Repetitive Transcranial Magnetic Stimulation Enhances Recovery in Central Cord Syndrome Patients
Article information
Abstract
Objective
To investigate the effect of repetitive transcranial magnetic stimulation (rTMS) on neurological and functional recovery in patients with central cord syndrome (CCS) involving the upper extremities between the treated and non-treated sides of the treated group and whether the outcomes are comparable to that of the untreated control group.
Methods
Nineteen CCS patients were treated with high-frequency (20 Hz) rTMS over the motor cortex for 5 days. The stimulation side was randomly selected, and all the subjects received conventional occupational therapy during the rTMS-treatment period. Twenty CCS patients who did not receive rTMS were considered as controls. Clinical assessments, including those by the International Standard for Neurological Classification of Spinal Cord Injury, the Jebsen-Taylor Hand Function Test, and the O'Connor Finger Dexterity Test were performed initially and followed up for 1 month after rTMS treatment or 5 weeks after initial assessments.
Results
The motor scores for upper extremities were increased and the number of improved cases was greater for the treated side in rTMS-treated patients than for the non-treated side in rTMS-treated patients or controls. The improved cases for writing time and score measured on the Jebsen-Taylor Hand Function Test were also significantly greater in number on the rTMS-treated side compared with the non-treated side and controls. There were no adverse effects during rTMS therapy or the follow-up period.
Conclusion
The results of the application of high-frequency rTMS treatment to CCS patients suggest that rTMS can enhance the motor recovery and functional fine motor task performance of the upper extremities in such individuals.
INTRODUCTION
Spinal cord injury (SCI) is a major devastating lesion and the treatments for the condition in the clinical setting remain controversial. A number of clinical trials aiming to achieve functional recovery in SCI patients have been carried out and most of the results relevant to the protection of the injured spinal cord and modulation of secondary injury following SCI were uncertain [1]. Recently, many studies have aimed to explore means of regenerating damaged neurons using various types of stem cells [2,3], regeneration-associated genes [4], biomaterials [5] or their combinations [6]. However, the reported treatment methods are invasive with effects limited for clinical application and many safety issues have not been considered in the existing studies. Another treatment strategy for post-SCI functional restoration is neuronal plasticity enhancement. Although neuronal plasticity after SCI is not as well studied or understood as that after brain lesion, some studies have reported collateral sprouting of spared axons to disconnected tracts and cortical remapping in incomplete SCI animal models [7,8]. In fact, in the case of extensive and proper plasticity of spared axons within the spinal cord, functional recovery could be expected [9,10].
Repetitive transcranial magnetic stimulation (rTMS) has been reported to modulate cortical and spinal cord circuits and neuronal plasticity [11] to the extent of enhancing neuronal plasticity, which in turn could promote functional improvements after SCI [12]. Recent clinical studies have revealed that rTMS can reduce neuropathic pain [13] and spasticity [14] in SCI patients; however, the reported effects are variable and limited [15].
Central cord syndrome (CCS) is the most common type of SCI with frequent occurrence in older patients with cervical spondylosis or hyperextension injury [16]. CCS is characterized by upper extremity weakness that is disproportionately greater than that in the lower extremities [17]. Globally, the frequency of incidence of CCS, one of the major age-related spinal disorders [18] is on a constant rise with an aging population. Although the prognosis of CCS patients is usually better compared to the patients with other types of incomplete SCI, complete recovery is rare, and in fact, most of the CCS patients suffer from neuropathic pain and upper extremity dysfunction for the rest of their lives.
In the present study, subsequent to prospective application of rTMS to CCS patients, we aimed to delineate its effect on neurological and functional recovery of the upper extremities between the treated and non-treated sides of a treated group and determined whether the effect is comparable with the untreated control group.
MATERIALS AND METHODS
Subjects
We performed a prospective clinical trial with subacute stage (9–83 days post-injury) CCS patients recruited from the inpatient population in Department of Rehabilitation Medicine at Dankook University Hospital. The diagnostic criterion for CCS was similar to that of Schneider et al. [19]: SCI patients with disproportionately more motor impairment of the upper than the lower extremities. Any subjects having the following conditions were excluded: pre-existing or combined brain lesions, combined peripheral nerve injuries or polyneuropathies, metal implants in the head, history of substance abuse, severe cognitive dysfunction, and personal or family history of seizure. Nineteen patients with CCS (mean age, 53 years; 15 males and 4 females) participated in this study, and 20 CCS patients who disagreed to receive rTMS treatment were included as a control (mean age, 55 years; 19 males and 1 female). The most common neurological level of injury (NLI) was C5 (36.8% in rTMS-treated patients and 40% in controls), and the severity of impairment in most of the subjects, according to the International Standards for the Neurological Classification of Spinal Cord Injury (ISNCSCI), was AIS (American Spinal Injury Association [ASIA] Impairment Scale) D (84.2% in rTMS-treated patients and 80% in controls) (Tables 1, 2). There was no difference in age or in the gender distribution, initial NLI, and initial AIS between rTMS-treated patients and controls. This study was approved by the Dankook University Hospital Institutional Review Board (No. 2013-04-015).
Treatments
All the subjects received high-frequency (20 Hz) rTMS over the unilateral motor cortex by means of a Magstim Super Rapid2 magnetic stimulator (Magstim, Carmarthenshire, UK) with a 70-mm diameter figure-of-eight coil. The side for rTMS treatment (to which the data analyzer was blind) was randomly determined and the treatment was performed once per day for 5 consecutive days. Stimulation of the left or right primary motor cortex (M1) induced a response in the contralateral abductor pollicis brevis muscle, which manifested as a muscle twitch that was recorded as a motor-evoked potential (MEP) using surface electromyography. We defined the ‘treated side’ as the contralateral side of the stimulated motor cortex; accordingly, when the left motor cortex was stimulated, the ‘treated side’ was considered as the right side. Twosecond bursts of 20 Hz were applied over the hand area of the assigned unilateral motor cortex at inter-train intervals of 28 seconds, for a total of 1,800 pulses during 30 minutes. The intensity of the stimulation was set to 90% of the resting motor threshold, which was defined as the lowest intensity necessary for the evocation of an MEP response of 50 μV in 50% of trials. Also, the subjects received conventional occupational therapies including strengthening exercises, training in the activities of daily living, and manual dexterity exercises for 30 minutes twice per day during their rTMS treatment.
Neurological assessment
All the subjects received physical examination along with the motor and sensory, NLI and AIS evaluations by ISNCSCI at admission and again at 4 weeks post-rTMS treatment. We scored the upper extremity motor and sensory statuses from C5 to T1 and the lower-extremity ones from L2 to S1. Also, hand strength was objectively evaluated using a hand dynamometer and pinch gauge to measure the grip strength and lateral and tip pinch strengths exerted by the thumb and index fingers in both the hands. Each test was performed three times, and the score was recorded as the average of three values [20]. For comparison of the treated and non-treated sides of rTMS treated patients, the motor, sensory, and muscle power of both the sides of the control patients were divided by half by adding the left and right measurements.
Functional assessment
The hand and finger functional assessments were determined using the Jebsen-Taylor hand function test (JHFT) and the O’Connor Finger Dexterity Test (OFDT; Lafayette Instrument Co., Lafayette, IN, USA) at admission and 4 weeks post-rTMS treatment. The JHFT provides quantitative measurements of standardized tasks in assessing the following 7 subsets of hand function: writing, turning over 3×5-inch cards, picking up small common objects, simulated feeding, stacking checkers, picking up large light objects, and picking up large heavy objects. The time to complete each subset was recorded and compared with the established normal value determined for age and sex. The OFDT is a standardized test used to evaluate rapid picking up and insertion of small pins into 100 holes arranged in 10 rows and spaced 1/2 inch apart. The subjects were instructed to insert 3 pins per hole using their left or right hand. Following the guidelines in the manual, the time required by the subject to insert 3 pins into the first 5 rows of the board (total 50 holes) was considered to be the first halftime, and the time required to insert another 3 pins into the other 5 rows (total 50 holes) was considered as the second halftime. The raw score was recorded as the average of the first and second half times multiplied by 1.1. The standard score and percentile rank were determined according to the raw score ranges specified in the manual (Lafayette Instrument Co.). For comparison of the treated and non-treated sides of the rTMS treated patients, the results for the control patients were expressed as the averages of the left and right measurements.
Statistical analysis
Statistical analyses were performed using PASW Statistics version 23 (IBM Corp, Armonk, NY, USA). The Shapiro-Wilk test was used to reveal the normal distribution of the quantitative data obtained from the neurological and functional assessments. One-way analysis of variance and Games-Howell post-hoc test were performed to compare all the numerical data at the baseline and during the follow-up period among the treated and nontreated sides of the rTMS-treated patients and controls, and Wilcoxon rank sum test was employed to compare neurological and functional data between the initial and follow-up periods in the same subjects. The likelihood ratio test was used to analyze the subjects who showed any improvements following rTMS treatment on the treated and non-treated sides and controls. Spearman rank correlation analysis was performed to find relationships between the duration from onset to rTMS treatment and neurological and functional changes. The p-values less than 0.05 were considered to be significant.
RESULTS
Following randomization of the treated side, 11 patients received rTMS treatment on their right hemisphere (treated side, left) and 8 patients received treatment on their left hemisphere (treated side, right). There were no differences in the changes in neurological and functional status between the left- and right-side-treated subjects. No adverse effect was found during or after rTMS treatment in any of the subjects.
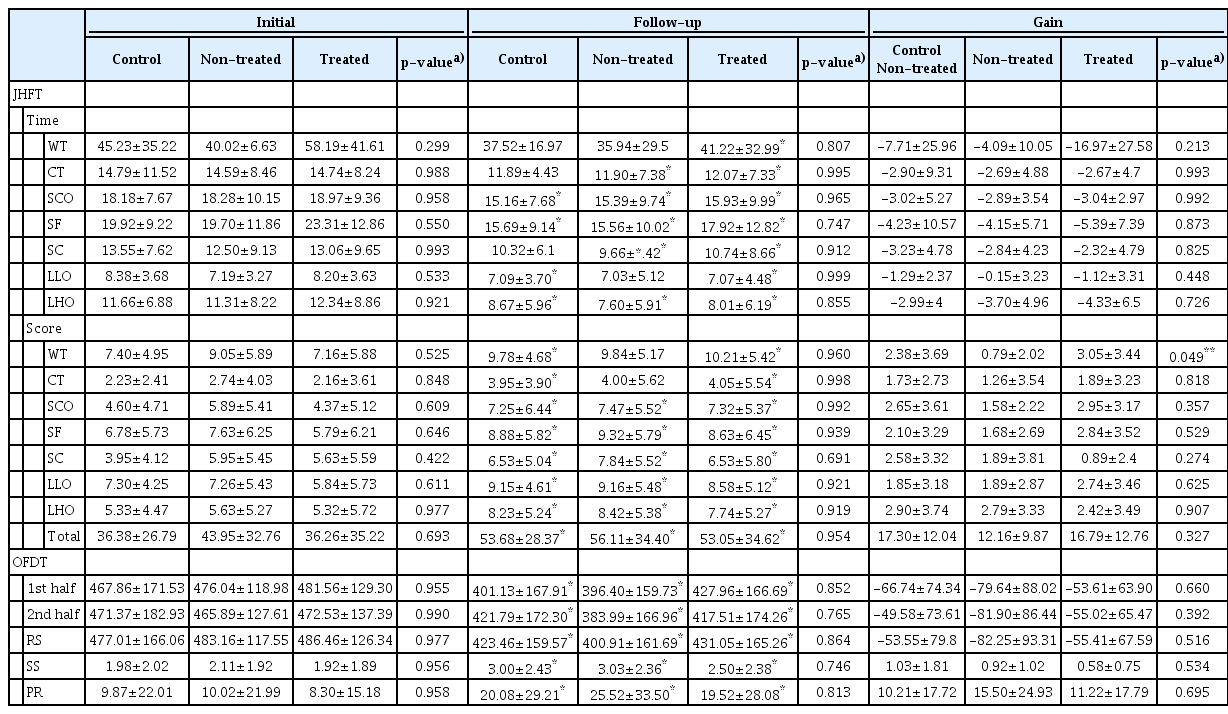
The upper extremity motor scores for rTMS-treated patients and controls were improved 4 weeks after rTMS treatment or 5 weeks after initial assessments, and notably, the gain score of both the sides of rTMS-treated patients exhibited more increase compared with the controls (gain score, 4.05±2.00 and 3.37±3.44 for both the sides of rTMS-treated patients vs. 1.85±2.71 for controls; p=0.049) (Table 3). In addition, when we counted the number of improved cases for each side of rTMS-treated patients and controls, there were more cases with the treated side than the non-treated side in rTMS-treated patients and controls (95%, 68%, and 65%, respectively; p=0.035) (Fig. 1A). Also, the grasp power and fingertip and lateral pinch powers were increased during the follow-up period, regardless of the side or rTMS treatment (Table 3). The sensory score of the upper extremities and the motor and sensory scores of the lower extremities exhibited no change on either side of rTMS-treated patients or controls during the follow-up period (Table 3).
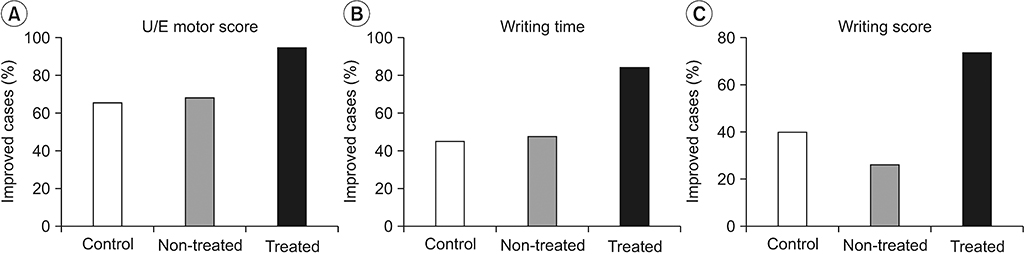
Featured neurological and functional changes in control and rTMS-treated patients: number of subjects with improvement (%) with respect to UE motor score (A), writing time (B) and score (C) by JHFT for controls or rTMS-treated patients of treated and non-treated sides during the follow-up period. All p-values were less than 0.05 by likelihood ratio test. rTMS, repetitive transcranial magnetic stimulation; UE, upper extremity; JHFT, Jebsen Hand Function Test.
The functional status measured by JHFT and OFDT exhibited improvement on the treated side in rTMS-treated cases and on the non-treated side in rTMS-treated patients. Neither the writing time score nor the card turning score measured by JHFT exhibited any change at 4 weeks after rTMS treatment, and time for writing, card turning, and picking up large heavy objects showed no improvement in controls (Table 4). When we compared the number of cases of improvement in writing time and score between the treated and non-treated sides in rTMS-treated patients and controls, more cases were observed on the treated side in rTMS-treated patients: 84% for the treated side vs. 47% for the non-treated side of rTMS-treated patients and 45% for controls, p=0.016; 74% for treated side vs. 26% for non-treated side of rTMS-treated patients and 40% for controls, p=0.009, respectively (Fig. 1B, 1C).
The NLI changed to 15.8% (3 subjects) in rTMS-treated patients and 25% (5 subjects) in controls during the follow-up period without any statistical difference (Table 5). The AIS changed from C to D in 2 rTMS-treated patients and controls, and there was no relationship between duration from onset to rTMS treatment and neurological and functional changes in rTMS-treated patients (data not shown).
DISCUSSION
In the past, numerous experiments and clinical trials have been performed to investigate post-SCI functional restoration by modulation of inflammation and secondary injury, enhancement of axonal regeneration or remyelination or neuronal plasticity. Neuronal plasticity is represented by brain remapping, collateral sprouting of spared axons, and synaptic changes that allow neurons in the central nervous system to compensate for neuronal injury and to adjust their activity in response to new environments. Remapping of the motor cortex has been noticed subsequent to partial cervical spinal cord transection in mice [7]. Also, it has been observed that some injured motor tracts sprout collaterally and integrate into propriospinal circuits and even cross the midline bypassing the lesions after cervical spinal cord hemisection in rodents [8,21]. However, in most of the cases, spontaneous plasticity changes compensatory to SCI are not sufficient to achieve functional restoration following SCI. Stimulation of the brain or spinal cord might boost post-SCI neuronal plasticity by enhancing the strength of the synaptic connections [22], to which end, task-specific rehabilitation, electrical stimulation, magnetic stimulation or their combination have been suggested as strategies in previous reports [23-26].
rTMS has several advantages like non-invasiveness, painlessness, and applicability to severely disabled patients who cannot perform the task-specific exercise. Some neurological disorders including stroke [27,28], Parkinson disease [29], multiple sclerosis [30], and SCI [31-33] have been treated with rTMS, and a few neurological and functional improvements have been reported until date [34]. The exact treatment mechanism of rTMS in neurological disorders is still unclear, but some possibilities involving the following mechanisms have been suggested: synaptic plasticity via long-term potentiation and depression; neurotrophic effects including those of brain-derived neurotrophic factor and glutamate; anti-apoptotic effects, and magnetic-field-induced biophysiological effects [35,36]. Previous studies have reported some differences in neurological and functional improvement in SCI patients subsequent to application of rTMS. For example, rTMS at 5 Hz was not helpful for the improvement of neurological status; functional improvement was seen only in 2 of 15 chronic SCI patients 2 weeks after treatment [32], higher-frequency (10 Hz) rTMS enhanced the neurological and functional improvement in 4 chronic SCI patients 3 weeks after treatment [33], and even though 20 sessions of high-frequency (20 Hz) rTMS treatment before robot-assisted gait training might have improved the gait function in subacute or chronic SCI patients just after treatment, the observed neurological improvement was not different between sham and rTMS-treated groups [31]. The relationship between the frequency of rTMS and functional improvement after SCI is not clear due to the small number of clinical trials; moreover, variations in the persistence of the therapeutic effect have been noted in different studies. Previous studies have reported that high-frequency (10 Hz) rTMS can induce long-lasting plasticity of excitatory postsynapses in an animal slice culture system [37] and could be more helpful in improving the grip strength in stroke patients than low-frequency (1 Hz) rTMS [38]. However, previous clinical trials on rTMS treatment of SCI patients involved follow-up of patients only for 2–4 weeks after treatment [32,33]; therefore, it cannot be claimed that the long-term effects of rTMS treatment have been identified clinically. It was observed that for a fine motor task, writing time and score were improved on the treated side in rTMS-treated patients, whereas the improvement in grip and pinch strength was similar in both the treated and non-treated sides (Table 3, Fig. 1). The recovery patterns for dexterity and hand strength might differ according to the complexity of movement, which, in cases of unilateral stroke, is dominated by two or more pathways on both the sides [39]. Nonetheless, a direct comparison was not possible in the present case, as we performed rTMS application unilaterally to bilaterally injured CCS patients. In this study, sensory score change of upper extremity was not apparent in the rTMS treatment group or control group, unlike motor score. Although a previous study reported a partial change in the sensory score 3 weeks after rTMS treatment [33], the 4-week follow-up period was not adequate for delineation of overall motor and sensory changes. We did not observe any further effects on NLI or AIS improvement in rTMS-treated patients beyond the control in this study; however, previous studies have shown different results. A study, including a sham group, reported no effect of rTMS treatment on AIS improvement [32], whereas the effect of rTMS on neurological or functional recovery was apparent in combination with robot gait training [31] or in non-control studies [33]. All the subjects in the present study were CCS, and most of the initial AIS were D (84.2% of rTMS-treated patients; 90% of controls); therefore, small changes in neurological or functional status on the treated side might not be sufficient to change the neurological injury level or severity of both the sides in CCS. No incidences of adverse effects were observed during rTMS treatment or the follow-up period. Previous studies have reported some minor adverse effects of rTMS, including headache, seizure, scalp pain, and facial twitching during rTMS application [29,40].
The present study has several limitations. First, we did not perform sham rTMS treatment for the control group, as the subjects were not willing to undergo the treatment. Therefore, we cannot rule out any bias that might have arisen from the lack of a sham operation or randomization. Second, the follow-up period was only 5 weeks from initial assessments, which is not long enough for detection of any long-lasting effects of rTMS treatment.
In conclusion, our findings suggest that rTMS treatment of SCI patients, especially those with CCS, can enhance motor recovery of upper extremity and some functional fine motor task performance on the treated side.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by grants (No. NRF2015R1A2A1A15053883 and NRF-2015R1D1A1A02061196) from the National Research Foundation of Korea (NRF) and the Korea Health Technology R&D Project (No. HI14C0522) by the Ministry of Health & Welfare, Republic of Korea.