Functional Outcomes After Critical Pathway for Inpatient Rehabilitation of Total Knee Arthroplasty
Article information
Abstract
Objective
To investigate functional outcomes after the application of a critical pathway for inpatient rehabilitation of total knee arthroplasty (TKA).
Methods
A total of 184 patients (57 males and 127 females; average age, 71.5±5.9 years) who underwent unilateral or bilateral TKA were included. The critical pathway included early, intensive individualized rehabilitation exercises. Patients completed the following performance-based physical function tests: the stair climbing test (SCT), 6-minute walk test (6MWT), and Timed Up and Go test (TUG) as well as measurement of isometric knee flexor and extensor strength of the operated knee, gait speed, and range of knee flexion and extension. Self-reported physical function and pain were measured using the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) and visual analog scale (VAS), respectively, and self-reported quality of life was measured using the EuroQoL 5 dimension (EQ-5D) questionnaire. These evaluations were performed preoperatively and at 1 month and 3 months postoperatively.
Results
Performance-based and self-reported physical function and quality of life measures improved nonlinearly over time. Specifically, the 6WMT, TUG, gait speed, WOMAC-pain, WOMAC-function, VAS, and EQ-5D scores showed a significant improvement at 1-month post-TKA, whereas SCT, peak torque of the knee extensors and flexors, and WOMAC-stiffness scores showed gradual, but substantial, improvements over 3 months. There were between-group differences (unilateral and bilateral TKA groups) in the time course of the SCT, 6MWT, TUG, VAS, WOAMC-stiffness, and WOMAC-function results.
Conclusion
Patients who underwent critical pathway rehabilitation after TKA showed significant improvements in functional measurements during the first 3 months post-surgery.
INTRODUCTION
Knee osteoarthritis (OA) is one of the most common joint disorders and a leading cause of joint pain, swelling, functional limitation, and poor quality of life in the elderly [1]. Total knee arthroplasty (TKA) is the standard treatment for severe knee osteoarthritis, with demonstrable benefits in terms of improving pain, activity, and quality of life [2-4]. An increasing number of patients undergo TKA each year, therefore, it is important to identify appropriate rehabilitation programs after surgery; indeed, physical rehabilitation programs are widely advocated and are provided routinely.
TKA reduces pain and improves quality of life; studies have shown that fast-track surgery and an enhanced postoperative recovery program improve the initial postoperative physical performance, reduce the length of hospital stay from 4 to 2 days after surgery, and make readmission less likely [5-7]. However, quadriceps muscle strength is 41% weaker, walking distance is 28% lower, stair-climbing speed is 105% slower, and active knee flexion and extension are reduced after TKA, despite patients undergoing standard rehabilitation protocols [8,9]. Moreover, a randomized controlled trial of 165 TKA patients showed no difference in terms of mobility between a home-based only group and a 10-day admission rehabilitation service group at the 26th week assessment [10]. In addition, there was a critical pathway for rehabilitation after hip fracture surgery in South Korea [11] but lack of that for postTKA rehabilitation. Most studies included outpatients or inpatients for a short-term period (3–4 days) after TKA, had inadequate accurate and detailed rehabilitation protocols, and did not report varied evaluation outcomes [12-16]. Therefore, more effective post-TKA rehabilitation protocols are needed. At present, there is no critical pathway for intensive rehabilitation during the early post-TKA period in South Korea. Therefore, the aim of this study was to evaluate short-term functional outcomes after intensive critical pathway rehabilitation of inpatients after TKA.
MATERIALS AND METHODS
Participants
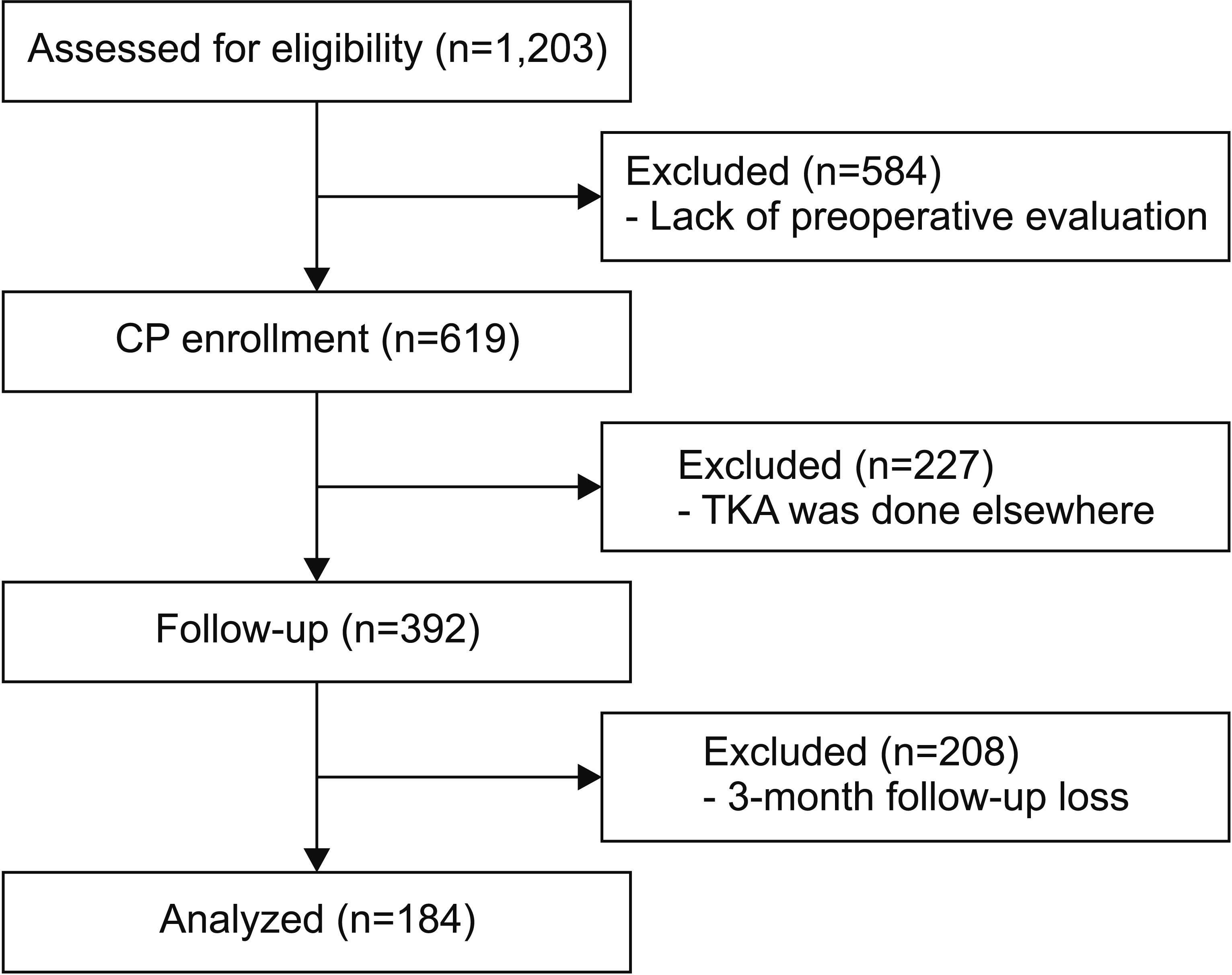
This retrospective cohort study included 184 patients (158 females and 26 males; average age, 71.5±5.9 years) who were diagnosed with end-stage primary knee OA. A total of 1,203 patients diagnosed with end-stage primary knee OA were recruited. We excluded 584 patients who were not evaluated preoperatively. Further inclusion criteria were as follows: (1) be scheduled for a first TKA, (2) hospitalized between October 2013 and April 2018, and (3) could walk independently with or without an ambulatory aid. A total of 227 patients were excluded as they underwent TKA surgery at another hospital, as were 208 patients who did not complete the 3-month follow-up. Finally, 184 patients were enrolled in the study (Fig. 1). The study protocol was approved by the local ethics committee of Jeju National University Hospital (No. 2019-01- 015). Written informed consents were obtained.
The critical pathway
When the need for an operation was confirmed, the orthopedic surgery department referred the patient to the rehabilitation department for preoperative consultation and evaluation, which included performancebased physical function tests and self-reported physical function questionnaires. If vital signs were stable after TKA, the patient was started on an early rehabilitation protocol, which comprised range of motion (ROM) exercises using a continuous passive motion device and progressive resistance exercises (incline leg press, leg press, leg extension, leg curl, hip abduction, and hip adduction) using air resistance machines (HUR Co., Kokkola, Finland) (Fig. 2). The 1 repetition maximum (1RM) for each patient was measured. Resistance loads began at 10%–20% of the 1RM (3 sets of 15 repetitions) from the 4th day post-surgery. Two weeks post-surgery, the patient was transferred to the rehabilitation department.

The progressive resistance exercises consisted of (A) incline leg press, (B) leg press, (C) leg extension, (D) leg curl, (E) hip abduction, and (F) hip adduction using air-resistance machines (HUR Co., Kokkola, Finland).
The intensive rehabilitation program included progressive gait training using a lower-body positive pressure treadmill (Alter-G Inc., Fremont, CA, USA) (Fig. 3), aerobic exercise using a stationary ergometer, and progressive resistance exercises. Progressive resistance exercises using the HUR increased gradually from 30% (3 sets of 15 repetitions) to 60% of 1RM; the number of repetitions decreased as the load increased.

The gait training exercises consisted of Alter G anti-gravity treadmill (Model M320; Alter G Inc., Fremont, CA, USA).
For progressive gait training, patients began with 50% bodyweight support (BWS) and walked at a speed of 2.0 km/hr; BWS was reduced gradually. When BWS was no longer needed, patients moved onto a land treadmill. They received stair training on the day of discharge. The G-trainer was used daily, whereas the ergometer and HUR machine were used on alternate days. The TKA rehabilitation programs were performed as follows: 30 minutes per session, 2 sessions per day, 5 days per week, for 2 weeks.
To enable self-exercises in the ward, the rehabilitation nurse instructed patients how to perform a range of joint motion and TheraBand exercises; patients were provided with an exercise brochure. Prior to discharge, patients were educated about self-exercise for home-based rehabilitation. Evaluations including performance-based physical function and self-reported physical function were performed 1 month and 3 months post-surgery (Fig. 4).
Outcome measures
Each examination was performed preoperatively, 1 month postoperatively, and 3 months postoperatively, giving sufficient rest time; all outcome measures were conducted on 1 day. In all patients, isometric strength of the knee extensors and flexors was measured by a physical therapist, and other tests, including the questionnaire, were performed by the education nurse at our arthritis center.
Performance-based physical function tests
Stair climbing test
The stair climbing test (SCT) was used to assess functional mobility and the ability of the lower extremity muscles to generate concentric and eccentric forces. For the test, the time taken to ascend and descend a flight of stairs (12 steps; each step was 17-cm high and 25-cm wide) was measured [17].
Six-minute walk test
The 6-minute walk test (6MWT), a measure of the distance (m) that an individual walks in 6 minutes, was used to assess the overall locomotor ability and locomotor fatigue. Patients were instructed to walk as far as possible for 6 minutes along a 50-m hallway that was marked with lines [18].
Timed Up and Go test
For the Timed Up and Go (TUG) test, patients began in a seated position in an armchair (seat height, 44 cm; depth, 45 cm; width, 49 cm; and armrest height, 64 cm). They were then instructed to rise, walk forward for 3 m, turn around, walk back to the chair, and sit back down without any physical assistance. The whole process was timed and evaluated the dynamic balance [19].
Isometric strength of the knee flexors and extensors
The maximal isometric strength of the bilateral knee extensors and flexors was measured using an isokinetic dynamometer (Computer Sports Medicine Inc., Stoughton, MA, USA). Before the test, all patients relaxed their muscles by performing light stretches [20]. Patients were instructed to grasp the sidebars of the apparatus during the test procedure. After a structured warm-up with the knee joint fixed at 60° of flexion (to generate maximal isometric force) [21], patients were instructed to perform maximal voluntary contractions until the torque did not increase by >5% on three successive attempts.
Gait speed
Spatiotemporal variables of gait were measured using a validated wireless inertial sensing device (BTS Bioengineering S.p.A., Milan, Italy). The first and last steps of the 8-m walk were removed from all calculations to eliminate the effects of abnormal patterns during the initiation of gait or psychological responses at the termination of gait [22].
Measurement of knee ROM
Available knee ROM was measured using a standard long arm goniometer. Knee flexion was measured as the value of maximal active bend at the knee while the patient was lying in a supine position. Knee extension was measured as the angle of maximal active straightening with the patient’s heel placed on a 10-cm wooden block [23].
Self-reported physical function, pain, and quality of life
The Western Ontario McMaster Universities Osteoarthritis Index
The multidimensional Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) questionnaire includes questions on pain, stiffness, and physical function. The questionnaire includes 5 pain, 2 stiffness, and 17 physical function variables. Each of these variables is scored on the Likert scale (0, none; 1, slight; 2, moderate; 3, very; and 4, extremely), which is used to measure outcomes in rheumatology clinical trials. Thus, the Likert scale determines the degree of pain, stiffness, and difficulty experienced when performing each of the 17 activities during the preceding 48 hours. Higher scores indicate greater levels of pain, stiffness, and difficulty [24].
Visual analog scale
Patients were instructed to evaluate their level of knee pain using visual analog scale (VAS), which was measured when the patient was resting. The scale consisted of a 10-cm long horizontal line that ranged from ‘no pain’ to ‘worst possible pain’. The VAS system ranged from 0 (no pain) to 10 (worst possible pain) points [25].
EuroQoL 5 dimension questionnaires
The EuroQoL 5 dimension (EQ-5D) questionnaire is used to evaluate self-reported quality of life. The EQ-5D index is used widely to measure general health status. The instrument comprises questionnaires with the following 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is represented by one question that has three severity levels, namely, no problems, some or moderate problems, and extreme problems [26].
Statistical analysis
All statistical analyses were performed using IBM Statistical Package for the Social Sciences software version 18.0 (IBM Co., Armonk, NY, USA). All variables were subjected to descriptive statistics. Repeated-measures ANOVA was performed to assess the effect of time on the postoperative outcomes of performance-based and selfreported physical function and on the quality of life. Posthoc analyses using Bonferroni test were performed to detect significant interactions between group and time. A p-value of <0.05 was considered significant.
RESULTS
Patient demographics and characteristics are presented in Table 1. There were 158 (85.9%) females and 26 (14.1%) males (average age, 71.5±5.9 years). The average body mass index was 26.1±3.1 kg/m2. Of the 184 patients, 127 (69%) underwent unilateral TKA and the remaining 57 (31%) underwent bilateral TKA.
Postoperative outcomes with respect to objective performance-based physical function, self-reported physical function, pain, and quality of life
Postoperative outcomes with respect to performancebased physical function, self-reported physical function, pain, and quality of life are presented in Table 2.
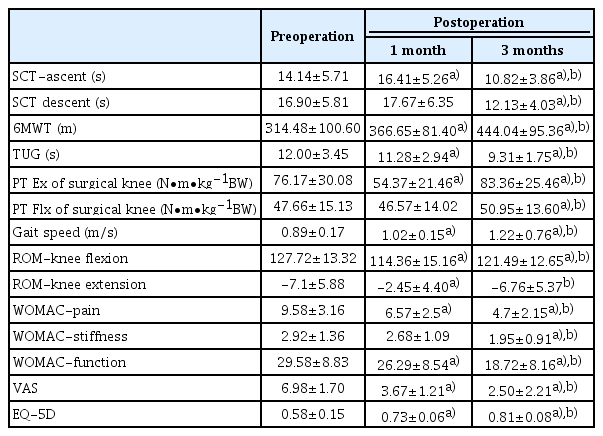
Postoperative outcomes of performance-based and self-reported physical function, pain and quality of life by repeated measure of ANOVA
The performance-based and self-reported physical function and quality of life measures improved nonlinearly over time. Specifically, the 6MWT (314.48±100.60 vs. 366.65±81.40 vs. 444.04±95.36 m; p<0.001), TUG test (12.00±3.45 vs. 11.28±2.94 vs. 9.31±1.75 seconds; p< 0.001), gait speed (0.89±0.17 vs. 1.02±0.15 vs. 1.22±0.76 m/s; p<0.001), WOMAC-pain (9.58±3.16 vs. 57±2.5 vs. 4.7±2.15; p<0.001),WOMAC-function (29.58±8.83 vs. 26.29±8.54 vs. 18.72±8.16; p<0.001), VAS (6.98±1.70 vs. 3.67±1.21 vs. 2.50±2.21; p<0.001), and EQ-5D (0.58±0.15 vs. 0.73±0.06 vs. 0.81±0.08; p<0.001) scores improved significantly between the preoperative, 1 month postoperative, and 3 months postoperative measurements, respectively. The SCT ascent (14.14±5.71 vs. 12.13±4.03 seconds; p<0.001), SCT descent (16.90±5.81 vs. 12.13±4.03 seconds; p<0.001), peak torque generated by operated knee extensors (76.17±30.08 vs. 83.36±25.46 N∙m∙kg-1BW; p<0.001), peak torque generated by surgical knee flexors (47.66±15.13 N∙m∙kg-1BW vs. 50.95±13.60 N∙m∙kg-1BW; p=0.002), and the WOMAC-stiffness score (2.92±1.36 vs. 1.95±0.91; p<0.001) improved significantly between the preoperative and 3-month postoperative measurements, respectively.
Postoperative outcomes of the unilateral and bilateral TKA groups with respect to objective performance-based physical function, self-reported physical function, pain, and quality of life
Differences in the postoperative physical function, pain, and quality of life outcomes between the groups are presented in Table 3. Time course of various functional measurements differed between the unilateral and bilateral TKA groups. At 1 month post-surgery, there were significant differences between the unilateral and bilateral TKA groups with respect to SCT ascent (15.52±4.79 vs. 18.34±5.76 seconds, respectively; p=0.001), SCT descent (16.37±5.09 vs. 17.50±6.06 seconds, respectively; p<0.001), TUG test (10.91±2.55 vs. 12.12±3.58 seconds, respectively; p=0.009), and VAS (3.52±1.28 vs. 4.04±0.97, respectively; p=0.004) scores. The unilateral TKA group showed significant improvement in the 6MWT (preoperative 428.82±97.54 vs. postoperative 474.91±84.10 m; p=0.001) at 3 months post-surgery. This group also showed a significant difference in the WOMAC-function score at 1 month (preoperative 25.22±8.66 vs. postoperative 28.39±7.98; p=0.024) and 3 months postoperatively (preoperative 17.65±8.39 vs. postoperative 20.82±7.39; p<0.001).
DISCUSSION
TKA is becoming more common; therefore, it is important to identify the most effective rehabilitation program to optimize patient care. According to several studies, critical pathways reduce the length of hospital stay without increasing clinical complications; also, patients seem more inclined to make use of rehabilitation services [27,28].
To the best of our knowledge, this study is the first to report on both physical and self-reported, short-term functional outcomes following the application of a critical pathway for early and inpatient TKA rehabilitation in Korea. Comparing other critical pathway programs, our critical pathway started on the 4 days of operation day, and patients were transferred to rehabilitation department at 2 weeks of operation day and trained for 2 weeks to achieve early intensive rehabilitation in terms of starting time and concentration. In addition, we have a strong advantage of using individualized and advanced equipment and evaluating the effects on various performance based physical function and self-reported physical function outcomes. The results showed significant improvement in a range of performance-based and self-reported physical functions, pain, and quality of life at 1 month and 3 months post-TKA.
Many studies have examined rehabilitation outcomes after TKA, and benefits and drawbacks have been reported. For example, Buhagiar et al. [10] conducted a randomized clinical trial of 165 unilateral TKA patients and compared an intensive inpatient rehabilitation group (which received physical therapy twice daily for 10 days) with a monitored home-based therapy group. Neither groups showed improved mobility at 26 weeks post-TKA. In contrast, our study recorded significant improvements in physical function (6MWT and EQ-5D scores) within a short period of time, although it is difficult to compare our study directly with that study, as that study was a randomized controlled trial. In addition, another study followed up 16 unilateral TKA patients who underwent early and highly intensive rehabilitation for a total of 25 visits over 12 weeks; patients showed positive results in terms of the SCT, TUG, and 6MWT scores at 3.5, 6.5, and 12 weeks post-TKA [7]. The rehabilitation program included both weight-bearing and non-weight-bearing exercises (such as quadriceps setting, straight leg raises, hip abduction, and hamstring curls with increasing resistance), as did our study. However, we report superior outcomes for TUG and 6MWT scores at 3 months post-surgery; the SCT scores were similar. In addition, we initiated early rehabilitation at 2 weeks post-TKA and a period of 2 weeks, with significant improvements.
Gait speed is a useful tool for measuring a patient’s physical function. A previous study reported 24 patients who underwent conventional rehabilitation after TKA; gait speed was slow until 3 months post-TKA, and at 6 months, it was similar to that recorded pre-TKA [29]. In contrast, our data show a linear improvement up to 3 months post-TKA. We believe that this finding is due to the intensive program based on the critical pathway in our study.
Various physical outcomes are used before and after discharge from hospital to assess functional recovery after TKA; however, they provide limited information. Thus, functional variables such as pain-VAS and WOMAC-function scores are effective tools for estimating pain and quality of life after TKA [30]. Consistent with our findings, Moffet et al. [31] demonstrated that subjects from an intensive functional rehabilitation group showed faster recovery and increased ability to perform daily activities with less pain, stiffness, and difficulty than conventional group following TKA. Furthermore, a study found that leg press power is more closely related to selfreported and performance-based outcomes than knee extensor strength [32]. In contrast, other studies report a more variable relationship between patient reported function and muscle strength [33,34].
In terms of postoperative quadriceps muscle strength, we found that our protocol had a marked effect. Judd et al. [29] reported the results of 24 patients who underwent conventional post-TKA rehabilitation; compared with the preoperative value, there was a 42% decrease in the peak toque generated by operated knee extensors at 1 month post-TKA and 34% decrease in that generated by the knee flexors. Muscle strength did not return to preoperative levels until 3 months post-TKA. In contrast, we found only a 29% and 3% decrease in the peak toque generated by the surgical knee extensors and flexors, respectively; we also found that quadriceps muscle strength was significantly better at 3 months post-TKA than at pre-TKA. Within the first month post-TKA, the knee extensors and flexors were at their weakest (compared with pre-, post-, and 1-year post-TKA) [35]. Such muscle weakness is predominantly due to the failure of spontaneous muscle activation, reduced ROM, and muscle atrophy [36]. This emphasizes the importance of rehabilitation strategies focusing on muscle strengthening during the early period after TKA; minimal reductions in early quadriceps muscle strength lead to improvements in several physical performance factors. Also, increased muscle strength has a positive effect on the SCT.
We found that the unilateral and bilateral TKA groups reported time differences with respect to functional measures, particularly in SCT, TUG, and VAS scores at 1 month, the 6MWT at 3 months, and WOMAC-function scores at 1 month and 3 months post-surgery. Several factors may be involved in these results, and presumably, the quadriceps strength of the non-surgical side and VAS score may affect performance. Iwata et al. reported that the VAS score and strength of quadriceps of the non-surgical side were significantly associated with gait speed and TUG test [37]. A study by Valtonen et al. [38] on 56 patients with end stage knee OA reported that muscle power of the extensor and flexor of the knee on the nonsurgical side was independently associated with SCT. However, in contrast to our results, Huang et al. [39]conducted a comparative analysis of the unilateral and bilateral groups at 6 months post-TKA and showed similar functional improvement in pain, stiffness, function, and total WOMAC scores without significant difference between the two groups. However, that study only evaluated WOMAC scores at 6 months postoperatively, and it cannot be directly compared with our study as we evaluated various performance-based and self-reported physical functions at 1- and 3 months post-TKA.
This study had some limitations. First, it was a retrospective cohort study with no control group; therefore, we could not compare our patients with those who did not receive early intensive rehabilitation. More research regarding the relationship between postoperative functional outcomes and the effects of our critical pathway program are required. Second, the study may suffer selection bias as only subjects followed up from pre-TKA to 3 months post-TKA were included. Therefore, longterm prospective comparative randomized control trial studies are needed. In conclusion, this study confirmed that patients who underwent early intensive rehabilitation within 2 weeks post-TKA via a critical care pathway showed significant improvements in various functional measures during the first 3 months post-TKA, although intergroup differences were observed in some functional outcome measures.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by the 2019 education, research and student guidance grant funded by Jeju National University.
Notes
Conceptualization: Kim BR, Kim JH. Methodology: Kim BR, Kim JH, Han EY, Lee SY. Formal analysis: Kim BR, Kim JH. Project administration: Kim BR, Kim JH, Han EY, Kim SR, Nam KW, Lee SY, Kim WB. Visualization: Kim BR, Kim JH, Han EY, Kim SR, Nam KW, Lee SY, Kim WB. Writing – original draft: Kim BR, Kim JH. Writing – review and editing: Kim BR, Kim JH. Approval of final manuscript: all authors.