
Participants were patients who have experienced fall-related fractures in the past and received home-based rehabilitation service from July 1, 2021 to December 31, 2022, from data providing institutions, along with their primary caregivers. Home-based rehabilitation is one of the in-home rehabilitation services implemented under the long-term care insurance system in Japan, and it is broadly categorized into home-based rehabilitation and commuting rehabilitation services. The home-based rehabilitation program is based on a comprehensive approach in the home environment, which includes resistance training, gait exercises, and Activities of Daily Living training, as necessary. In many cases, Patients received one-40 minute rehabilitation session per week. The data providers in this study were International University of Health and Welfare Ichikawa Hospital, Mihara Memorial Hospital, Home-Visit Nursing Station Ryugasaki, and Ushiku Aiwa General Hospital. The exclusion criteria were: fall-related fracture before age 65, living alone, the primary caregiver was not the spouse or a child, and the primary caregiver clearly had cognitive decline. Fractures of patients that occurred within the past 5 years were included. Primary caregiver surveys had to be conducted within one week of the patient’s evaluation.
Measurement of patients’ characteristics
Patients’ data were obtained by rehabilitation personnel at each facility, including: age, sex, relationship with caregiver, long-term care level, fracture site, comorbidities(stroke, intractable neurological disease, diabetes mellitus, heart disease, and neoplasm) Japanese version of Montreal Cognitive Assessment (MoCA-J), Short Physical Performance Battery (SPPB), Barthel Index, and Frenchay Activities Index.
Measurement of caregivers’ fear of post-fracture patients falling
CFFI and Falls Efficacy Scale-International (FES-I) are questionnaires used to assess caregivers’ fear of post-fracture patients falling. This study limited the primary caregivers to those who: live with the patient, are the patient’s spouse or child, and do not have obvious cognitive decline. This was to ensure that caregivers could accurately answer the questionnaires and that their fear of patients’ falls was not influenced by their own cognitive decline. Additionally, the rehabilitation staff provided instructions on how to answer the questionnaires to ensure that the caregivers understood how to complete them correctly.
CFFI is a self-rated questionnaire that measures the fear of falls among primary caregivers of patients with fall-related fractures (Fig. 1). The evaluation items consists of 20 items extracted from our previous study [15]. These 20 items included assessment of patients’ physical function (e.g., 1. She/He has weak legs) and behavioral characteristics (e.g., 13. She/He often get caught up in unstable things), as well as assessment of the caregivers’ home environment (e.g., 15. She/He stays at home alone during the day) and behavioral characteristics (e.g., 17. I’m occupied with personal matters). The questionnaire consists of 20 items, each rated on a 4-point scale: “not at all applicable”=1 point, “not very applicable”=2 points, “somewhat applicable”=3 points, and “applicable”=4 points, with a maximum score of 80 points. Since the questionnaire is targeted specifically at the primary caregiver, the caregiver and patient are explicitly identified at the beginning of the questionnaire as follows: “This questionnaire asks about you and the patient (name).”
FES-I is a self-administered questionnaire that originally asked patients to complete 16 items on an 84-point scale. However, it was also used for caregivers in previous studies [13]. The assessment items of FES-I questionnaire consist of activities that are relevant to daily living and could potentially cause falls, such as taking a bath or shower, walking around the house, and getting in or out of a chair. The respondents, the primary caregivers in this case, were asked to rate their confidence in the patients’ ability to perform each of these activities on a scale. The scale ranged from 4, indicating the most confident, to 1, indicating the least confident. The FES-I was validated for reliability and validity by Yardley et al. [16].
Statistical analysis
For statistical analysis of CFFI, various methods were used to examine its reliability and construct validity. To examine reliability, item-total correlations were calculated, including Cronbach’s alpha for internal consistency. The mean, variance, correlation coefficient with total score, and Cronbach’s alpha were also calculated for each of the 20 items in CFFI, when each item was deleted. The sample size in this study was set at 48 participants, with an alpha of 0.8 based on Cronbach’s alpha sample size calculation [17]. To determine construct validity, correlations with FES-I for primary caregivers were determined. Shapiro–Wilk examination was conducted to assess the normality of CFFI and FES-I. The data were analyzed using IBM SPSS 25 (IBM Corp.). A p-value less than 0.05 was considered significant; no correction for multiple testing was performed.
RESULTS
The characteristics of participants
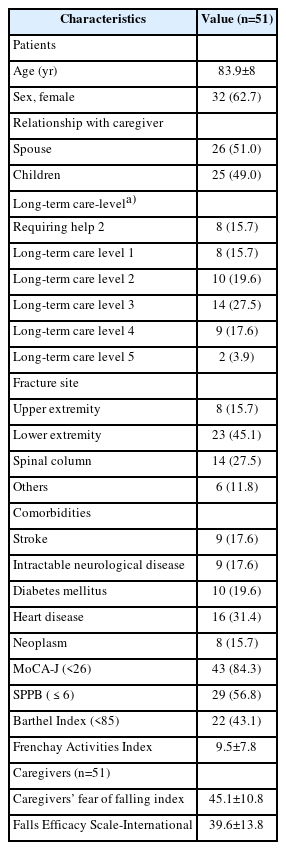
There were 51 study participants (each participant being a patient and caregiver pair). The characteristics of the patients are described in Table 1. The mean age of the patients was 83.9±8.6 years, and 62.7% (n=32) were female, 84.3% (n=43) showed a cognitive decline with MoCA-J scores<26 [18], and 56.9% (n=29) had a high risk of falls with SPPB scores≤6 [19]. The caregiver relationships were spouse in 51.0% (n=26), and children in 49.0% (n=25).
Evaluation of reliability
The mean CFFI score for the 51 primary caregivers was 45.1±10.8, with a variance of 115.5. The internal consistency of CFFI showed an alpha coefficient of 0.904. The results of item-test correlation analysis are shown in Table 2. Corrected item-total correlations were greater than 0.2 for all items (range, 0.221–0.758). Cronbach’s alpha if an item was deleted revealed positive and significant values (range, 0.892–0.908).
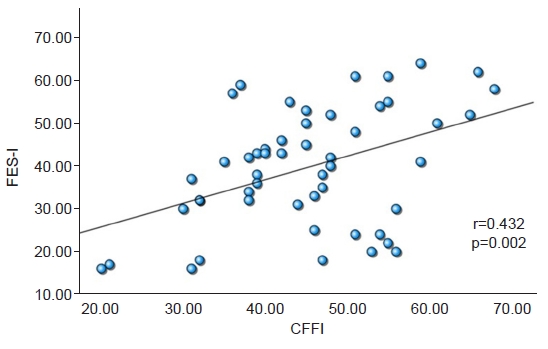
Evaluation of validity
Correlation coefficients between the CFFI and the FES-I were calculated to assess criteria-related validity (Fig. 2). The normality of CFFI and FES-I was calculated by the Shapiro–Wilk test, and both had a normal distribution. CFFI and the FES-I were shown to be significantly correlated (r=0.432, p=0.002), indicating that the index is a valid measure of caregivers’ fear of post-fracture patients falling.
DISCUSSION
This study investigated the reliability and validity of CFFI in a sample of primary caregivers caring for community-dwelling patients with fall-related fractures. The internal consistency alpha was 0.904 (0.892–0.908), indicating high-level consistency. The correlation with FES-I was 0.432, indicating a moderate correlation. The strength of this study was that it standardized the measurement of caregivers’ fear of post-fracture patients falling, for which a commonly utilized index does not exist. This index can be used to examine whether the caregivers’ fear of post-fracture falls affects the functional ability of the post-fracture patients. This is because excessive fear from primary caregivers may potentially decrease the activity levels of the post-fracture patients. If it is found that primary caregivers’ fear is indeed a factor that negatively impacts the functional ability of the post-fracture patients, healthcare professionals should not only support primary caregivers in improving the environment for fall prevention and teaching appropriate caregiving techniques but also provide guidance to help primary caregivers themselves manage their excessive fear. It is important to empower caregivers to support patients in leading as independent a life as possible.
An item-test correlation is a measure of the association between an individual item on a test or questionnaire and the overall test score. It is used to assess the extent to which an individual item is related to the construct or trait that the test is designed to measure. Item-test correlation is often used as an indicator of item quality and as a way to determine which item to include in or exclude from a test [20]. It is generally accepted that items with a corrected item-total correlation below 0.2 should be considered for exclusion [21]. Because the corrected item-total correlation was greater than 0.2 (range, 0.221–0.758), no items were excluded.
It is possible that the high degree of consistency noted in the present study, limited to patients living at home, could be related to the fact that the participants all shared similar experiences. Thus, they may have been more likely to respond in a similar way to items in the questionnaire, resulting in a higher degree of consistency across the items. This increased consistency may also be an indication that the questionnaire assesses a specific aspect of the construct that is relevant to the population studied and less relevant to other populations. However, it is important to note that other factors, such as the quality of the test items, the validity of the construct being measured, sample size, and representativeness of the population studied also have an impact on the degree of consistency noted in the study.
A moderate correlation between CFFI and FES-I scores could indicate that there is a relationship between the two measures, but it is not a strong one. This could be due to the difference in scope between the two measures. For example, FES-I assesses the self-reported confidence and perceived control of individuals to prevent falls, and other measures may assess the physical or cognitive abilities that can affect fall risk, such as balance, gait, or muscle strength [22]. Thus, the moderate correlation between these two measures could suggest that there is some overlap in the construct they measure, but they also assess different aspects of the fall risk.
There are three limitations of this study to consider. The first is that the number of participants in this study was relatively small. It was not easy for us to collect a lot of participants for this study sufficiently as we had expected, unfortunately. Now we consider that the inclusion and exclusion criteria for this study was somewhat strict, which could be one of the reasons for this insufficiency. However, on the other hand, we understand that the strictness of these criteria contributed to the appropriate analysis for this study, undoubtedly. The second limitation is that the period between the injury and the present measurement was not unified. In this study, the periods since the injury and living at home differed among the participants. This was because the timing of the start of home-based rehabilitation differed for each participant. It is possible that the experiences of the patients and primary caregivers during the period of living at home may have influenced the results of this scale. The third limitation was that the study failed to take into account the content of the rehabilitation implemented. The study focused on developing a tool to measure the fear of caregivers, but it did not consider the effect of rehabilitation on that fear. Rehabilitation programs can vary markedly in their content, focus, and intensity, and it is possible that certain types of rehabilitation may be more effective in reducing caregivers’ fear of post-fracture patients falling than others [23]. Therefore, it may be beneficial for future studies to investigate the impact of different rehabilitation programs on caregivers’ fear of post-fracture patients falling, and consider the rehabilitation content as a potential moderator of the fear level.
In conclusion, this study found CFFI to be a reliable and valid tool for measuring the primary caregivers’ fear. These results suggest that CFFI may be a useful tool for healthcare professionals to identify and support primary caregivers who fear post-fracture patients falling and design interventions that can alleviate such a fear and support post-fracture patients’ recovery.
Notes
No potential conflict of interest relevant to this article was reported.
None.
Conceptualization: Kakehi T, Kakuda W. Methodology: all authors. Formal analysis: Kakehi T, Kakuda W. Project administration: Kakehi T, Kakuda W. Visualization: Kakehi T, Kakuda W. Writing – original draft: Kakehi T, Kakuda W. Writing – review and editing: all authors. Approval of final manuscript: all authors.
Acknowledgements
The authors acknowledge the rehabilitation therapists of International University of Health and Welfare Ichikawa Hospital, Ushiku Aiwa General Hospital, Mihara Memorial Hospital, and A Home-visit Nursing Station of Ryugasaki for their contributions to the data collection.