Development and Evaluation of the Korean Version of Hospital-Based Transitional Rehabilitation Program Using Daily Living Home for Spinal Cord Injury
Article information
Abstract
Objective
To develop and evaluate the Korean version of a hospital-based transitional rehabilitation program (TRP), using daily living home for spinal cord injury (SCI) patients.
Methods
In this study, we developed the Korean version of a hospital-based TRP through domestic and overseas surveys and focus group meetings. By applying this to chronic SCI patients, we observed the functional and quality of life (QOL) changes and evaluated the degree of achievement of the core goals set for each patient during hospital-based TRP.
Results
Hospital-based TRP, for 21.8±3.9 days on average, was applied to four chronic SCI patients (two patients with long-term hospital stays and two homebound disabled individuals) with an average injury period of 736.8±185.4 days. The Korean version of the Spinal Cord Independence Measure (49.3±6.9 vs. 62.5±6.0; p<0.05) showed functional improvement at the end of TRP, when compared to that before the TRP. The Korean version of the World Health Organization’s QOL scale, abbreviated version (159.8±36.6 vs. 239.8±36.1; p<0.05), showed improvement in QOL. Goal attainment scaling showed a significant degree of achievement for the core goals through TRP (33.6±4.4 vs. 70.0±2.8; p<0.05). These results confirmed that the effect was maintained 1 month after the end of TRP. Additionally, two patients were successfully discharged after TRP completion, and the other two could start social activities.
Conclusion
The Korean version of the hospital-based TRP, applied to chronic SCI patients, showed the potential to improve the patients’ functioning and QOL and appeared to be effective in successful discharge and social participation.
INTRODUCTION
In the 2017 survey on the status of disabled individuals by the Ministry of Health and Welfare in Korea, the rate of spinal cord injury (SCI) was 3.5% among Koreans with physical disabilities, and there were at least 45,000 registered SCI patients. Since 99.2% of physical disabilities are acquired and 70.8% of these disabilities occur in individuals aged 20–65 years, a considerable number of SCI patients experience impairment during their active social life [1]. It is known that distress, depression, and frustration due to a disability can have a huge impact on mental health; therefore, a careful, multidisciplinary approach must be implemented to assist SCI patients to return to society [2,3].
Data on the current status of SCI patients in Korea are scarce; nonetheless, the report published in 2018 by the Korea Spinal Cord Injury Association (KSCIA) revealed that 62.7% of cases were referred to more than three hospitals until discharge and that the average duration of inpatient treatment was 30.8 months [4]. This is significantly longer than the data reported by SCI registries worldwide. In a 2018 New Zealand report, the average length of hospital stay from injury to discharge was 76.9 days, compared to 53.0 days in the United States between 2015 and 2020 [5,6]. This indicates the absence of an integrated rehabilitation system, from acute phase rehabilitation to return to society, despite the high level of medical care in Korea. It can be presumed that an extended hospital stay leads to unnecessary medical expenditure, dependency of SCI patients, and secondary family-related problems due to dysfunction in the household, resulting in social losses for individuals, families, and even the state.
In contrast, in other countries, the following three types of SCI rehabilitation systems exist: (1) national spinal injury centers, such as those seen in the UK and Switzerland, which provide treatment from the acute stage until the rehabilitation stage and ensure a smooth return to society, along with integrated follow-up management within a single national institution [7,8]; (2) SCI rehabilitation centers in accredited hospitals with completed certifications, such as the American Spinal Cord Injury Model System [9]; and (3) supporting a smooth return to society through a transitional rehabilitation program (TRP) prepared during the period of discharge, which is implemented in Australia and New Zealand [10,11]. In any case, efforts are being made for SCI patients to achieve a quick and safe return to society through a multidisciplinary approach, with the intention of shortening the period of hospitalization and increasing the rate of home discharge [5,6].
In the present study, we developed the Korean version of a hospital-based TRP for SCI patients using daily living home (DLH), a space in the hospital where patients could be taught to perform the activities of daily living (ADL), and evaluated its effectiveness for SCI patients.
MATERIALS AND METHODS
Development of the Korean version of hospital-based TRP
Survey of the current status of domestic and overseas transitional rehabilitation
The content of the rehabilitation programs provided to SCI patients by a total of six national, public, and private medical institutions in Korea and one non-medical institution (KSCIA), were investigated through electronic documents, publications, and in-person visits [12,13]. With respect to overseas programs in the UK (London Spinal Injuries Center), Switzerland (Swiss Paraplegic Center), USA (Rehabilitation Institute of Chicago), Australia (Princess Alexandra Hospital), New Zealand (Burwood Hospital), Sweden (Rehab Station Stockholm), and Japan (Kanagawa Rehabilitation Center), seven public and private medical institutions provided information on rehabilitation programs for SCI patients through electronic documents, publications, and e-mails from relevant institutions [7-11,14,15]. Among these, we visited medical institutions in New Zealand and Japan and conducted an on-site survey.
Focus group composition
The focus group (FG) consisted of the following: five rehabilitation medicine specialists, five KSCIA members, three executives and occupational therapists from the Korean Association of Occupational Therapists, three social workers and welfare administration experts, one specialized nurse in the spinal cord rehabilitation ward, three SCI patients who were actively socializing, and one administrative officer with disabilities in the metropolitan city. Opinions were exchanged and communicated through FG meetings and Delphi surveys and were reflected in the development of the prototype and improvement proposals for the TRP.
Development of the hospital-based TRP and pilot application
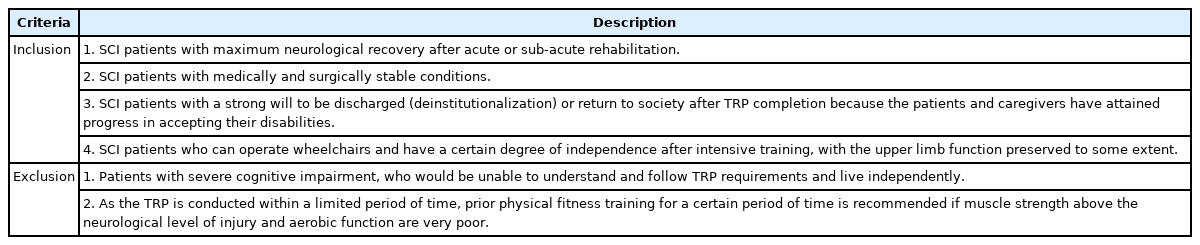
The prototype of the hospital-based TRP was developed through domestic and overseas surveys and FG meetings. After confirming the prototype for the definition of hospital-based DLH, subject criteria, composition of the multidisciplinary team, and program content, a pilot trial was conducted to evaluate the effectiveness of the hospital-based TRP. The subjects included SCI patients who met all of the following criteria: (1) maximum neurological recovery after acute or sub-acute rehabilitation, (2) medically and surgically stable condition, (3) a strong will to be discharged (deinstitutionalization) or return to society after TRP completion; and (4) who can operate wheelchairs and have a certain degree of independence after intensive training, with the upper limb function preserved to some extent. A final improved proposal was developed after feedback from the pilot application, FG meetings, and Delphi surveys.
Effect evaluation of the hospital-based TRP
To evaluate the effectiveness of the hospital-based TRP, the following items were assessed prior to implementation of the TRP (Evaluation 1 [E1]), at the end of the TRP (Evaluation 2 [E2]), and 1 month after the TRP (Evaluation 3 [E3]). Neurological status was evaluated using the American Spinal Injury Association impairment scale (AIS). Functional evaluation was performed using the Korean version of the Spinal Cord Independence Measure (K-SCIM), Seoul-Instrumental Activities of Daily Living (Seoul-IADL), and the Canadian Occupational Performance Measure (COPM). Social welfare was evaluated using the Rehabilitation Institute of Chicago Functional Assessment Scale (RIC-FAS). Psychological conditions were evaluated using the Korean version of the Beck Depression Inventory (K-BDI), Beck Anxiety Inventory (K-BAI), and Beck Hopelessness Scale (K-BHS). Quality of life (QOL) was evaluated using the Korean version of the World Health Organization’s QOL scale, abbreviated version, (K-WHOQOL-BREF) and the Korean version of the Community Integration Questionnaire (K-CIQ). Furthermore, Goal Attainment Scaling (GAS) was used to evaluate core goal achievement.
Statistical analysis
The Friedman test was used for nonparametric testing of continuous variables repeatedly collected through E1, E2, and E3. Statistical significance was set at p<0.05. The Wilcoxon signed-rank test was used for E1 and E2, E2 and E3, and E1 and E3 as a post-hoc test for statistically significant data set by the Friedman test. The statistical significance level for each test was set at p<0.017 by applying the Bonferroni correction. Collected data were statistically analyzed using SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
Ethics statement
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of Chungnam National University Hospital (No. 2019-05-047). Informed consent was provided by all subjects at the time of their enrollment. The purpose of the study and the process were fully explained to the patients. A separate financial incentive was not provided to the subjects, and all expenses for the evaluation and TRP, including inpatient hospital room fees and food expenses, were paid as research expenses.
RESULTS
Development of the Korean version of hospital-based TRP
The prototype was developed and then improved through feedback from pilot applications, FG meetings, and Delphi surveys.
Definition of the hospital-based DLH
The DLH was defined as an operational space that could maximize the potential for challenges expected in ADL after being discharged from the hospital (Fig. 1).
Proper time and subjects for the TRP
Hospital-based TRP application was considered effective for SCI patients who met the conditions described in Table 1. Considering neurological recovery after injury, 6 months to 1 year (or later) after SCI was considered appropriate.
Multidisciplinary team composition for the TRP
For the hospital-based TRP operation, a multidisciplinary team consisting of personnel listed in Table 2 was required. Members who were not qualified as health care professionals from health authorities included case managers, independent living coaches (ILCs), and program assistants. The case manager was in charge of one person in the multidisciplinary team and conducted the TRP process, including in-depth interviews with subjects before starting and collecting feedback during the TRP. The ILC, as a peer disabled person, undertook the ADL training and transfer of know-how, including counseling for the subject. Program assistants provided safety and excellence in performing the hospital-based TRP by assisting with activities.
Process of the hospital-based TRP
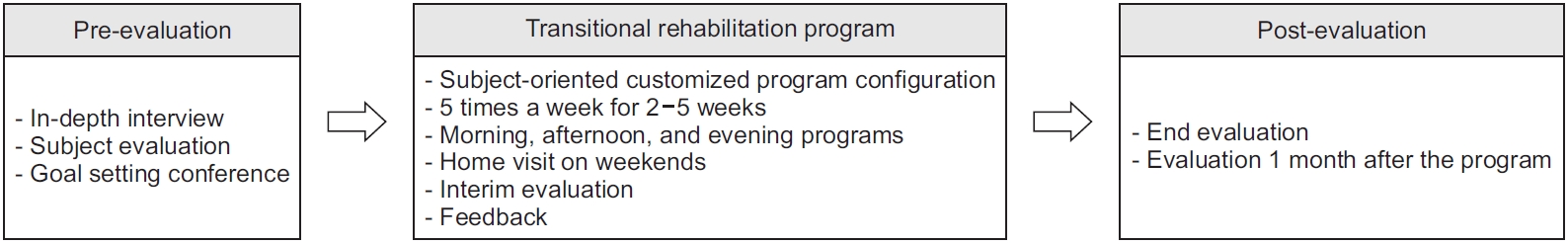
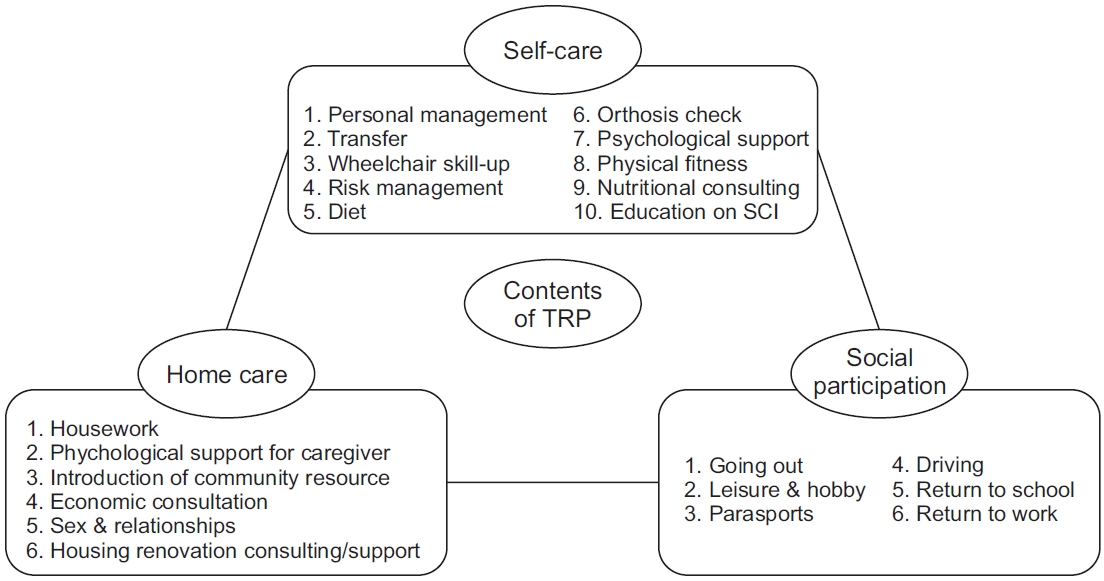
The TRP process consisted of pre-evaluation, TRP implementation, and post-evaluation, as shown in the flowchart in Fig. 2. In the pre-evaluation period, the case manager conducted an in-depth interview with the subject and the caregiver. This was based on the International Classification of Functioning, Disability and Health (ICF) model to identify the subject’s degree of disability, physical function, activity and social participation; internal and external factors; and clarify the needs that the subject wanted to meet during the TRP (Fig. 3). Based on this, a goal-setting conference was held in the presence of a multidisciplinary team, target audience, and caregiver. Here, 5–6 core goals (which reflected the subject’s desires but were adjusted realistically by considering the subject’s condition) were set up. A subject-oriented customized program was formed to achieve them; however, among the TRP content shown in Fig. 4, the content thought to be needed by the subject could be added through discussion within the multidisciplinary team. The TRP duration was flexibly adjusted within a period of 2–5 weeks with consideration of the initial and intermediate evaluation results. Hospital-based TRP proceeded in the morning/afternoon in a space other than the DLH or in the DLH according to the program content, and it was common practice to stay at the ward for safety after completion. ADL training was conducted with a group of three persons (subject, ILC, and program assistant) according to the level of risk, and the self-care item during ADL training was assigned an ILC in consideration of sex and neurological level of injury (NLI). The case manager received feedback from the subject and the multidisciplinary team during the program and, on Friday afternoon, a plan for the next week was organized after discussion with the subject (Fig. 5).

The International Classification of Functioning, Disability, and Health model-based on in-depth interview items.

Example of the week one program for subject #5. DLH, daily living home; QOL, quality of life; CM, case manager; PC, psychology counselor; PFP, physical fitness program; PTR, physical therapy room; PT, physical therapist; OTR, occupational therapy room; OT, occupational therapist; OrT, orthosis technician; SW, social worker; ADL, activities of daily living; CIC, clean intermittent catheterization; ILC, independent living coach; PA, program assistant.
Results of the pilot application of the hospital-based TRP
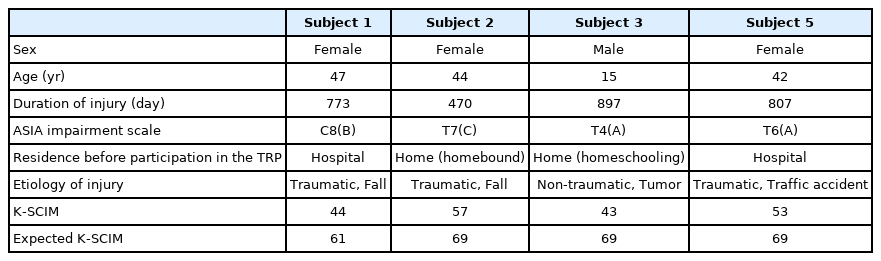
Patient demographics
Five SCI patients participated. In the fourth subject, a fracture of the left distal femur occurred during a home visit after completion of the second week, and the program was discontinued. The other four patients completed the program as planned. The average duration of injury was 736.8±185.4 days, and two patients were under continuous inpatient rehabilitation treatment after injury. One of the remaining patients was a homeschooled student, and the other was a homebound disabled individual without social activities. According to the NLI, the average expected K-SCIM [16] was 67.0±4.0, and the average initial K-SCIM was 49.3±6.9 points (Table 3).
Effect of the hospital-based TRP
As a result of nonparametric tests conducted on E1, E2, and E3, statistically significant results were shown in K-SCIM, Seoul-IADL, COPM, RIC-FAS, K-WHOQOL-BREF, K-CIQ, and GAS. However, there were no statistically significant post-hoc differences for E1 and E2, E2 and E3, and E1 and E3 (Table 4). After the end of the program, subject 1 and subject 5 were discharged from the hospital for the first time after injury and successfully returned to society, subject 2 started social activities, and subject #3 was able to resume school attendance and stopped homeschooling. The average duration of hospital-based TRP for the four subjects was 21.8±3.9 days (16.5±2.4 days excluding weekends), the total average cost for the hospital- based TRP was 7,494,502±1,729,204 Korean won, and the average cost strictly for the hospital-based TRP was 2,446,647±352,666 Korean won. The average wage of the researcher employed for this study who served as a program assistant was 1,608,257±232,025 Korean won per hospital-based TRP (Table 5).
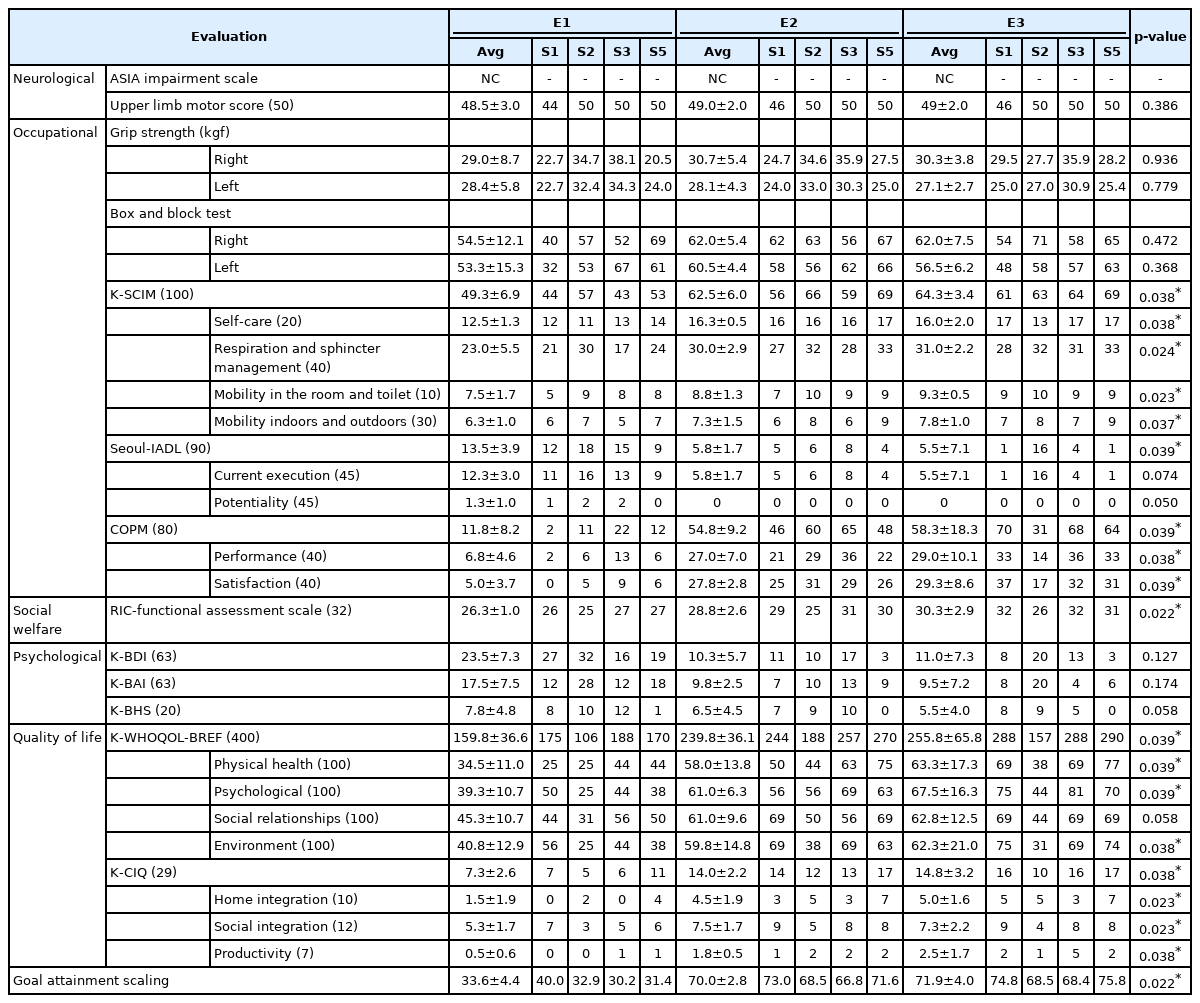
Results of the Korean version of the hospital-based transitional rehabilitation program for spinal cord injury patients using the daily living home
DISCUSSION
This study was conducted to develop the Korean version of the hospital-based TRP using DLH and to evaluate its effectiveness for SCI patients’ successful discharge and smooth return to society. TRP, as an intermediate link between rehabilitation treatment in the hospital and life after discharge, was developed with the goal of buffering the secondary trauma experienced after discharge by experiencing the home and social environment that would have changed after SCI by maximizing functional ability and minimizing trial and error. Therefore, the big difference from conventional rehabilitation treatment is hard training for self-care (independent clean intermittent catheterization [CIC] technique, bathing, etc.), safe performance of indoor activities (cooking, washing, etc.) and outdoor activities (shopping, participating in para-sports, visiting homes of peer disabled persons, creating hobbies, using public transportation, etc.) with supervision and assistance by medical staff and ILCs.
Hospital-based TRP was developed through current status surveys of domestic and overseas institutions and FG meetings, following which improvement proposals were developed through feedback obtained from pilot applications, FG meetings, and Delphi surveys. Hospitalbased TRP, with an average duration of 21.8 days (16.5 days excluding weekends), was applied to four chronic SCI patients with an average injury duration of 736.8 days. As a result, K-SCIM, Seoul-IADL, COPM, RIC-FAS, K-WHOQOL-BREF, K-CIQ, and GAS showed statistically significant improvement. In particular, although subjects 1 and 5 had been receiving continuous inpatient rehabilitation after their injury for more than 2 years before the hospital-based TRP was implemented, they satisfied 72.1% (44/61) and 76.8% (53/69) of expected K-SCIM, respectively. Eventually, both achieved 100% of the expectation, and the achievement rate for the core goals evaluated through GAS also showed very high results. The average cost per subject was 7,494,502 Korean won, and the average cost of the strictly hospital-based-TRP was 2,446,647 Korean won.
Although there have been theoretical considerations for establishing the Korean Transitional Rehabilitation System Model, the present study is the first to plan, implement, and evaluate its effectiveness clinically [17]. Although there have been cases in which the TRP was conducted at non-medical sites, including the KSCIA, the present study is the first to intensively carry out a hospital-based TRP within a short period [12,18,19]. In the future, when improving the medical rehabilitation system and determining the related medical fee, it is expected that the present study will be of high value.
Several common important points were found through the current status survey of overseas rehabilitation systems implemented in the process of developing the hospital-based TRP [7-11,14,15,20]. First, other countries have an integrated management system from acute treatment after injury to subacute rehabilitation and rehabilitation for a smooth return to society. In particular, it is important to actively engage patients with early mental interventions and peer support on a potential return to society when moving into an acute SCI ward or rehabilitation ward. Through this, it is possible to prevent the occurrence of learned lethargy in SCI patients. This can be considered one of the factors that can achieve successful early discharge within months after injury. In Korea, such an integrated system is not widely available after SCI, and patients and their caregivers have to go individually to rehabilitation hospitals, social rehabilitation procedures, community welfare institutions, and government agencies. It is expected that there are several cases of long-term hospitalization due to fear of returning home. Second, the rehabilitation system is operated by a multidisciplinary team, and third, peer support is important. There were several cases in which the peer disabled persons were members of medical institutions, and it is judged that presenting a visible role model to SCI patients increases the efficiency of preparing for discharge through the transfer of practical know-how and mental management by peer support. Fourth, there are professional personnel to support the rehabilitation of SCI patients; therefore, it is necessary to support a consistent rehabilitation process from the initial stage of SCI to follow-up management. In the UK, this role is played by are settlement officer or community coordinator, in the United States by a case manager, in New Zealand by an ILC, and in Sweden by a rehabilitation instructor. Typically, they are nurses, social workers, occupational therapists, or persons with SCI (people who have experienced a successful return to society after injury) and play a role as experts in supporting the return to society of SCI patients. Fifth, the local community care system for SCI patients is properly established. These points are very different from the current reality in Korea, and it seems to be why a rapid and safe return to society for SCI patients in Korea is not smoothly achieved.
As mentioned in the Introduction section, the hospital stay of SCI patients in Korea has been observed to be significantly extended, compared to that of SCI patients overseas [4-6]. In addition to medical factors, other cultural and social factors such as the completeness of community care and the payment system for medical expenses are considered to be complex. From a medical point of view, neurological recovery in general SCI patients is known to be within 2 months and, in 77% of cases, within 3 months after injury [21,22]. Depending on upper limb function, muscle strength has been reported to be rarely recovered until 2 years after injury [23]. In the present study, in subject 1, the upper limb motor score increased from 44 at the initial stage to 46 after TRP, with a certain improvement in the grip strength, which was not enough to change AIS. Therefore, the level of neurological recovery in most SCI patients is determined, in most cases, at 3 to 12 months. Therefore, if the serial neurological evaluation shows a saturation pattern, efforts should be made to educate the patient to use residual function to the extreme and change the surrounding environment, including the caregiver, to suit the patient. For this reason, it is reasonable to consider increasing the proportion of hospital-based TRP in inpatient rehabilitation treatment or completely converting to hospital-based TRP at a certain point in time.
Of course, based on the evidence that it can take up to 2 years after injury before muscle strength is restored, the National Health Insurance system in Korea allows neurodevelopmental treatment to be conducted twice a day during hospitalization, for up to 2 years after onset [23]. It is necessary to consider whether such a system may unnecessarily extend the length of hospital stay for the patient. The perception that patients can receive inpatient rehabilitation treatment for up to 2 years after injury onset is widespread among patients, and it is necessary to consider whether the discharge of SCI patients is delayed due to the formation of interest between consumers and suppliers of rehabilitation treatment. To solve this problem, it is necessary to refer to the Japanese convalescent hospital system. According to the information obtained by visiting the Kanagawa Rehabilitation Center in Japan, SCI patients are transferred from the acute stage hospital to the convalescent hospital within 2 months after SCI and receive rehabilitation treatment up to 5 months after injury. Rehabilitation treatment is partially supported by the National Health Insurance, and differential rates are applied to excellent institutions by evaluating the rate of return to the community, rate of long-term hospitalization, and characteristics such as severity and disease group. Based on the Japanese convalescent hospital system, an active rehabilitation system is in operation. Considering that the period is limited to 5 months after injury, rapid transfer from acute hospitals to convalescent hospitals is being achieved, and weekend rehabilitation treatment, home rehabilitation support, and advanced daily life training are thoroughly operated. In Korea, the “rehabilitation medical institution” pilot project kicked off in 2020. For SCI, the hospitalization period is set within 90 days after the onset/surgery, and the admission application period is 180 days. During this period, an integrated planning management fee (for patient management through multidisciplinary team meetings), an integrated rehabilitation functional evaluation fee (for periodic functional evaluation), and a fee per unit of treatment time are applied, and it is known that the fees are improved and newly established to support the patients’ smooth return to society [24]. When this “rehabilitation medical institution” system is officially established, it is believed that applying the hospital-based TRP developed in this study will help patients return to society quickly and stably. Not only professional rehabilitation treatment conducted by medical staff but also TRP, such as programs along with ILC and psychological supporting program, are needed for institutionalization and establishment of related fees.
TRP programs may be implemented in hospitals or nonmedical areas such as the KSCIA; it is thought to be best if the first TRP after injury is based in a hospital [12,18,19]. A representative example is urinary tract infection (UTI). In subjects 1 and 5 who participated in this study, they had never performed CIC independently, despite it being 730 days after injury. Self-CIC is very necessary for independent ADL. CIC training is conducted under the close guidance of a specialized nurse and ILC; however, if both subjects have a UTI, they have to proceed with concurrent TRP and antibiotic treatment. Moreover, if TRP is performed for subacute SCI patients, there is a possibility of medical or surgical problems. Therefore, it is believed that the initial TRP program should be conducted before discharge based on the hospital.
As indicated in Table 5, some costs were incurred in the TRP operation. The average cost per TRP of one subject was 7,494,502 Korean won, of which 32.6% was used for the pure TRP operation, and 21.5% was the wage of a researcher who was hired for this study and served as a program assistant, and 88.7% of the pure TRP operating costs were the service costs for ILC. The cost related to the activities of the case manager, such as in-depth interviews and goal-setting meetings, could not be set because there was no relevant fee. Although a certain cost is incurred for TRP operation, if the average length of hospital stay for domestic SCI patients can be reduced to 30.8 months within a year or 3–6 months with stable settlement, unnecessary national and individual medical expenses can be drastically reduced [4].
Looking deeper into the hospital-based TRP developed in this study, hospital-based DLH should be configured as similar to the home environment as possible so that daily life training, such as cooking, housekeeping, transfer education, and excessively advanced facilities, can be avoided to enable realistic training for the subject. In addition to the components of indoor facilities, it is necessary to form a network with outdoor facilities, such as courses that enable wheelchair technology promotion training, and facilities outside medical institutions, such as shopping and leisure experiences. An ILC, a peer SCI person who has achieved a successful return to society, is a member of the multidisciplinary team that plays an important role in TRP. Because they are not healthcare professionals from health authorities, if TRP becomes institutionalized in the future, verification processes may be needed for ILCs, which could be done through a regular curriculum and qualifications through the KSCIA. Additionally, for SCI patients, it is necessary to secure a number of ILCs because SCI patients’ functioning can be very diverse in consideration of sex and NLI. Additionally, under the current system, it is not possible to apply for an activity assistant supported by the authorities when admitted to a hospital. However, for the successful settlement of daily life after discharge, it is also worth considering that SCI patients and their activity assistants, to be assigned after discharge, need the time to adjust by allowing them to participate in the hospital-based TRP.
There exists no internationally accepted standard for the TRP duration; however, in Burwood Hospital in New Zealand, which operates a hostel, the admission period is designated as 1 month [11]. In the Australian TRP, which is conducted at the subject’s home, the program is operated for a flexible period of 2–8 weeks; however, direct comparison is difficult because most of the daily life training is sufficiently performed in the SCI ward before discharge [10,25]. A 2016 study indicated that a lower initial daily living ability evaluation score is associated with a longer program period. Moreover, the degree of satisfaction at the end of the program was proportional to program duration. However, there was no significant relationship between performance improvement and program duration [26]. Considering economic feasibility, excessively long program periods should be avoided. Based on 4 weeks, the operation may be adjusted to 2–4 weeks for paraplegia and 3–5 weeks for tetraplegia.
Study limitations
The present study has some limitations. First, this study was applied to a small number of subjects in a single institution. As suggested in this study, a considerable cost is incurred for TRP operation per patient, and large-scale research has limitations of research funding. In the future, further studies conducted in multiple institutions and involving several subjects are necessary to verify the effectiveness and stability of the hospital-based TRP.
In this study, the TRP was developed for spinal cord-impaired patients with lower cervical and thoracic SCI and relatively preserved upper limb function. It is necessary to develop a program for patients with upper cervical SCI through additional studies.
Furthermore, it was confirmed that the subjects maintained their functional improvement and return-to-society status (deinstitutionalization, participation in social activities, and return to school) 1 month after completion; however, long-term monitoring was not conducted because of the limited study period. In Australia, the Spinal Outreach Team systematically monitors those who participated in the social rehabilitation program for up to 12 months and provides early intervention and advice [10]. In New Zealand, outreach nurses visit and continuously monitor patients through phone calls after TRP, and at the end of 6 months, the patients are re-hospitalized for 3 days, and physical, occupational, social welfare, and psychological evaluation, including neurological and urodynamic tests, are performed. In the future, through additional research, it is necessary to formulate a follow-up management plan after hospital-based TRP.
In conclusion, the Korean version of the hospital-based TRP, applied to chronic SCI patients, it was thought that there is a possibility of improving the patients’ functioning and QOL, and appeared to be effective in successful discharge and social participation. Through this, it is considered that the inclusion of hospital-based TRP is necessary in the future when constructing a comprehensive rehabilitation system from SCI to return to society.
Notes
No potential conflict of interest relevant to this article was reported.
Conceptualization: Cho KH, Moon CW; Methodology: Cho KH, Moon CW, Jung IY; Software: Moon CW; Validation: Cho KH, Moon CW; Formal analysis: Cho KH, Moon CW, Jung IY; Investigation: Moon CW, Kim JY, Jang HN; Data curation: Moon CW, Kim JY, Jang HN; Original draft preparation: Moon CW, Kim JY, Jang HN; Review & editing: Cho KH, Moon CW, Jung IY.
Acknowledgements
This study was supported by the Rehabilitation Research & Development Support Program (No. NRC RSP2019004), National Rehabilitation Center, Ministry of Health and Welfare, Korea.
We would like to express our gratitude to Yong-koo Kim, Sora Kim, and Yong Deuck Yoo, who participated in the hospital-based TRP as ILCs.