Ultrasonographic Findings of Superficial Radial Nerve and Cephalic Vein
Article information
Abstract
Objective
To investigate the anatomic relationship between the superficial radial nerve (SRN) and the cephalic vein (CV) through ultrasonography due to the possibility of SRN injury during cephalic venipuncture.
Methods
Both forearms of 51 healthy volunteers with no history of trauma or surgery were examined in proximal to distal direction using ultrasonography. We measured the distance between the radial styloid process (RSP) and the point where the SRN begins contact with the CV, and measured the distance between the RSP and the point where the SRN is separated from the CV. The point where the SRN penetrates the brachioradialis fascia was also evaluated.
Results
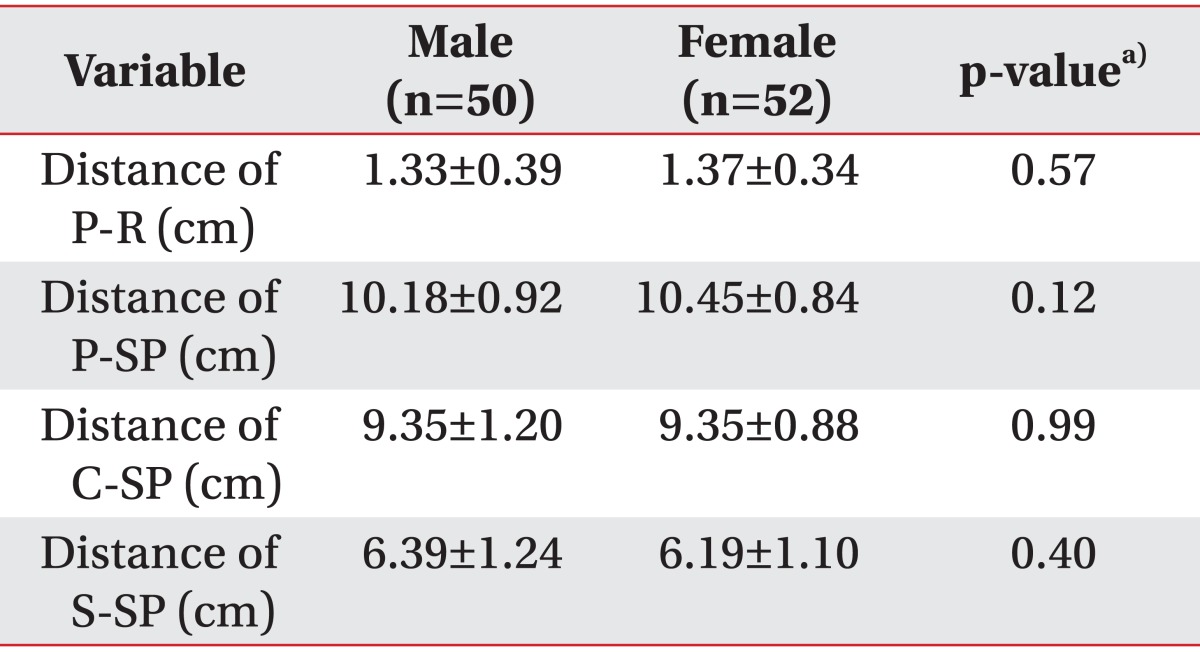
The SRN came in contact with the CV at a mean of 9.35±1.05 cm from the RSP and separated from the CV at a mean of 6.29±1.17 cm from the RSP. The SRN pierced the brachioradialis fascia at a mean of 10.31±0.89 cm from the RSP and horizontally 1.35±0.36 cm medial to the radius margin. All parameters had no significant differences in gender or direction.
Conclusion
The SRN had close approximation to the CV in the distal second quarter of the forearm. We recommend for cephalic venipuncture to be avoided in this area, and, if needed, it should be carried out with care not to cause injury to the SRN.
INTRODUCTION
The superficial radial nerve (SRN) is a terminal sensory branch of the radial nerve that passes along the front of the radial side of the forearm and runs beneath the tendon of the brachioradialis, piercing the deep fascia. It innervates the skin of two thirds of the dorsoradial region of the hand, including the proximal part of the dorsum of the thumb and the proximal portion of one-and-a-half or two-and-a-half adjacent fingers [1]. Obtaining detailed knowledge on the anatomic pathway of SRN could help in approaching the radial region of the forearm and hand during treatment for De Quervain disease, nerve conduction study of the SRN, and localization of regional nerve blockades. On the other hand, the cephalic vein (CV) begins in the radial part of the dorsal venous network and winds upward around the radial border of the forearm, receiving tributaries from both surfaces. This vein that is superficial in the distal forearm and easily visible through the skin is a good candidate for venous access. However, its close proximity to the SRN increases the risk of nerve injury during CV cannulation or puncture. Nerve injury may lead to neuroma formation and possible wrist and hand pain that may be difficult to treat. Although painful neuromas can occur after injury to any nerve, the superficial branch of the radial nerve is more likely to develop this painful syndrome [2]. A variety of therapies, including nerve grafting and the implantation of the nerve into bone or muscle, have been successful in alleviating the pain in some patients [3]. Thus, an understanding of the anatomic location of the SRN and CV is important for the prevention of nerve injury. A recent study examined anatomic relationships of the SRN, CV, and styloid process of radius from 10 cadavers [4]. Another study focused on venipuncture-induced neuropathic pain, type of nerve fibers affected, and sympathetic nervous system effects [5]. However, studies on ultrasonographic evaluation for SRN and CV of healthy adults have been lacking. Thus, to identify the appropriate site for venipuncture of the CV in the distal forearm to decrease the damage of the superficial branch of the radial nerve, we evaluated the anatomic relationship between the SRN and the CV in the forearm through ultrasonographic examination.
MATERIALS AND METHODS
In our prospective study, we recruited healthy subjects who had no history of trauma or upper extremity surgery and also presented normal findings in a neurologic examination. We obtained the approval from the Institutional Review Board at our hospital before conducting the study, and all subjects gave informed, written consent for their inclusion in this study.
The height and the forearm length of the participants were measured. The length of the forearm was defined as the distance from the radial styloid process (RSP) to the antecubital skin crease with the forearm in neutral position.
Ultrasound scanning of both SRN was performed by a single sonographer who is experienced in musculoskeletal ultrasonography, using the Accuvix XQ system (Medison, Seoul, Korea) with a linear 6-2 MHz high resolution transducer. Keeping the volunteer's wrist halfway between pronation and supination, the lateral aspect of the forearm was examined. The SRN was scanned in proximal to distal direction using the continuous tracing method with the transducer placed transversely to the course of the SRN. The SRN was identified in the proximal third of the forearm based on its location between the brachioradialis and the radial artery and was scanned under the cover of brachioradialis. The transducer was then moved distally to obtain the point (Point 3) where the SRN pierces the brachioradialis fascia as well as the contact (Point 1) and separating points (Point 2) between the SRN and the CV. We measured 1) the distance between the contact point and the RSP; 2) the length from the separating point to the RSP; 3) the distance between Point 3 and the RSP; and 4) the horizontal distance between Point 3 and the radius margin (Fig. 1). Each point was identified by sonography, and the distance was measured on the skin with a tapeline. Color Doppler was also used to identify the radial vessels and to establish the relation of the nerve and vessels. For statistical analysis, SPSS ver. 18.0 for Windows (SPSS Inc., Chicago, IL, USA) was used. The independent t-test was used to analyze the differences between male and female participants. Right- and left-side SRNs were compared using paired t-test. Two-tailed p-values less than 0.05 were considered statistically significant.

Distribution of superficial radial nerve (A) and cephalic vein (B) in the forearm. A, point at which the superficial radial nerve pierced brachioradialis fascia; B, contact point of superficial radial nerve with cephalic vein; C, separating point of superficial radial nerve with cephalic vein; BR, brachioradialis; LACN, lateral antebrachial cutaneous nerve; SRN, superficial radial nerve; EPB, extensor pollicis brevis; APL, abductor pollicis longus; ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus; FCR, flexor carpi radialis.
RESULTS
A total of 102 SRN from both forearms of 51 volunteers (25 men and 26 women) were examined for the study. The age range was 22-81 years (mean±standard deviation, 52.08±19.76 years). The mean height was 163.14±7.13 cm, and the mean forearm length was 22.30±2.31 cm. The SRN had a bright echogenic texture with hypoechoic fascicles similar to the honeycomb appearance of other peripheral nerves (Fig. 2). After becoming subcutaneous by penetrating the brachioradialis fascia, the SRN came to be close to the CV from beneath the vein and had the contact point with the CV at a mean of 9.35±1.05 cm from the RSP. The SRN separated from the CV at a mean of 6.29±1.17 cm from the RSP. The point where the SRN became subcutaneous was at a mean of 10.31±0.89 cm proximal to the RSP. The SRN pierced the brachioradialis fascia horizontally at a mean of 1.35±0.36 cm medial to the radius margin. There was no significant statistical difference between the right and left sides in all the values (Table 1). All of the above parameters were compared between male and female patients by using independent-sample t-test. There was no significant statistical difference between male and female participants (Table 2).
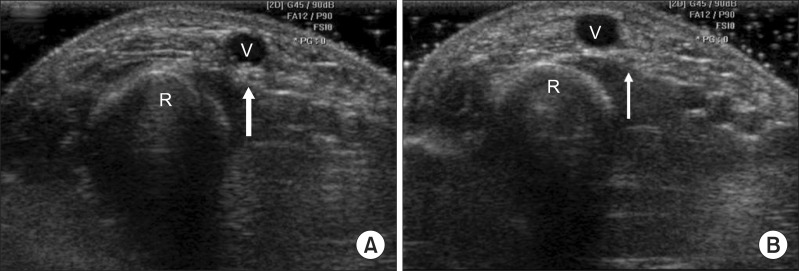
Ultrasonographic images of the forearm where (A) the superficial radial nerve (arrow) begins to contact the cephalic vein and (B) the superficial radial nerve is separated from the cephalic vein. V, cephalic vein; R, radius.
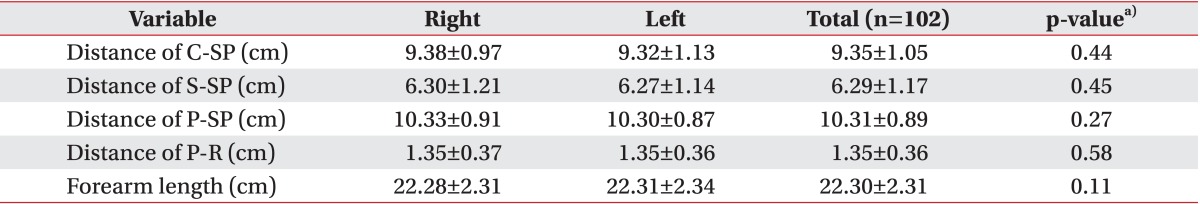
The measured distances from the radial styloid process to the superficial radial nerve and the point at which the superficial radial nerve pierced fascia
DISCUSSION
The present study was conducted to evaluate the SRN and the CV in the forearm by ultrasonography and revealed the close anatomical relationship between the SRN and the CV in the distal forearm. The SRN started to contact the CV at 9.35±1.05 cm distance from the RSP and was separated from the CV at 6.29±1.17 cm distance from the RSP.
The SRN emerges just dorsal to the brachioradialis muscle in the mid-forearm, and it terminates in fine sensory branches at the level of the wrist and over the dorsum of the hand [6]. Injury to this nerve results in a variable area of anesthesia that may include the dorsal surfaces of the proximal halves of the thumb, index, and middle fingers. It is usually limited to a triangular area on the dorsum of the web between the first and second metacarpal [2]. Although the distribution of the SRN has been described in anatomic textbooks, the characteristics of its pathway which are related to its clinical importance have not been clearly demonstrated. Also, the majority of the studies have been focused on the SRN of cadavers. In one study on anatomic variation of SRN using cadavers, the SRN became subcutaneous at a mean of 9.20 cm and bifurcated at a mean of 4.90 cm proximal to the styloid process of the radius in 48 specimens [7]. Another anatomic study of the SRN and the CV in 14 hands from 10 cadavers reported that the mean distance from the styloid process of radius to the point at which the SRN pierced fascia was 79.9±9.84 mm (range, 60 to 93 mm) and from the styloid process of radius to the crossing point of the SRN with the CV was 29.5±15.24 mm (range, 13 to 55 mm) [4]. These findings that are inconsistent with the present study may be due to a distinction between cadavers and living subjects. The cadaveric study could have a measurement error because of the transposition of anatomic structures, especially of such structures as subcutaneous nerves or vessels, occurring during dissection. In contrast, ultrasound is able to search the anatomic constructions without transposition. In addition, there is some benefit of the ultrasonographic evaluation. It provides anatomic information not available with electrodiagnostic studies, and it is readily available, is inexpensive, does not involve radiation exposure, and is painless [8]. It can provide information about nerve structure to help assess nerve pathologies. Many studies have reported the usefulness of ultrasonography to investigate nerve diseases [9]. On the other hand, acquisition of accurate ultrasonographic images depends on the operator. Our ultrasound scanning of both SRN was performed by a single sonographer, so inter-rater reliability was not evaluated. Also due to the size of SRN being very small, technical errors, like misinterpretation, can occur. These might have effected a discrepancy between this study and the cadaveric study. Injury to the SRN has been reported after trauma and surgery [10] and during routine peripheral vein cannulation. Injury resulted in the development of a neuroma and considerable discomfort and disability [2]. According to a recent study on the histological and ultrasonographical findings of the SRN, with advancing age, the changes in SRN intraneural anatomy were noticed in the form of an increased amount of adipose tissue in the interfascicular domains. These findings may help to explain poor prognosis with advancing age following repair [11]. In another study on nerve evaluation using ultrasonography, most nerves in the upper extremity showed a clear fascicular pattern similar to that of a honeycomb. However, according to other reports, small nerves, such as the superficial radial or posterior interosseous nerve, appeared as only 1 hypoechoic fascicle with an oval shape [9].
To our knowledge, this is the first attempt to evaluate the anatomic relationship between the SRN and the CV in living subjects through ultrasonographic examination. The current study demonstrated the close anatomical relationship between the SRN and the CV in the distal forearm through ultrasonography. This implies that the cephalic venipuncture in the distal forearm requires close attention to the possibility of the SRN injury. Furthermore, we investigated the point where the SRN pierced the brachioradialis fascia and became subcutaneous. This result provides the appropriate stimulation site in an SRN conduction study for optimal response of sensory nerve action potentials.
This study has several limitations. First, most participants were Asian and of old age with relatively short statures which could influence the forearm length and the results. Second, the SRN and the CV were measured with the forearm in neutral position only. There is a possibility of a change in the measurement data according to the forearm position, such as pronation. Further studies are necessary regarding this matter. Nonetheless, all of the participants thoroughly completed the ultrasonographic examination without any particular adverse effects.
In conclusion, the SRN has close approximation to the CV in the distal second quarter of the forearm in ultrasonographic examination. We recommend that cephalic venipuncture had better be avoided in this area, that is, the crossing point of the SRN with the CV. If needed, it should be carried out with caution not to cause injury to the SRN. Also, when physicians perform nerve conduction studies of the SRN, the stimulation point within about 10 cm proximal to the styloid process of radius is recommend.
Notes
No potential conflict of interest relevant to this article was reported.