Risk Factor of Visuospatial Neglect: A Study of Association Between Visuospatial Neglect and Anemia
Article information
Abstract
Objective
To investigate the correlation between visuospatial neglect and anemia in patients with right cerebral infarction, as well as to identify the risk factor of neglect and furnish preliminary data on rehabilitation management.
Methods
The line bisection test and Albert test were conducted on subjects with right cerebral infarction in order to analyze neglect severity. Multiple linear regression analysis was conducted to investigate correlation between neglect severity and hemoglobin and hematocrit level. Logistic regression analysis was applied to identify the risk factor of neglect.
Results
Visuospatial neglect was observed in 33 subjects out of 124. Hemoglobin and hematocrit were not directly correlated with visuospatial neglect severity, whereas infarct size was directly correlated. Subjects with visuospatial neglect were characterized by a large infarct size, a low score in the Mini-Mental State Examination and long hospital stay.
Conclusion
In this study, visuospatial neglect was found to be uncorrelated with anemia. It implies that emphasis should be placed on the early detection of anemia and neglect in patients with left hemiplegia, the formulation of respective therapeutic plans and improvement of prognosis. The study found that the possibility of a visuospatial neglect occurrence increases with infarct size. In this regard, it is required that visuospatial neglect was detected and treated in the earliest possible stage, notwithstanding the difficulty that lies in the precise measurement of the severity.
INTRODUCTION
Unilateral visuospatial neglect is defined as where any responses do not or cannot be produced to a significant stimulus, as given to the other side of the damaged cerebral hemisphere. The prognosis tends to be poorer in patients with visuospatial neglect who have had an acute stroke in the right hemisphere than those who did not [1-4]. Patients with visuospatial neglect have difficulties in the activities of daily living and thus need to be rehabilitated much longer [3,4]. Gottesman et al. [5] reported that visuospatial neglect became severe in elderly patients with a stroke in the right hemisphere. There have been few studies on the risk factors of visuospatial neglect.
Ordinarily, hemoglobin or hematocrit level falls in patients with acute stroke [6,7]. Anemia caused by a stroke may lead to death or have a poor prognosis, but the connection has not as yet been studied fully. Tanne et al. [6] has reported that anemia may lead to an acute stroke with a poor prognosis and that the same applies to an excessively high level of hemoglobin. Gottesman et al. [8] reported that an excessively high or low level of hemoglobin brought about a decrease in cerebral perfusion and oxygen delivery and therefore worsened visuospatial neglect in patients with right cerebral infarction. It provides the only study on the correlation between hemoglobin and visuospatial neglect. Previous studies have not found any factor other than the age in the right cerebral lesion cases [9]. According to a recent study on the elderly populations in the West, there is a wide deviation in the prevalence of anemia from 4.4% to 28% [10-16]. In comparison, in the case of elderly Koreans, the deviation marks from 8.33% to 13.6% [17]. In Koreans, moreover, the case history of stroke has been reported to be a risk factor that increases the frequency of anemia [17].
This study is to investigate the correlation between visuospatial neglect and anemia in Koreans with right cerebral infarction, as well as to compare the results with previous studies and, by extension, to identify the risk factors of visuospatial neglect. The results are expected to provide preliminary data on the rehabilitation management.
MATERIALS AND METHODS
Subjects
This study was retrospectively conducted on patients who had a right ischemic stroke and were rehabilitated at this hospital between January 2007 and September 2012. There were 22 excluded cases due to the following: severe cognitive impairment (n=13), second attack (n=7), lung cancer (n=1), and visual field defect (n=1). Finally, 124 patients were subject to this study. All the subjects possessed the cognitive ability for the line bisection test and Albert test and had a magnetic resonance imaging (MRI) brain scan.
Methods
This study was conducted with the approval of the Institutional Review Board. All the subjects had an MRI brain scan and blood test within 24 hours following a neurological treatment. Anemia was defined as where the hemoglobin level was less than 14 g/dL in males or 12 g/dL in females [18]. Within 24 hours after being transferred to the Department of Rehabilitation Medicine, another blood test was run and the line bisection test and Albert test under the direction of an experienced physiatrist were conducted. The patients were diagnosed as unilateral visuospatial neglect through the symptoms of neglect (functional deficits in real-life situations as observed by experienced physiatrists), line bisection test and Albert test. The line bisection test asks the subjects to bisect 20 horizontal lines. The invigilator gave subjects a demonstration, bisecting the top and bottom line, and the subjects bisected the other 18 lines. The deviation between a real midpoint and one marked by the subject was converted into a percentage. The percentage results were added up, wherewith the results were evaluated. The deviation above 10% in line bisection test was determined visuospatial neglect [19]. The Albert test is to mark a total of 40 oblique lines (4 in the middle, 18 in the right side, and 18 in the left side) on an A4 paper. Likewise, the invigilator gave subjects a demonstration, marking 4 lines in the middle, and then the subjects marked the other 36 lines. The results were evaluated with the percentage of unmarked lines. The patients who could not check above five lines in the left side were diagnosed as having visuospatial neglect [20]. The number of days it took each patient to be transferred from the Department of Neurology to Rehabilitation Medicine and the number of hospitalization days were noted. In addition, subjects carried out the tests in the Mini-Mental State Examination (MMSE) within 24 hours of the transfer. Infarct size was converted into a percentage through the 25-area method of semiquantitative method based on diffusion weighted imaging [21]. We classified patients into two groups depending on the presence of visuospatial neglect. In the subgroup with visuospatial neglect, subjects were divided according to the presence of anemia.
Statistical analysis
The data were statistically analyzed with SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). Independent sample t-test was conducted to detect demographic difference between the two groups. Mann-Whitney test was conducted to compare characteristics of the two subgroups. Multiple linear regression with enter method analysis was conducted to identify correlation between visuospatial neglect severity and hemoglobin and hematocrit levels in subjects with visuospatial neglect. Logistic regression analysis with backward stepwise method was conducted to identify risk factors of visuospatial neglect from baseline. The significance level was defined as where the p-value was less than 0.05.
RESULTS
Characteristics according to presence or absence of visuospatial neglect
Out of total 124 patients, 33 subjects were diagnosed with visuospatial neglect. In age and gender, there was no significant difference between subjects with visuospatial neglect and without. Hemoglobin levels of the two groups measured on the day of hospital admission were 13.33±1.88 g/dL in group with neglect and 13.35±1.70 g/dL in group without neglect; and hematocrits were 38.97±4.61% in group with neglect and 38.67±4.56% in the other, showing no statistically significant difference. Also in hemoglobin level and hematocrit measured on the day of transfer, there were no inter-group significant differences. However in subjects with visuospatial neglect, hemoglobin level decreased as much as 0.78±2.08 g/dL and hematocrit decreased as much as 2.98±5.02% on the day of transfer. Also in subjects without visuospatial neglect, hemoglobin level decreased as much as 0.75±1.14 g/dL and hematocrit decreased as much as 1.42±2.23%. The decrease of hematocrit was more severe in patients with neglect than in those without neglect (p=0.048). It averagely took subjects with visuospatial neglect 23.18±15.13 days to be transferred to the Department of Rehabilitation Medicine, while subjects without visuospatial neglect took 21.53±21.42 days. The difference of transfer duration between two groups was without significant difference. The two groups were rehabilitated in the hospital for 52.87±35.65 days in group with neglect and 36.74±30.43 days in the other. The difference of hospital duration between the two groups was without statistically significant difference (p=0.014). Infarct size was 35.03±20.23% in group with neglect and 11.29±11.79% in the other, and thus were significantly larger in subjects with visuospatial neglect (p<0.001). Averagely in MMSE, subjects without visuospatial neglect received 2.36 more points than those with visuospatial neglect (p<0.001) (Table 1).
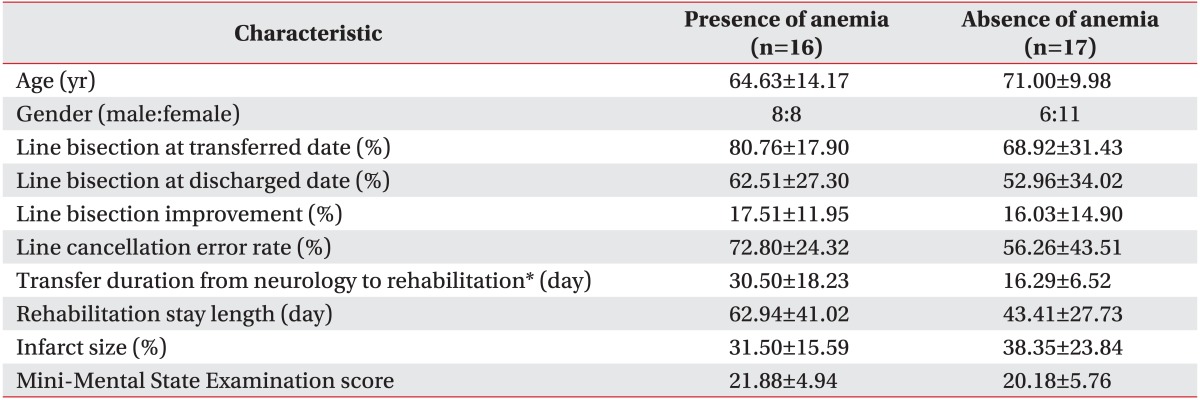
Comparison between presence and absence of anemia in visuospatial neglect group
In subjects with visuospatial neglect, anemia was observed in 16 out of 33 subjects on the day of transfer. Anemia was not significantly correlated with age and gender. In the line bisection test, subjects with anemia correctly divided 80.76±17.90% and 62.51±27.30% on the day of transfer and discharge, respectively. Subjects without anemia got 68.92±31.43% and 52.96±34.02%, respectively. They showed a difference in mean value, which was not statistically significant. In the Albert test, subjects with anemia and those without anemia correctly performed 72.80±24.32% and 56.26±43.51%, respectively, on the day of transfer, and there was no statistically significant difference. It averagely took subjects with anemia 30.50±18.23 days to be transferred from the Department of Neurology to Rehabilitation Medicine, while it took those without anemia 16.29±6.52 days. Thus, subjects with anemia needed a significantly longer transfer time from the Department of Neurology to Rehabilitation Medicine (p=0.001). On the other hand, there were no significant differences in the period of hospital rehabilitation, infarct size, and MMSE (Table 2).
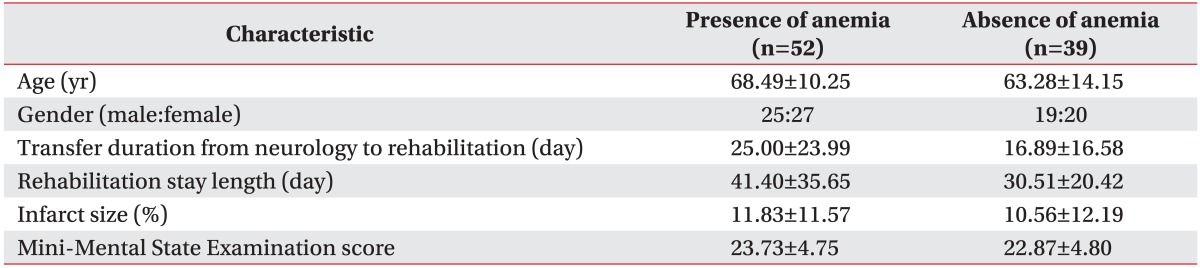
In subjects without visuospatial neglect, anemia was observed in 52 out of 91 patients on the day of transfer. There were no statistically significant differences in age, gender, period of time for transfer, period of hospital rehabilitation, infarct size, and MMSE (Table 3).
Correlation between visuospatial neglect severity and anemic severity
Hemoglobin and hematocrit reflect anemic severity. Results of the line bisection test, conducted on the day of transfer, were negatively correlated with the hemoglobin level measured on the same day. Thus visuospatial neglect severity was found to be in inverse proportion to the hemoglobin level (Fig. 1). However after age, gender, infarct size, and MMSE were corrected by confounding the variables, there were found to be no correlations. After correcting for the four factors, the line bisection test and Albert test showed a negative correlation with hemoglobin and hematocrit levels on the day of hospital admission and transfer. It was observed that visuospatial neglect severity was in inverse proportion to hemoglobin and hematocrit, without statistical significance (Table 4).

The graph shows that the line bisection text, conducted on the day of transfer, was negatively correlated with the hemoglobin (Hb) level without adjustment for the age, gender, infarct size, and Mini-Mental State Examination.
Risk factor of visuospatial neglect
From gender, age, infarct size, MMSE, and hemoglobin measured on the day of hospital admission and transfer, infarct size was identified as a risk factor of visuospatial neglect. Degree of risk was 1.105. It means that the possibility of visuospatial neglect occurring increases with the infarct size. Other factors were not regarded as risk factors of visuospatial neglect (Table 5).
DISCUSSION
This study investigated correlations between visuospatial neglect and anemia. In the visuospatial neglect group, hematocrit was more severely decreased than in patients without neglect. In considering influence of other factors, subjects having lower levels of hemoglobin scored higher in the line bisection test, which showed that anemic severity and visuospatial neglect severity were proportional to each other. It was found however that they were not in direct correlation when unaffected by gender, age, infarct size, and cognitive ability. Gottesman et al. [8] reported that visuospatial neglect became severer in cases where hemoglobin level rose or fell beyond the normal even when unaffected by other factors. Contrariwise, this study shows that visuospatial neglect is not directly correlated with the severity and occurrence of anemia. In the study of Gottesman et al. [8], visuospatial neglect was observed in 101 patients out of 203, a result highly different from a previous cohort study in which visuospatial neglect was observed in 24.7% to 31.1% of 1,281 patients. In their study, moreover, hemoglobin levels were excessively low in most patients [9]. In this study, as in the cohort study, visuospatial neglect was observed in 26.6% of subjects, and hemoglobin levels had an even distribution from 8 to 18 g/dL. It suggests that the results may be generalized to be much more. Most studies, conducted on the nearly homogenous Korean population, have been consistent in the frequency of anemia, which facilitates an independent comparison between anemia and visuospatial neglect [10].
Altogether, it appears that visuospatial neglect is not directly affected by anemia but is affected by one or more of internal or chronic diseases related to anemia. Patients with anemia are more likely to contract diabetes, hyperlipidemia, chronic renal failure, and cardiovascular diseases and therefore are exposed to a higher risk of death. Also diabetes and old age have been reported to worsen the prognosis of stroke [4,22]. Another report has noted that underlying diseases affected the prognosis of stroke [23,24]. In this respect there is a need to carry out further studies on the internal diseases that affect visuospatial neglect.
Previous studies have identified age and right hemisphere damage as risk factors of visuospatial neglect, but have not addressed the influence of infarct size on visuospatial neglect [9]. In the study of Gottesman et al. [8], however, infarct size was regarded as a control variable, with consideration for the correlation between infarction size and visuospatial neglect severity. This study aimed to identify the risk factor of visuospatial neglect between the gender, age, infarct size, MMSE, and hemoglobin and finally found infarct size to be the risk factor. Specifically, the possibility of visuospatial neglect occurring increased with the infarct size, while other factors did not affect it.
Previous studies reported that visuospatial neglect delayed the recovery of hemiplegic patients with prolonged period of hospitalization [3,4]. In this study, period of hospitalization was prolonged not only by visuospatial neglect but by comorbidity of visuospatial neglect and anemia. Nybo et al. [7] reported that a stroke had poor prognosis when under the influence of anemia. Tanne et al. [6] reported that anemia negatively affected acute stroke-related mortality and disability. Regardless of visuospatial neglect, hemoglobin level and hematocrit significantly decreased on the day of transfer rather than on the day of admission. The results were consistent with the study of Fisher and Meiselman [25], who reported that hematologic changes, a decrease in hemoglobin and hematocrit, might arise in patients with acute stroke. Accordingly, it is necessary to conduct hematologic examination for the presence of anemia and monitor changes in hemoglobin and hematocrit levels in patients with visuospatial neglect, prior to rehabilitation management, and unravel the pathogenic mechanism.
Another finding is that patients with visuospatial neglect scored lower in MMSE in comparison to those without visuospatial neglect. A previous study hypothesized that a decline in concentration may be a cause of visuospatial neglect [26]. In fact, cognitive function is closely related to the treatment for visuospatial neglect, and the rehabilitation program requires patient's concentration [27-31]. Thus, it is required to precheck for cognitive impairment that often arises in patients with right cerebral infarction.
The limitations of this study are as follows. First, it was difficult to investigate the correlation between hemoglobin level and visuospatial neglect due to insufficient number of subjects. Second, lesion location of stroke could not be considered. Third, factors affecting visuospatial neglect early in the attack could not be assessed due to failure to conduct the line bisection or Albert test on subjects under neurologic treatments. Fourth, reasons for hemoglobin level decrease and longer hospitalization could not be determined due to failure to analyze subjects' internal disease and nutritive conditions. Fifth, there may be a selection bias from the exclusion of patients with visuospatial neglect who were not transferred from the Department of Neurology to Rehabilitation Medicine.
Considerations for further studies are to recruit more patients with visuospatial neglect, conduct the line bisection test and Albert test early on in cooperation with neurologists and to apply various tests, such as the clock copy test, oral reading test, and neglect test to define perceptual extrapersonal neglect and representational neglect, including tests using virtual reality technologies, behavioral inattention test, modified fluff test, and modified comb test [32-34]. Furthermore, it is necessary to classify anemic patterns in the interest of effective treatment and explicate the link between visuospatial neglect and hematologic indexes, such as ferritin, peripheral blood, total iron binding capacity, and plasma iron.
In conclusion, visuospatial neglect was found to be uncorrelated with hemoglobin and hematocrit levels directly in the Korean population. It implies that we may not expect improvement of neglect followed by a treatment of anemia. The incidence of anemia was increased, and the hematologic levels (hemoglobin and hematocrit) were decreased during hospitalization. Therefore, respective detection and management of anemia and visuospatial neglect are important in left hemiplegia. As mentioned above, the possibility of visuospatial neglect occurrence increases with infarct size. In this regard, it is required that visuospatial neglect be detected in the early stages for patients with large cerebral infarction, notwithstanding the difficulty that lies in the precise measurement of the severity due to patient's cognitive disorder and aphasia. In addition, there is a need to establish guidelines on the rehabilitation programs with accurate follow-ups.
Notes
No potential conflict of interest relevant to this article was reported.