The Utility of Ultrasonography for the Diagnosis of Developmental Dysplasia of Hip Joint in Congenital Muscular Torticollis
Article information
Abstract
Objective
To determine whether a routine ultrasonography (US) is necessary for diagnosis of developmental dysplasia of hip (DDH), presenting with congenital muscular torticollis (CMT).
Methods
Cases of 133 patients (81 males, 52 females) diagnosed as CMT were reviewed, retrospectively. We reviewed the medical charts and diagnostic examination. We also assessed the coincidence of CMT and DDH, and investigated the clinical features of CMT related to DDH.
Results
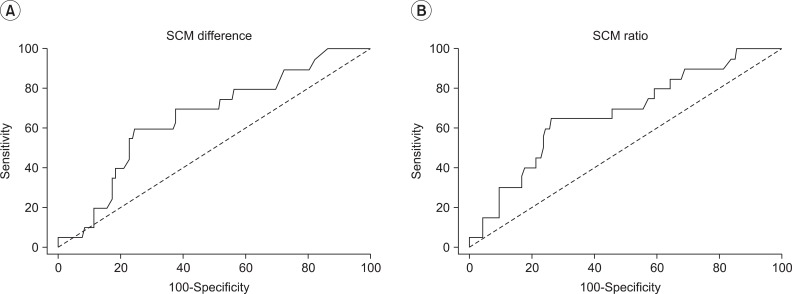
Twenty (15.0%) patients out of 133 CMT patients were diagnosed as having DDH by US. Of whom, 8 patients were radiographically positive and 4 patients were both clinically and radiographically positive. Nine patients were treated with a harness and 1 of them needed closed reduction and casting. Out of 9 patients treated with a harness, only 4 were clinically positive. The difference and ratio of the sternocleidomastoid (SCM) muscle thickness between the normal and abnormal side was significantly greater in DDH patients (p=0.014). Further, receiver operating characteristic analysis showed when the SCM ratio is greater than 2.08 and the SCM difference is greater than 6.1 mm, the efficiency of US for the diagnosis of the DDH was found to be the best (p<0.05).
Conclusion
To evaluate DDH, physical examination showed low sensitivity and radiologic study has limitation for the child before 4 to 6 months of age. Therefore, we recommend that hip is screened by US for the diagnosis of DDH associated with CMT when physical examination is positive or CMT patients with large SCM difference and high SCM ratio.
INTRODUCTION
Newborns with developmental dysplasia of the hip (DDH) joint and congenital muscular torticollis (CMT) are reported with the incidence as 0.017% to 1.9% and 1.0%, respectively; they are comparatively common orthopedic anomalies [1-3]. The incidence of the coexistence of CMT and DDH is reported as 0% to 29% [1,4], and 4.5% among them needed treatments [2]. These results suggested that patients with CMT or DDH should be evaluated with either disease. For the diagnosis of DDH, physical examination may obtain different interpretations between examiners, and is likely difficult to detect DDH [1,5].
Although simple radiographic film of hip is generally accepted as a good diagnostic tool for DDH, there are some limitations of the DDH diagnosis in infants younger than 3 months of age, who has not yet completely ossified [2]. Early diagnosis and treatment for DDH may result in good prognosis, but the late finding may lead to impairments, such as dislocation of hip joint.
In recent years, hip ultrasonography (US) has appeared as an effective tool for the early diagnosis of DDH in newborns. US is an effective and noninvasive method without radiation, but due to its high cost there are still some controversial issues to use US as a screening method [2,6]. The purpose of this study was to investigate whether routine US is a useful measurement for the diagnosis of DDH, presented CMT.
MATERIALS AND METHODS
This retrospective study was approved by the Institutional Review Board of our hospital with the informed consent waived. We reviewed the medical records of 201 patients who visited our hospital due to abnormal posture of the head and neck, from September 2008 to November 2011. Of these patients, 78 were excluded from the study under each criterion as follows; evidence of other neurodevelopmental disorders causing abnormal posture of the head and neck, ocular torticollis, and a loss of follow-up. Patients who did not take examinations at our hospital were also excluded. Of the 133 CMT patients, 81 males and 52 females were included in this study. The diagnosis of CMT was made when the following criteria were included: 1) sternocleidomastoid (SCM) mass on physical examination, 2) limited neck rotation toward torticollis side, 3) limited neck tilting toward nontorticollis side, and 4) differed thickness and echogenecity of the SCM between both sides by US. We also reviewed medical history, related risk factors, asymmetry of the skull and face, and presence of DDH.
Diagnosis of DDH was based on physical examination, including limitation of abduction in the hip joint, positive findings from the Ortolani and the Barlow tests by an orthopedic surgeon.
Also DDH was diagnosed and classified with simple X-ray and US by an experienced radiologist. On a simple X-ray, DDH was diagnosed with discontinue of the Shenton's line, abnormality in the acetabular index and the migration index.
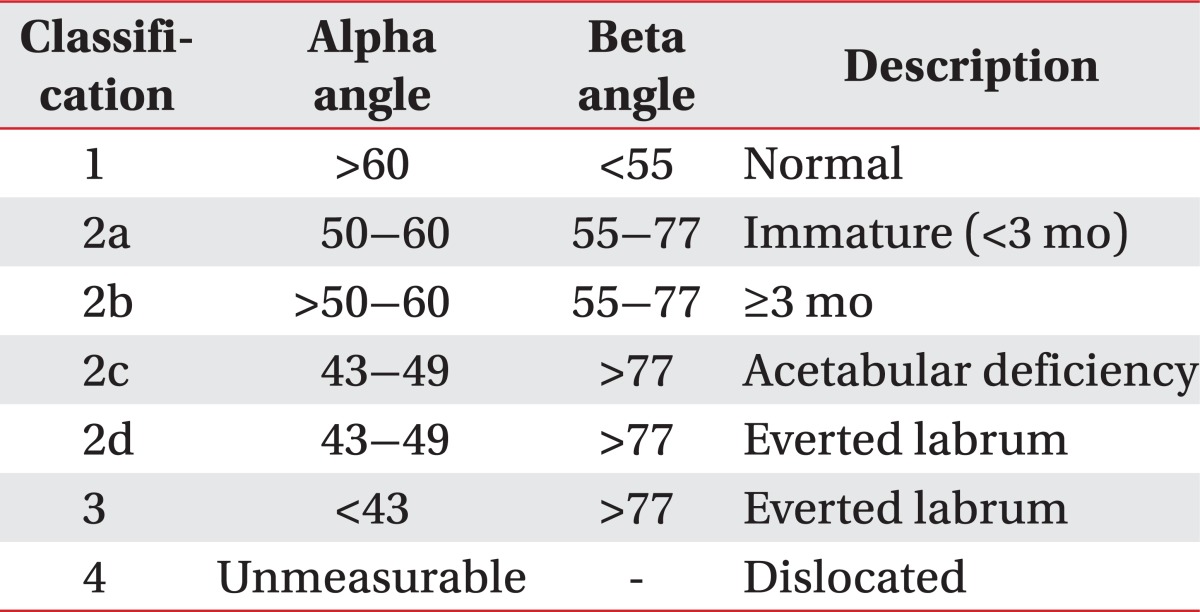
The hip US were taken using a 9 mH linear transducer LOGIQ 9 (GE Healthcare, Milwaukee, WI, USA) by the Graf method. By the Graf method, as the patient was placed in the lateral decubitus position, the alpha angle (α) corresponding to the inclination of the bony acetabulum and the beta angle (β) corresponding to the inclination of the cartilaginous acetabulum on a coronal view of the hip joint, were calculated and classified (Table 1) [7,8].
We divided patients into two groups; group 1 consists of patients with CMT only and group 2 includes patients with DDH and CMT coexisting. We also investigated a relationship between CMT, DDH and medical history.
All statistical analyses in this study were carried out using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Mann-Whitney tests were used for the difference and the ratio of SCM thickness between the normal and the affected sides, gestational age, birth weight for the comparison between the two groups. Fisher's exact tests were used to compare the frequencies of categorical variables, such as mode of birth, presentation, sex, date of first clinical examination, birth order, and oligohydramnios, between groups 1 and 2. We calculated receiver operator characteristic (ROC) curve for relation between US necessity and the differences in the SCM thickness and difference ratios of SCM. The level of statistical significance was regarded as a p-value less than 0.05.
RESULTS
Out of 133 CMT patients (52 females and 83 males), 20 patients (11 females and 9 males) had abnormal ultrasound examination. This gave the frequencies of 17.7%. Female showed a higher frequency of DDH, but it was not statistically significant.
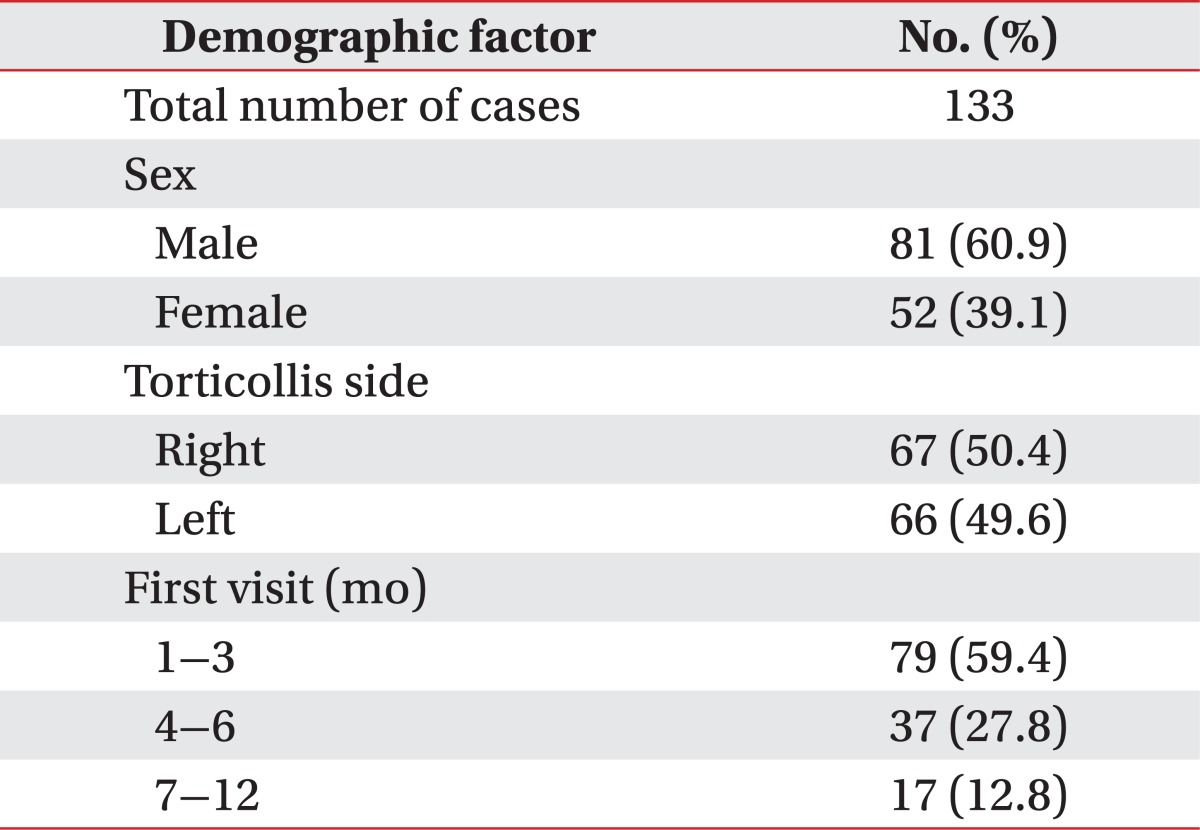
Among the total of 133 CMT patients, 67 (50.4%) patients had lesions on the right side, while 66 (49.6%) patients had lesions on the left side; according to the side of torticollis, infants received their first clinical examination before 3 months old were 79 (59.4%), 4 to 6 months were 37 (27.8%), and over 7 months were 17 (12.8%) (Table 2).
Out of the 20 patients with coexisted CMT and DDH, distributions of the CMT side were 13 (65%) patients on the right side, and 7 (35%) patients on the left side. Among these, the abnormal side of hip joints was distributed as follows; only 7 (35%) patients on the right side, 9 (45%) patients on the left, 4 (20%) patients on both sides, and 5 (25%) patients on each other side of the CMT side.
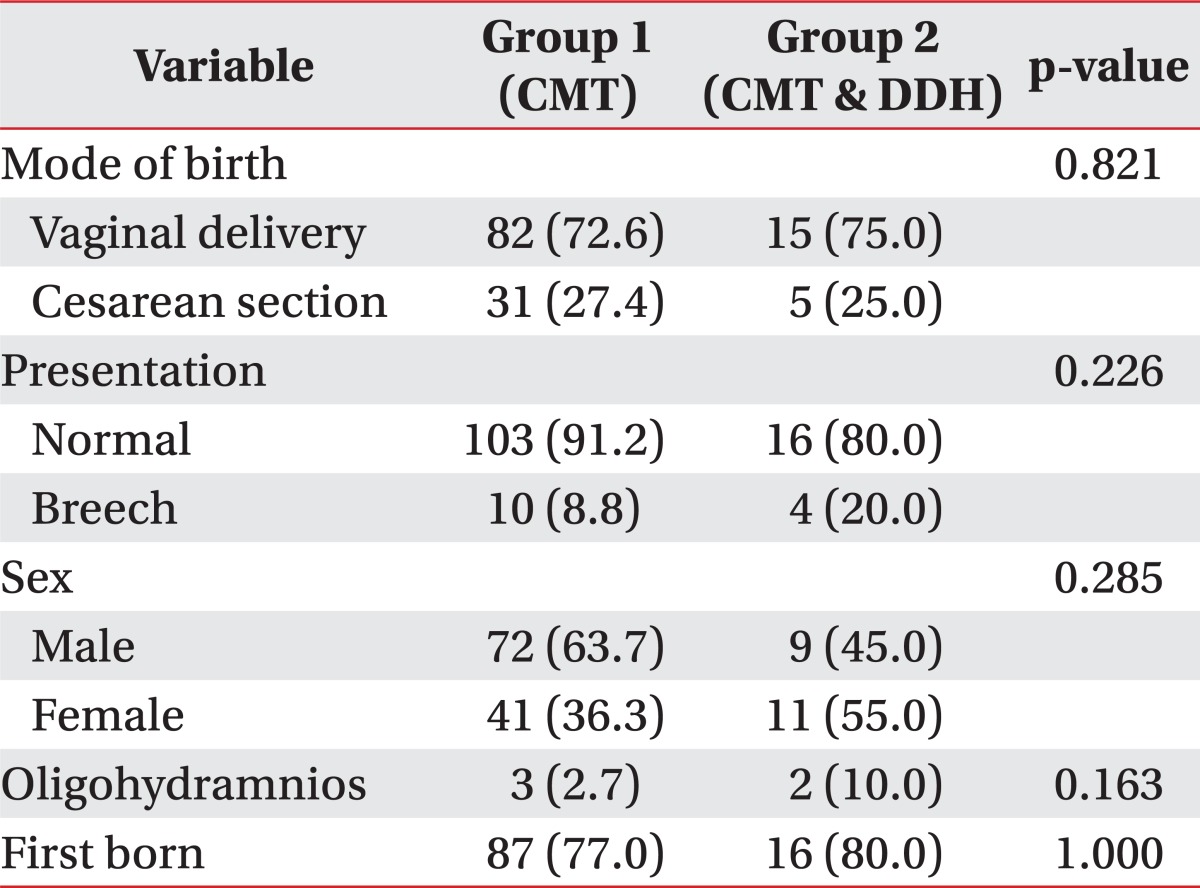
The distribution of risk factors and physical examination, according to radiologic diagnosis and final clinical diagnosis, is shown in Table 3.
Only 4 (20%) out of 20 patients diagnosed with DDH by US had a positive physical examination finding, and 8 (40%) patients had positive simple X-ray finding. Four patients with positive physical examination also showed simple X-ray abnormality. Eleven (55%) patients were improved with wide diaper use and abduction exercise of hip joint, and in 8 out of 9 patients, the treatments needed were treated with hip abduction orthosis (harness). One patient who was diagnosed at 7 months old showed progress with a harness treatment, after closed reduction and serial casting (Table 3).
Related risk factors, such as mode of delivery, weight on birth, presentation, gestational age, being firstborn, and oligohydramnios between two groups, did not show a significant difference. The average for the first received clinical examination was 97±81 days after birth in group 1, 69±56 days after birth in group 2, and the averages between the two groups were statistically different.
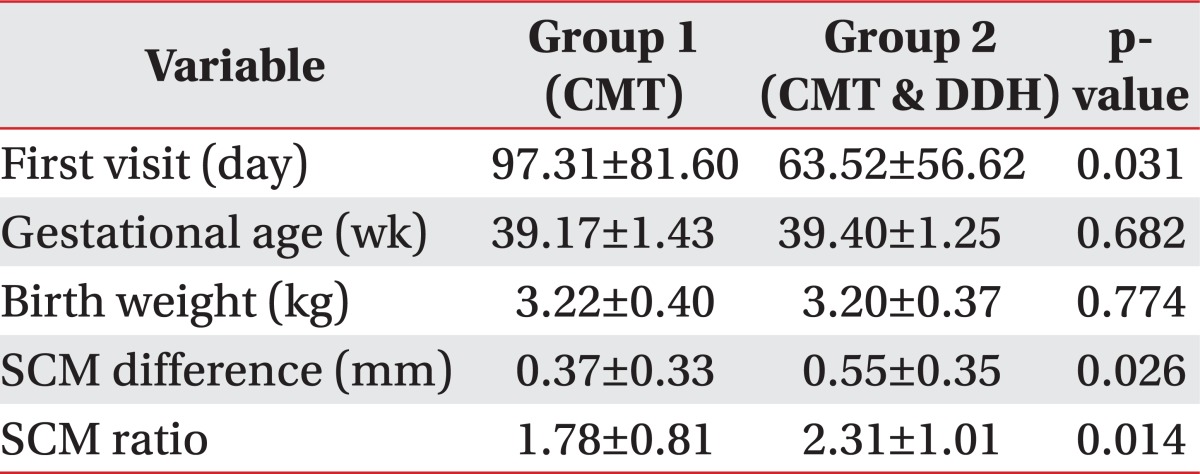
The mean of the SCM thickness difference was 0.37±0.33 cm in group 1, 0.55±0.35 cm in group 2, and the mean of the SCM thickness ratio was 1.78±0.81 in group 1, and 2.31±1.01 in group 2. Group 2 showed significantly higher means of these two measurements (Tables 4, 5).
Validity and reliability achieved high scores when the thickness difference was over 0.61 cm (p=0.015), and over 2.08 in the thickness ratio (p=0.0091) with statistical significance according to ROC curve analysis (Fig. 1).
DISCUSSION
DDH results from an abnormal position between femoral head and acetabulum, and classified by dislocation, subluxation and instability [9]. Even the precise etiology of DDH is uncertain, and conditions, such as physiological, environmental, and genetic factors were well known to be involved [10].
Also, metatarsal adductus, congenital dislocation of knee joint, and CMT are common conditions with DDH [6,11,12]. The association with CMT and DDH is well established. Lidge et al. [13] and Do [14] suggested that the malposition in the uterus of fetus, which is one of the CMT risk factors or with insufficient space of uterus, CMT could lead DDH in CMT patients as risk factors. Hamanishi and Tanaka [15] studied physiological conditions, according to the position in the uterus and the CMT side, and the side of hip joint problems was found on the same side.
In this study CMT patients showed even frequencies of the torticollis side (67 patients on the right side, 66 patients on the left side) and the DDH side was higher on the left side with 9 patients, compared with 7 patients on the right side and 4 on both sides.
The lesion side of the torticollis and the DDH appeared more on the same side with 11 (55%) patients, than on the other side, which was seen in 5 (25%) patients. DDH is known for more frequent occurrence with related risk factors, including oligohydramnios, breech presentation, first born, female, low birth weight, cesareans section, and preterm infant [1,2,5,9].
In this study, although between mode of delivery and presence of DDH showed no relationship, DDH was diagnosed more in infants with breech presentation, oligohydramnios, being first born and female without statistical significance.
For the early diagnosis of DDH, physical examination and US are recommended after 4-6 weeks after birth [16,17]. The Graf method is widely used for the diagnosis of DDH and showed a high sensitivity [18].
Rosenberg et al. [19] reported that the frequency of DDH was 0.8%, and 47% of these were diagnosed by a physical examination and others were diagnosed only by US in their study of 9,199 infants. Several studies reported sensitivity of physical examination as 6% to 50% [5,20,21], these results suggested US examination as a necessary measurement.
Zdravkovic and Stojanovic [9] presented the results concerning the treatment costs and that operation and rehabilitation of DDH require more costs than simple prevention of DDH. Wirth et al. [6] proposed the necessity of US from a study of 12,331 patients; US screening could decrease duration of treatments, operation rate and worsening DDH.
Prognosis of DDH depends on early diagnosis and treatments [5]. Treatments of DDH implement within 6 weeks after birth and at least within 3 months old can lead to good results [9].
The limitation of hip joint abduction based on physical examinations to diagnosis DDH generally appears as a contraction of adductor muscle of dislocated hip joint at 3 months old after birth. The Ortolani and the Barlow tests may not give sufficient results in the dysplasia or the subluxation conditions, and have low sensitivity as tools to determine a possibility of manual reduction in dislocated patients. Because simple X-ray has low diagnostic value for infants younger than 4 to 6 months old [22], we consider that US screening is needed for an early diagnosis of DDH.
On the contrary, high costs for US use remain controversy over its necessity. Castelein et al. [23] reported 4 DDH patients after 6 months follow-up from 101 abnormal hips by US with negative results on a physical examination and suggested the use of US screening for only high risk infants, and not all infants, because US was too sensitive that clinically unimportant instability was diagnosed with DDH. The American Academy of Pediatrics recommends radiologic examination of the hip joint in female infants [24,25].
Kim et al. [1] reported in his study of DDH and CMT that 18 out of 21 CMT patients had positive US findings, and amongst them, two received the harness treatment. Those two treated patients also had a positive finding by a physical examination. Thus, Kim et al. [1] suggested that only the positive cases from a physical examination should be screened with US because majority of DDH diagnosed with US became normal without any treatment.
In this study the results from 3 measurements, including physical examination, simple X-ray, and US, did not always reach an agreement, and the sensitivity of physical examination was 20.0% (Table 3). Eight out of 20 DDH patients received harness treatments for several months, and 1 patient was treated with a closed reduction and serial casting, in addition, only 4 patients were diagnosed with DDH by a physical examination. Therefore, our study proposes that US screening is needed for an early detection of DDH, despite the negative results from a physical examination.
DDH with CMT patients (group 2) showed significantly higher levels of thickness difference and ratio of SCM, and received their first examination significantly earlier than the other group (Table 5). Degree of CMT was more severe, possibility of DDH occurrence was higher in our study.
According to the ROC curve analysis of association between the sensitivity and the false positive rate (1-specivity), US was an appropriate measurement when patients showed over 0.61 cm of the SCM difference (sensitivity, 60%; specificity, 75%; area under curve [AUC], 0.657; p=0.015) and over 2.08 of the SCM thickness ratio (sensitivity, 65%; specificity, 73%; AUC, 0.673; p=0.009) (Fig. 1).
There are some limitations of this study. Generalization of our results had some limitations due to a small sample size of our study, even though the results showed significant difference based on nonparametic statistics we applied. Our study had insufficient sample size; therefore, we applied nonparametric statistics. Thus, generalization of our results had some limitations, despite the results that showed a significant difference. Additionally, most conditions among mild DDH tend to be normal spontaneously, and US applying in early stage of newborn can lead to over diagnosis, due to physiologic acetabular development insufficiency, but some cases in our study received the US evaluation earlier than 4 to 6 weeks after birth. Thus, some clinically mild patients were also included in our study, these should be considered with further studies.
In conclusion, the sensitivity of the physical examination for early detection of DDH is low and varies depending on the expertise of the evaluators. Also, simple radiography has some limitations. To consider the benefit of early diagnosis of DDH, we recommend using US to screen for DDH in CMT patients when positive on a physical examination, the difference of SCM thickness was over 0.61 cm, and/or over 2.08 of the ratio of SCM thickness.
Notes
No potential conflict of interest relevant to this article was reported.