- Search
| Ann Rehabil Med > Volume 44(2); 2020 > Article |
|
Abstract
Objective
To characterize the patients in the inpatient rehabilitation facility who were transferred to acute care facilities and identify the frequency of and reasons for the unplanned transfer.
Methods
Medical records of patients admitted to the inpatient rehabilitation facility from October 2017 to December 2018 were reviewed. Patients were categorized according to their diagnoses. The included patients were divided into the unplanned transfer and control groups based on whether they required to transfer to another department for acute care before completing an uninterrupted rehabilitation course. The groups were compared in terms of sex, age, length of stay, admission sources, and disease groups. The reasons for unplanned transfers were classified based on medical or surgical conditions.
Results
Of the 1,378 patients were admitted to the inpatient rehabilitation facility, 1,301 satisfied inclusion criteria. Among them, 121 (9.3%) were unexpectedly transferred to the medical or surgical department. The unplanned transfer group had a higher age (69.54±12.53 vs. 64.39±15.32 years; p=0.001) and longer length of stay (85.69±66.08 vs. 37.81±31.13 days; p<0.001) than the control group. The top 3 reasons for unplanned transfers were infectious disease, cardiopulmonary disease, and orthopedic problem.
Conclusion
The unplanned transfer group had a significantly higher age and longer length of stay. The most common reason for the unplanned transfer was infectious disease. However, the proportions of those with orthopedic and neurological problems were relatively high. Therefore, further studies of these patient populations may help organize systematic strategies that are needed to reduce unplanned transfers to acute facilities for patients in rehabilitation facilities.
Rehabilitation medicine is a field of medicine that concerned with improving the patient’s physical, psychological, social, and vocational function through the diagnosis and treatment of physical and/or cognitive impairments and disabilities that result from musculoskeletal conditions, neurological conditions, or other medical conditions. It is also related to reducing impairments, and preventing or treating complications [1,2]. Rehabilitation management can minimize the patient’s disability, maximize their independence, and increase their participation in life situations. In recent years, the development of medicine has increased the survival rate in diseases that were difficult to treat in the past and the importance of early rehabilitation is emerging [3]. However, early rehabilitation intervention can cause unexpected medical problems during inpatient rehabilitation. In prior reports, some patients admitted to rehabilitation facilities were found to be at risk for unplanned transfer to acute care facilities; subsequently, they could not receive timely rehabilitation treatment. These complications can significantly increase the individual medical costs and socio-economic burden, increase the morbidity and mortality associated with increased length of stay, and reduce the access to hospitalization for other patients [4-7]. It can have a negative impact on patients, families, and medical staff and result in inefficient use of resources during rehabilitation. In such cases, specific medical or surgical complications can result in transfer to acute care facilities [7-9]. Therefore, it is important to know how many unplanned transfers actually happen.
In a previous study, the incidences of unexpected complications in the hospital were reported. Among them, infections and organ injuries were the main reasons [10]. In particular, there were reports of unplanned transfer from inpatient rehabilitation facilities in other countries [11-13]. However, to the best of our knowledge, no such studies have been reported in Korea. Other studies have focused on patients with specific disease categories at rehabilitation facilities [7,14,15]. The objective of this study was to characterize the patients in the inpatient rehabilitation facility of a tertiary hospital who were transferred to acute care facilities and identify the frequency of and reasons for such unplanned transfers.
Medical records were collected retrospectively from electronic medical records of the rehabilitation facility from October 2017 to December 2018. The inclusion criteria were as follows: all patients older than 19 years admitted to the inpatient rehabilitation facility. Patients with planned transfers for scheduled management were not included in the analysis. Then, the patients of the rehabilitation facility were categorized as per their diagnoses: stroke, spinal cord injury (SCI), traumatic brain injury (TBI), musculoskeletal and neuromuscular diseases, cancer, and cardiopulmonary diseases. Data were collected on age, sex, admission sources, diagnostic information, length of stay from admission to discharge and reason for the transfer. This study received approval from the Institutional Review Board of Chungnam National University Hospital (No. 2019-03-097). The informed consent was waived.
The included patients were divided into the unplanned transfer group and control group based on whether they required to transfer to another department for acute care before completing an uninterrupted rehabilitation course. An unplanned transfer was defined as an episode of unexpected clinical deterioration in a rehabilitation facility patient that necessitated transfer to the acute care unit. The control group included patients who completed scheduled rehabilitation management and had no transfer to acute care facilities. The unplanned transfer group was compared with the control group in terms of sex, age, length of stay, admissions to inpatient rehabilitation based on internal or external referrals, and admission disease groups. The reasons for unplanned transfers were classified based on medical or surgical conditions. Medical conditions included cardiopulmonary, infectious, gastrointestinal, renal, hemato-oncological and neurological diseases. Surgical conditions included orthopedic, neurosurgical, plastic surgical, and general surgical problems.
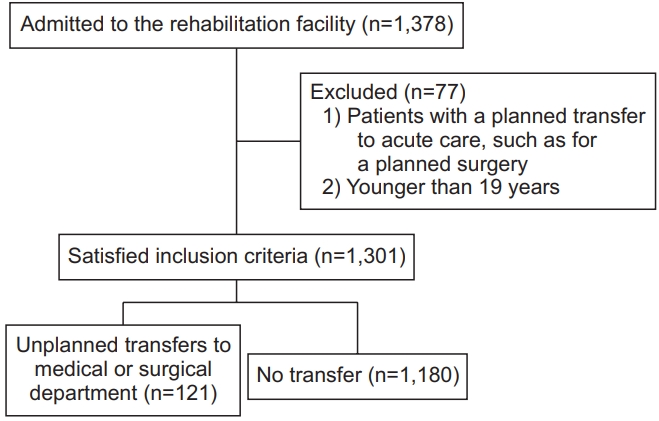
During the 15-month period of the study, 1,378 patients were admitted to the rehabilitation facility. Seventy-seven of them were excluded due to planned transfers or being under 19 years of age. Therefore, 1,301 patients were included in this study. Among participants, the proportions of those with stroke, musculoskeletal disease, SCI, TBI, neuromuscular disease, cancer, and cardiopulmonary disease were 46%, 22%, 13%, 7%, 6%, 3%, and 3%, respectively. In total, 121 (9.3%) were unexpectedly transferred to the medical or surgical department (Fig. 1).
The descriptive statistics by patient groups are shown in Table 1. One hundred twenty-one patients in the unplanned transfer group were significantly older (69.54±12.53 vs. 64.39±15.32 years; p=0.001), and their length of stay was significantly longer (85.69±66.08 vs. 37.81±31.13 days; p<0.001) than that of the control group. No significant difference in unplanned transfer rate was found by sex (male vs. female, 10.08% vs. 8.29%; p=0.27) or admission source (inside vs. outside hospital, 10.29% vs. 8.63%; p=0.31).
There were various medical or surgical reasons for unplanned transfers to the rehabilitation facility, including medical (cardiopulmonary, infectious, gastrointestinal, renal, hemato-oncologic, and neurological) or surgical (orthopedic, neurosurgical, plastic surgical, and general surgical) complications. The reasons that triggered the unplanned transfers are listed in Table 2. The proportions of medical and surgical reasons were 61.1% and 38.9%, respectively. Among the medical reasons, infectious disease (25.6%) was the most common, followed by cardiopulmonary (21.5%), neurological (6.6%), renal (4.1%) and hemato-oncological (3.3%) diseases. On the other hand, among surgical reasons, orthopedic problem (14.9%) was the most common, followed by neurosurgical (11.6%), plastic surgical (9.1%), and general surgical (3.3%) problems. For all reasons, the top 3 medical or surgical reasons for unplanned transfers were infectious disease (25.6%), cardiopulmonary disease (21.5%), and orthopedic problems (14.9%).
In this study, the rate of unplanned transfers was 9.3%. Several studies have reported the rates of unplanned transfers among patients admitted to rehabilitation facilities. Faulk et al. [12] demonstrated that 10.9% of patients admitted to rehabilitation facilities were transferred to acute care facilities. Carney et al. [11] reported 8.1% unplanned transfers to acute care facilities. Our findings were comparable to these results. We found a statistically significant difference in age and length of stay of the unplanned transfer group between the groups. No statistically significant differences were found relating to sex and admission source. Faulk et al. [12] reported no difference in age between the acute transfer and control groups. However, Leape et al. [16] reported an increased rate of adverse events in elderly individuals, and that many factors may account for such increased rates; for example, more complicated diseases, underlying degenerative conditions, and presence of comorbid conditions. These factors may also contribute to the differences from our results. When determining the length of stay, we investigated the time from admission to discharge. The length of stay in the unplanned transfer group was significantly longer than that in the control group, which is consistent with the findings of other studies [6,17]. The longer length of stay causes increased medical costs and reduced resource utilization in rehabilitation facilities [18-20].
In the current rehabilitation facility studied, infectious and cardiopulmonary diseases were the two most common reasons for unplanned transfers. These results are similar to those of a previous report [11]. In clinical practice, the criteria for the classification of complications are ambiguous and many cases are accompanied simultaneously by various reasons. For example, pneumonia is a disease that belongs to both infectious and cardiopulmonary diseases categories, but it is usually classified as an infectious disease. Hence, it was intentionally classified into infectious diseases. In a previous study, urinary tract infection (UTI) was the most common nosocomial infection in the general hospital [21]. However, in this study, among infectious diseases, pneumonia accounted for the largest portion. UTI was not the most common reason for unplanned transfer among those with infectious diseases. This difference may be related to the initial quick response to UTI that was carried out before proceeding with the onset of septic conditions, which would reduce unplanned transfer. The second most common reason for unplanned transfer, cardiopulmonary diseases, were estimated to be high in proportion because patients were older and had cardiac and pulmonary problems as underlying diseases [22].
Orthopedic problems were the third most common complications. Patients admitted to the rehabilitation facilities were usually hospitalized due to problems with movement; in the case of those with central nervous system (CNS) problems, they had restrictions on movement due to paraplegia, hemiplegia, or quadriplegia. Therefore, the risk of orthopedic problems seems to have increased due to characteristics of rehabilitation facilities that require frequent movements between the physical therapy room and the rehabilitation wards, which induces active physical movement. Additionally, it is likely that osteopenia or osteoporosis may have developed or worsened if the patient was older or had not been able to move voluntarily for a long period before and after surgery or pain [23,24].
In general wards, the rate of neurological and neurosurgical complications is not high [10,25]. However, in the rehabilitation facility of the current study, neurological and neurosurgical complications accounted for relatively large proportions (6.6%, 11.6%) of reasons for unplanned transfers. This could be attributed to the relatively early application of rehabilitation treatment in the tertiary hospital after CNS problems such as stroke, SCI, and TBI. Moreover, it may be a characteristic finding in rehabilitation facilities in Korea, where rehabilitation for CNS problems accounts for a large part of rehabilitation medicine in Korea due to its medical reimbursement system.
This study had several limitations. First, our investigation was limited because we only conducted the study for 15 months in a single tertiary rehabilitation center. Hence, the sample sizes of some disease groups were relatively small, and there was a big difference in sample size between the two groups. Therefore, there is a limit to the extent these results can be generalized. Based on these facts, future studies would need to conduct the long-term, disease-specific, multi-center studies. Second, we could not analyze the factors associated with unplanned transfers. Factors such as functional score, polypharmacy, comorbidity at admission, and presence of an indwelling catheter (e.g., central catheter, feeding tube, or Foley catheter) may be associated with unplanned transfers, but they were not explored in this study because there was missing data in some instances and no unified functional measures between different disease categories. Future studies should examine whether there are correlations between various factors and unplanned transfers. However, to our knowledge, this is the first study about unplanned transfers in a rehabilitation facility in Korea. Although some previous studies have investigated this concept in a similar method, they focused on specific disease groups within inpatient rehabilitation facilities [7,14,15]. However, our study is unique in its investigation of a large number of patients with entire disease groups admitted to the rehabilitation facility.
We investigated the frequency of and reasons for unplanned transfers from are habilitation facility in a tertiary hospital. The unplanned transfer group had a significantly higher age and longer length of stay than the control group. The most common reason for unplanned transfers was an infectious disease. However, the proportion of orthopedic and neurological problems as underlying reasons was relatively high. Therefore, further studies of these patient populations may help organize systematic strategies are needed to reduce unplanned transfers to acute facilities for patients in rehabilitation facilities.
AUTHOR CONTRIBUTION
Conceptualization: Im SB, Sohn MK, Kim YW. Methodology: Im SB, Sohn MK, Kim YW. Formal analysis: Im SB, Lim DY, Kim YW. Project administration: Im SB, Lim DY. Visualization: Im SB, Lim DY, Kim YW. Writing – original draft: Im SB, Kim YW. Writing – review and editing: Sohn MK, Kim YW. Approval of final manuscript: all authors.
Table 1.
Descriptive statistics by patient group
| Unplanned transfer (n=121) | Control (n=1,180) | p-value | |
|---|---|---|---|
| Continuous variablea) | |||
| Age (yr) | 69.54±12.53 | 64.39±15.32 | 0.001* |
| Length of stay (day) | 85.69±66.08 | 37.81±31.13 | <0.001* |
| Categorical variableb) | |||
| Gender | |||
| Male | 74 (61.16) | 660 (55.93) | 0.27 |
| Female | 47 (38.84) | 520 (44.07) | |
| Admission sources | |||
| Inside hospital | 54 (44.63) | 471 (39.92) | 0.31 |
| Outside hospital | 67 (55.37) | 709 (60.08) | |
| Disease group | |||
| Stroke | 43 (35.54) | 557 (47.20) | |
| SCI | 26 (21.49) | 144 (12.20) | |
| TBI | 8 (6.61) | 85 (7.20) | |
| Musculoskeletal disease | 20 (16.53) | 268 (22.71) | |
| Neuromuscular disease | 7 (5.78) | 74 (6.27) | |
| Cancer | 8 (6.61) | 25 (2.12) | |
| Cardiopulmonary disease | 9 (7.44) | 27 (2.30) |
Table 2.
Reasons for unplanned transferred from the rehabilitation facility
REFERENCES
1. Stucki G, Reinhardt JD, Grimby G. Organizing human functioning and rehabilitation research into distinct scientific fields. Part II: Conceptual descriptions and domains for research. J Rehabil Med 2007;39:299-307.


2. Gutenbrunner C, Ward AB, Chamberlain MA. White book on physical and rehabilitation medicine in Europe. Eura Medicophys 2006;42:295-332.
3. Johnston MV, Wood KD, Fiedler R. Characteristics of effective and efficient rehabilitation programs. Arch Phys Med Rehabil 2003;84:410-8.


4. Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Muller MK, Hahnloser D, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 2011;254:907-13.


5. White AC, Joseph B, Perrotta BA, Grandfield J, Muraldihar N, O’Connor HH, et al. Unplanned transfers following admission to a long-term acute care hospital: a quality issue. Chron Respir Dis 2011;8:245-52.


6. Tator CH, Duncan EG, Edmonds VE, Lapczak LI, Andrews DF. Complications and costs of management of acute spinal cord injury. Paraplegia 1993;31:700-14.



7. Civelek GM, Atalay A, Turhan N. Medical complications experienced by first-time ischemic stroke patients during inpatient, tertiary level stroke rehabilitation. J Phys Ther Sci 2016;28:382-91.



8. Pinto SM, Galang G. Venous thromboembolism as predictor of acute care hospital transfer and inpatient rehabilitation length of stay. Am J Phys Med Rehabil 2017;96:367-73.


9. Formisano R, Azicnuda E, Sefid MK, Zampolini M, Scarponi F, Avesani R. Early rehabilitation: benefits in patients with severe acquired brain injury. Neurol Sci 2017;38:181-4.


10. Soop M, Fryksmark U, Koster M, Haglund B. The incidence of adverse events in Swedish hospitals: a retrospective medical record review study. Int J Qual Health Care 2009;21:285-91.




11. Carney ML, Ullrich P, Esselman P. Early unplanned transfers from inpatient rehabilitation. Am J Phys Med Rehabil 2006;85:453-60.


12. Faulk CE, Cooper NR, Staneata JA, Bunch MP, Galang E, Fang X, et al. Rate of return to acute care hospital based on day and time of rehabilitation admission. PM R 2013;5:757-62.


13. Siegler EL, Stineman MG, Maislin G. Development of complications during rehabilitation. Arch Intern Med 1994;154:2185-90.


14. Hammond FM, Horn SD, Smout RJ, Beaulieu CL, Barrett RS, Ryser DK, et al. Readmission to an acute care hospital during inpatient rehabilitation for traumatic brain injury. Arch Phys Med Rehabil 2015;96(8 Suppl): S293-303. e1.



15. Alam E, Wilson RD, Vargo MM. Inpatient cancer rehabilitation: a retrospective comparison of transfer back to acute care between patients with neoplasm and other rehabilitation patients. Arch Phys Med Rehabil 2008;89:1284-9.


16. Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med 1991;324:377-84.


17. Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP. In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke 2011;42:3214-8.


18. Holloway RG, Witter DM Jr, Lawton KB, Lipscomb J, Samsa G. Inpatient costs of specific cerebrovascular events at five academic medical centers. Neurology 1996;46:854-60.

19. Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. Acute stroke care and rehabilitation: an analysis of the direct cost and its clinical and social determinants. Stroke 1997;28:1138-41.


20. Mamoli A, Censori B, Casto L, Sileo C, Cesana B, Camerlingo M. An analysis of the costs of ischemic stroke in an Italian stroke unit. Neurology 1999;53:112-6.


21. Kim JM, Park ES, Jeong JS, Kim KM, Kim JM, Oh HS, et al. Multicenter surveillance study for nosocomial infections in major hospitals in Korea. Am J Infect Control 2000;28:454-8.


22. Divo MJ, Martinez CH, Mannino DM. Ageing and the epidemiology of multimorbidity. Eur Respir J 2014;44:1055-68.



23. Be’ery-Lipperman M, Gefen A. Contribution of muscular weakness to osteoporosis: computational and animal models. Clin Biomech (Bristol, Avon) 2005;20:984-97.


- TOOLS
-
METRICS

- Related articles in ARM
-
The Discharge Destination of Rehabilitation Inpatients in a Tertiary Hospital.2005 February;29(1)