Inspiratory Muscle Training in Patients in the Postoperative Phase of Cardiac Surgery: A Systematic Review and Meta-Analysis
Article information
Abstract
To review the evidence about inspiratory muscle training (IMT) in patients in postoperative of cardiac surgery. We conducted this systematic review used the databases Ovid, LILACS, CINAHL, PubMed, PEDro, and CENTRAL. Randomized clinical trials that addressed IMT after cardiac surgery were selected. The outcomes assessed were maximum inspiratory pressure (MIP), maximum expiratory pressure (MEP), tidal volume (TV), peak expiratory flow (PEF), functional capacity (6-minute walk test) and length of hospital stay. The mean difference between groups and the respective 95% confidence interval (CI) were calculated and used to quantify the effect of continuous outcomes. Seven studies were selected. The IMT was superior to the control over MIP 15.77 cmH2O (95% CI, 5.95–25.49), MEP 15.87 cmH2O (95% CI, 1.16–30.58), PEF 40.98 L/min (95% CI, 4.64–77.32), TV 184.75 mL (95% CI, 19.72–349.77), hospital stay -1.25 days (95% CI, -1.77 to -0.72), but without impact on functional capacity 29.93 m (95% CI, -27.59 to 87.45). Based on the results presented, IMT was beneficial as a form of treatment for patients after cardiac surgery.
INTRODUCTION
Cardiac surgery is a procedure associated with increased survival and quality of life, but there are deleterious effects such as worsening pulmonary function and functional capacity [1]. These last two events are related to the decrease in ventilatory muscle strength common in this patient submitted to cardiac surgery, which may increase the length of hospital stay and postoperative complications [1-3].
In this scenario, inspiratory muscle training (IMT) appears as a fundamental strategy to minimize the negative damage caused by the surgical procedure, being a non-invasive technique, with good applicability in the hospital environment and in the intensive care unit (ICU). Some studies suggest that the IMT improve significant the respiratory muscle strength, tidal volume and peak expiratory flow [4-9]. Our group has already demonstrated that performing IMT and decreasing muscle loss is associated with improved functional capacity and potential benefit over the length of hospital stay in patients undergoing coronary artery bypass grafting (CABG) [10,11].
Thus, it becomes necessary to identify the best scientific evidence on the effect of IMT performed in the postoperative period and its influence on the clinical and functional aspects of these patients. The last review on the topic is in 2017 [4]. In recent years, new articles have been published making the update valid. The aim of our work is to review the effects of IMT and its impact on respiratory muscle strength, pulmonary function, functional capacity, and length of hospital stay in patients undergoing cardiac surgery.
METHODS
Protocol and registration
This meta-analysis was completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [12] guidelines. It is registered in PROSPERO (international prospective register of systematic reviews) under number CRD42021218265.
Eligibility criteria
To perform this systematic review, the Population, Intervention, Control, Outcomes and Study type (PICOS) [13] strategy was used, where the Population studied were patients undergoing myocardial revascularization, the Intervention was IMT, compared with patients who did not undergo the training or traditional method. Traditional method was defined as that performed without adjustment based on anaerobic threshold. The Outcomes were related to inspiratory and expiratory muscle strength, pulmonary functional (tidal volume and peak expiratory flow), functional capacity and length of hospital stay. Functional capacity was assessed by a submaximal test called the 6-minute walk test (6MWT). The point in time was until the moment of hospital discharge. Randomized controlled trials were used, without language and year restriction.
Information sources
We performed a computer-based search, querying Ovid MEDLINE, LILACS, CINAHL (Cumulative Index to Nursing and Allied Health), PubMed, PEDro (Physiotherapy Evidence Database), and the CENTRAL (Cochrane Central Register of Controlled Trials). We also searched the list of references from previous systematic reviews and from the clinical trials eligible for this review. The search for the articles started in August 2020 and finished in November 2020.
Search
The research was based on the PICOS [13] strategy previously described and Boolean operators AND and OR. We used as descriptors for the population cardiac surgery, cardiac surgeries, coronary artery bypass graft, CABG, and myocardial revascularization. For the intervention we used exercise, IMT, respiratory exercise, and breathing exercises. For outcomes were muscle strength, maximum inspiratory pressure (MIP), maximum expiratory pressure (MEP), MIP, MEP, inspiratory pressure, expiratory pressure, volume tidal, peak flow, functional capacity, and length of stay. As descriptors for the study design, we use randomized controlled trials clinical trials, and controlled trials.
Study selection
Randomized controlled trials enrolling cardiac surgery patients were included in this systematic review. To be eligible, the clinical trial should have assigned CABG surgery patients to a group of IMT alone. Studies with adults (18 years and older), regardless of sex, were also included. IMT was defined as training methods that applied loads only during inspiration and that aimed to increase strength and/or endurance of the inspiratory muscles.
Exclusion criteria were studies that involved another type of exercise combined with muscle training, aerobic exercises and IMT initiated in the preoperative period.
Data collection process
To extract the selected articles, we checked titles (first stage), abstracts (second stage), and complete reading (third stage). Then, an exploratory reading of the selected studies was carried out one, later, selective and analytical reading. The data extracted from the articles were summarized in authors, magazine, year, title, and conclusions, to obtain important information for the research.
The evaluation of the methodological quality of the studies was carried out by two independent reviewers. When there was disagreement between them, the article was read in full for reassessment. If the disagreement persisted, a third reviewer assessed and made the final decision.
Data items
Two authors independently (ALLC and LOS) extracted data from the published reports using standard data extraction considering: (1) aspects of the study population, such as the average age, sex, number of patients, diagnosis; (2) aspects of the intervention performed (sample size, type of IMT performed, presence of supervision, intensity, frequency, length, and duration of each session); (3) follow-up; (4) loss to follow-up; (5) outcome measures; and (6) presented results.
The quality of each study
Methodological quality was assessed according to the criteria of the PEDro scale, which scores 11 items, namely: 1, eligibility criteria; 2, random allocation; 3, hidden allocation; 4, baseline comparison; 5, blind individuals; 6, blind therapists; 7, blind evaluators; 8, adequate follow-up; 9, intention to treat the analysis; 10, comparisons between groups; and 11, point estimates and variability. Items are scored as present (1) or absent (0), generating a maximum sum of 10 points, with the first item not counting [14].
Whenever possible the PEDro scores were extracted from the PEDro database itself. When the articles were not found in the PEDro database, two trained independent reviewers assessed the article with the PEDro scale. The studies were considered of high quality if they had scores equal to or greater than 6. Studies with scores lower than 6 were considered as having low quality.
Synthesis of results
The presence of heterogeneity was evaluated using the chi-squared test and the I2 statistic. This statistic illustrates the percentage of variability in effect estimates from heterogeneity rather than sampling error.
Statistical assessment
The mean difference (MD) between groups and the respective 95% confidence interval (CI) were calculated and used to quantify the effect of continuous outcomes. For the meta-analysis in which the studies used the same scales, the results were presented as MD and 95% CI. Otherwise, the effects were calculated using standardized mean difference (SMD) and 95% CI. The effect size of the interventions was defined as small (MD<10% of the scale or SMD<0.4); moderate (MD=10%–20% of the scale or SMD=0.41–0.70), or large (MD>20% of the scale or SMD>0.70) [15].
RESULTS
Selection and characteristics of studies
We found 3,512 articles, of which seven studies [3,10,11,16-19] were considered eligible for systematic review (Fig. 1). Table 1 presents the characteristics of the studies.
Results of methodological quality
In the evaluation of methodological quality with the PEDro scale, the scores of seven articles were already available in the PEDro database [3,14,16-19] and that of an article [11] was evaluated by two independent reviewers, as it has not yet was available. The scores ranged from 3 to 7 points on a scale of 0 to 10 points (Table 2). All studies lost points in the items related to the blinding of the patient and therapist, and only three studies [3,11,16] blinded the evaluator.
IMT protocols for different outcomes
Seven studies [3,10,11,16-19] applied IMT after myocardial revascularization followed up to hospital discharge (n=181).
Manapunsopee et al. [16] compared the performance of incentive spirometry associated with breathing exercise with breathing exercise only (n=43); patients were encouraged to perform incentive spirometry 10 times an hour awake and were instructed to perform maximum slow inspirations while holding the sphere for 3–5 seconds, or as long as possible. The study by Zanini et al. [3] was composed of four groups, but for our analysis, the IMT group was compared with the control group (n=10); the training was carried out with the Threshold Respironics IMT, but without reporting the exercise prescription.
Cordeiro et al. [10] compared IMT with conventional physiotherapy treatment (n=25); IMT with a pressure linear load device (Threshold Respironics IMT; Respironics, Inc., Murrysville, PA, USA), with 40% of the MIP, performing 3 sets with 10 repetitions. Barros et al. [17] compared the IMT plus conventional physiotherapy with the control group that performed only conventional physiotherapy (n=15); the IMT protocol was performed with three sets of 10 repetitions, once a day, during all postoperative hospitalization days with a load of 40% of the MIP value.
The study by Matheus et al. [18] compared conventional physical therapy associated with IMT with conventional physical therapy (n=24); IMT was performed daily in the first three days after the surgical procedure, with three series with 10 repetitions, twice a day with a load of 40% of MIP. Cordeiro et al. [11] compared IMT based on the anaerobic threshold with conventional training that was recognized as control (n=21); patients were submitted to exercise prescription according to the glycemic threshold on the first day after the surgical procedure. In the study by Praveen et al. [19] compared the IMT with the control group that performed the usual hospital protocol (n=30); IMT was started on the fourth postoperative day with three series of 10 repetitions, patients were reevaluated on the eighth day and continued training until the 18th postoperative day.
IMT on ventilatory muscle strength
Seven studies [3,10,11,16-19] analyzed the impact of IMT on maximal inspiratory pressure in the postoperative period of cardiac surgery. For the meta-analysis of this comparison, a random model was used (I2=62%, df=6, p=0.02), in which there was a statistically significant difference between the groups in the comparison between the IMT and the control (difference between the means=12.24 cmH2O; 95% CI, 6.74–17.74; Fig. 2A). Another four studies [3,11,17,18] analyzed the impact of IMT on MEP in the postoperative period of cardiac surgery. For the meta-analysis of this comparison, a random model (I2=80%, df=3, p=0.002) was used, in which there was a statistically significant difference between the groups in the comparison between the IMT and the control (difference between the means=15.87 cmH2O; 95% CI, 1.16–30.58; Fig. 2B).
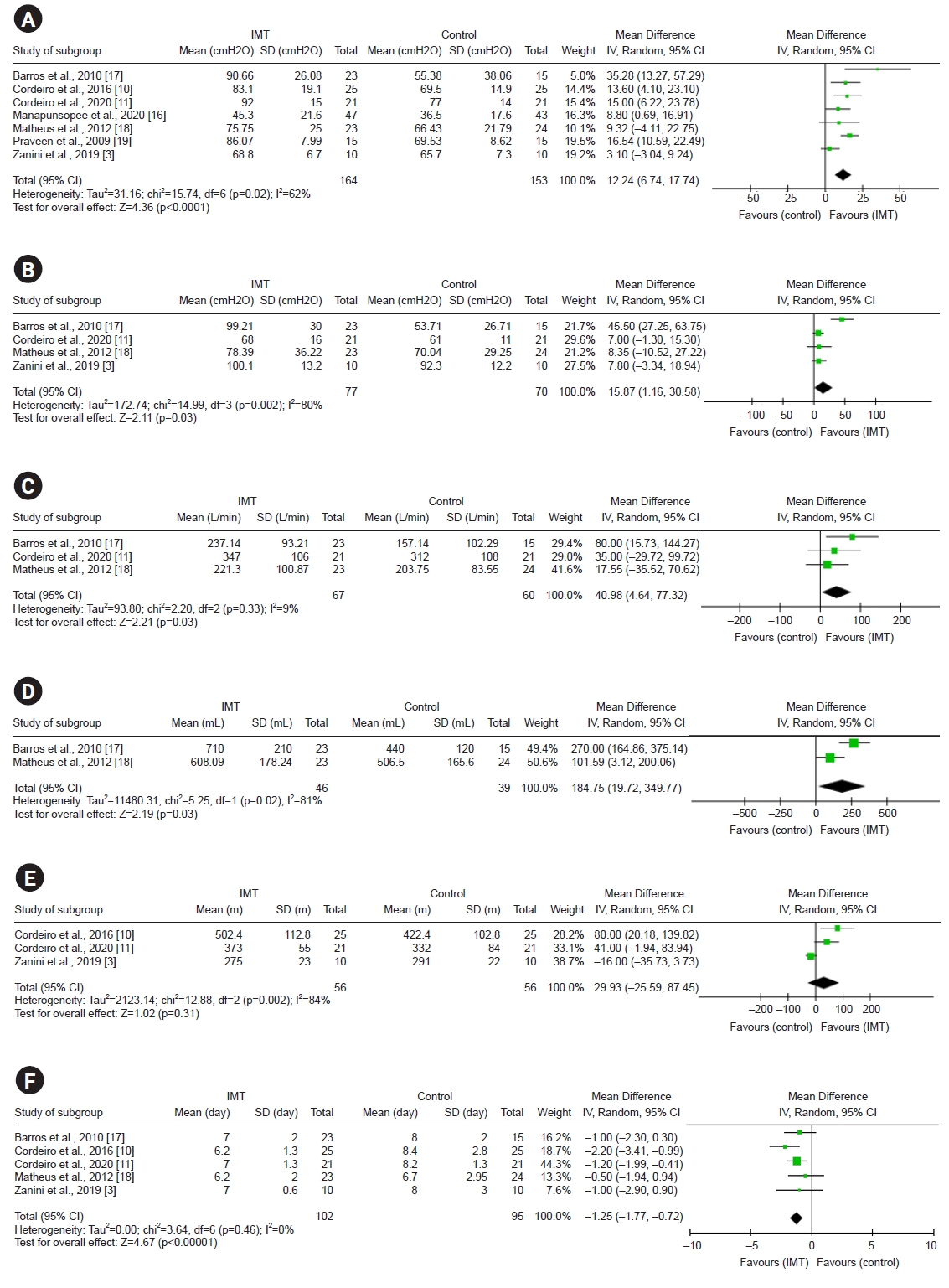
Forest plot of the results of the meta-analysis. (A) Comparison of the inspiratory muscle training (IMT) with the control over the maximum inspiratory pressure outcome. The values presented are the average effects (difference between the means) and a 95% confidence interval (CI). The average effect was calculated using a random-effect model. (B) Comparison of the IMT with the control over the maximum expiratory pressure outcome. The values presented are the average effects (difference between the means) and a 95% CI. The average effect was calculated using a random-effect model. (C) Comparison of IMT with control over peak expiratory flow outcome. The values presented are the average effects (difference between the means) and a 95% CI. The average effect was calculated using a random-effect model. (D) Comparison of the IMT with the control over the tidal volume outcome. The values presented are the average effects (difference between the means) and a 95% CI. The average effect was calculated using a random-effect model. (E) Comparison of the IMT with the control over the functional capacity outcome. The values presented are the average effects (difference between the means) and a 95% CI. The average effect was calculated using a random-effect model. (F) Comparison of the IMT with the control over the outcome length of hospital stay. The values presented are the average effects (difference between the means) and a 95% CI. The average effect was calculated using a random-effect model. SD, standard deviation.
IMT for pulmonary function
Three studies [11,17,18] analyzed the impact of IMT on peak expiratory flow in the postoperative period of cardiac surgery. For the meta-analysis of this comparison, a random model was used (I2=9%, df=2, p=0.33), in which there was a statistically significant difference between the groups in the comparison between the IMT and the control (difference between the means=40.98 L/min; 95% CI, 4.64–77.32, Fig. 2C).
Two other studies [17,18] analyzed the impact of IMT on tidal volume in the postoperative period of cardiac surgery. For the meta-analysis of this comparison, a random model was used (I2=81%, df=1, p=0.02), in which there was a statistically significant difference between the groups in the comparison between the IMT and the control (difference between the means=184.75 mL; 95% CI, 19.72–349.77; Fig. 2D).
IMT to functional capacity
Three studies [3,10,11] analyzed the impact of IMT on functional capacity in the postoperative period of cardiac surgery. For the meta-analysis of this comparison, a random model was used (I2=84%, df=2, p=0.002), in which there was no statistically significant difference between the groups in the comparison between the IMT and the control (difference between the means=29.93 m; 95% CI, -27.59 to 87.45; Fig. 2E).
IMT on length of hospital stay
Five studies [3,10,11,17,18] analyzed the impact of IMT on the length of hospital stay in the postoperative period of cardiac surgery. For the meta-analysis of this comparison, a random model was used (I2=0%, df=4, p=0.46), in which there was a statistically significant difference between the groups in the comparison between the IMT and control (difference between the means=-1.25 days; 95% CI, -1.77 to -0.72; Fig. 2F).
DISCUSSION
Based on the results of our meta-analysis, we found that IMT performed in the postoperative period has a positive impact on inspiratory and expiratory muscle strength, peak expiratory flow, tidal volume and length of hospital stay, but does not alter the functional capacity of this patient profile.
Seven studies [3,10,11,16-19] demonstrated that the IMT performed in the postoperative period had a positive impact on inspiratory muscle strength. Cordeiro et al. [11] highlight that the objective of the IMT is to decrease the loss of strength at discharge, since factors such as sternotomy, pain and immobilization are associated with a decline in postoperative strength. In this study, the beginning of IMT was on the first or second day after surgery and on discharge from the ICU, extending to the third day or hospital discharge.
The reduction in the loss of inspiratory muscle strength may be associated with the improvement of clinical outcomes such as postoperative complications and functional as well as functional capacity [5]. The increase in MIP makes it possible to take deep breaths, increasing lung capacity and reversing hypoventilation and atelectasis, which reduces the incidence of pulmonary complications [4].
Although they are not directly affected by IMT, expiratory muscles also benefit from this treatment option. Our meta-analysis showed a better result in this outcome in the patients who received the training. With the increase in the MEP, the cough becomes effective, allowing the displacement and elimination of bronchial secretions [15]. This hygiene reduces the risk of respiratory infections and may be associated with a decrease in hospital stay [7].
Based on the three studies included in this meta-analysis, which assessed functional capacity in patients undergoing IMT, there was no difference between the interventions. One possible explanation for this lies in the fact that performance on the 6MWT does not depend only on muscle and lung capacity. Cardiac function must also be taken into account, along with factors inherent to the surgical process such as pain.
Another relevant factor associated with the optimization of inspiratory and expiratory muscle strength is the improvement in functional performance. The strengthened diaphragm enhances minute ventilation and increases the delivery of oxygen to the muscle [20,21]. Still on the functional capacity in this meta-analysis, it is worth remembering the high heterogeneity, using a random process in an attempt to equalize, and the low sample size.
The variables of pulmonary function, peak expiratory flow and tidal volume showed positive results among patients who underwent IMT. This improvement is related to the increase in muscle strength and the ability to perform maximum inspirations and exhales [5,22].
A weakness of this study is the limited number of articles that assessed outcomes such as functional capacity. Among the limitations of this review is the heterogeneity of the included clinical trials. Intervention time, form of evaluation and application varied in each study. In addition, the low methodological quality of the work may have influenced the result of this review. Difficulties with keywords and the possibility of studies published in other languages that are not indexed in the databases used may have limited the number of included studies.
To minimize these limitations, we sought contact with the authors, searched for articles with the least possible heterogeneity, and evaluated and weighted the results based on methodological quality.
CONCLUSION
Based on the findings of this systematic review, IMT proved to be effective in improving inspiratory, expiratory muscle strength, tidal volume, peak expiratory flow and length of hospital stay. The only non-significant variable was the functional capacity assessed through the 6MWT.
The evidence brought by this review favors the use of IMT after cardiac surgery in clinical practice. The clinician needs to understand the reasons for muscle weakness and intervene early to restore strength, favoring changes in clinical and functional outcomes.
Notes
No potential conflict of interest relevant to this article was reported.
None.
Acknowledgements
This article is part of André Luiz Lisboa Cordeiro’s postdoctoral work at the Bahiana School of Medicine and Public Health.
Notes
Conceptualization: Cordeiro ALL, Souza LO. Methodology: Cordeiro ALL, Souza LO, Gomes-Neto M. Formal analysis: Cordeiro ALL, Souza LO. Visualization: Gomes-Neto M, Petto J. Writing – original draft: Cordeiro ALL, Souza LO. Writing – review and editing: Cordeiro ALL, Souza LO, Gomes-Neto M, Petto J. Approval of final manuscript: all authors.



