Ulnar Neuropathy at the Wrist in a Patient with Carpal Tunnel Syndrome after Open Carpal Tunnel Release
Article information
Abstract
Ulnar neuropathy at the wrist is rarely reported as complications of carpal tunnel release. Since it can sometimes be confused with recurrent median neuropathy at the wrist or ulnar neuropathy at the elbow, an electrodiagnostic study is useful for detecting the lesion in detail. We present a case of a 51-year-old woman with a two-week history of right ulnar palm and 5th digit tingling sensation that began 3 months after open carpal tunnel release surgery of the right hand. Electrodiagnostic tests such as segmental nerve conduction studies of the ulnar nerve at the wrist were useful for localization of the lesion, and ultrasonography helped to confirm the presence of the lesion. After conservative management, patient symptoms were progressively relieved. Combined electrodiagnostic studies and ultrasonography may be helpful for diagnosing and detecting ulnar neuropathies of the wrist following carpal tunnel release surgery.
INTRODUCTION
Carpal tunnel syndrome (CTS) is a commonly known condition that is caused by nerve entrapment. Although there are various treatment options, open carpal tunnel release surgery is a frequently performed operation. This procedure provides significant relief of pain and tingling sensation in over 70% of patients.1
The complications of open carpal tunnel release surgery have been well described. MacDonald et al.2 reported a complication incidence of 12% following open carpal tunnel release. Ulnar nerve injury near the wrist may be a rarely reported surgical complication. In particular, delayed ulnar neuropathy at the wrist following surgery is even more rare.3 In this paper, we report a case of delayed ulnar neuropathy at the wrist that was resolved with conservative management following an open carpal tunnel release surgery. This case report demonstrates the usefulness of ultrasonography and segmental nerve conduction studies of the ulnar nerve around the wrist.4
CASE REPORT
A right-handed, 52-year-old woman presented with a two-week history of a tingling sensation on the fifth finger of the right hand, which had started 11 weeks after she had undergone bilateral open carpal tunnel release procedures. After the carpal tunnel releases, the tingling in both hands gradually disappeared, but a new tingling sensation on the right fifth finger commenced 11 weeks after the carpal tunnel release. There was no history of localized, direct trauma around the right wrist after the carpal tunnel release. The physical examination demonstrated mild hypesthesia on the right fifth digit. According to the Medical Research Council scale, the strengths of the right abductor digiti minimi (ADM) and first dorsal interosseous (FDI) muscles were grade 4, whereas other muscle strengths of the right upper extremity, including flexor digitorum profundus III & IV and flexor carpi ulnaris muscles, were grade 5. There was no significant atrophy on the right hypothenar area. Froment's test was negative on both sides, while the nerve percussion sign was positive over the ulnar side of the right wrist. Deep tendon reflexes were normal bilaterally.
Prior to the carpal tunnel release, nerve conduction studies (NCS) had been performed on both upper extremities (Table 1). Bilateral median motor NCS with abductor pollicis brevis (APB) recordings had demonstrated prolonged latency and low amplitude on the left side, with normal responses on the right. Median nerve sensory responses showed prolonged latencies and low amplitudes at the wrist bilaterally. Needle electromyographic findings of the left abductor pollicis brevis muscle revealed abnormal spontaneous activities and polyphasic motor unit potentials with reduced recruitment patterns. The left ulnar motor NCS and bilateral ulnar sensory NCS were normal.
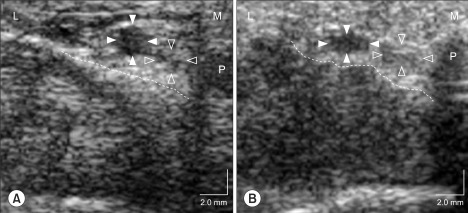
A follow-up electrodiagnostic study performed 10 weeks after the carpal tunnel release demonstrated the improvement of sensory and motor responses in both median nerves, with improved latencies and amplitudes (Table 1, 2). Thirteen weeks after the surgery, a third electrodiagnostic study was performed. Bilateral median sensory and motor responses showed no specific interval changes, as compared to the previous study. However, the right ulnar motor NCS with ADM recordings revealed prolonged latency, and the right ulnar sensory NCS with the fifth digit recordings showed low amplitude in comparison to the other side. The right ulnar motor and sensory short segmental studies at the wrist revealed an abnormally prolonged latency difference between the pisiform bone and 2 cm proximal to the pisiform bone (0.7 and 0.8 ms respectively; upper normal limit in ulnar motor and sensory nerves, 0.5 ms) in addition to a conduction block (54.1%) of the ulnar sensory response over the same segment (Fig. 1-A, B).4 Needle electromyographic findings from the right ulnar innervated muscles revealed no spontaneous activity, although the normal motor unit potentials had reduced recruitment patterns in the ADM and FDI muscles. Subsequent ultrasonography (SONOACE 9900, 7.5 MHz linear probe, Medison, Korea) of the right wrist showed ulnar nerve swelling between the pisiform and 2 cm proximal to the pisiform (Fig. 2-A), as compared to the left side (Fig. 2-B). Also, compared with the pre-operative ultrasonographic finding, mildly flattened ulnar nerve and artery at the level of pisiform and irregular floor line of Guyon's canal were observed (Fig. 3-A, B). Because electrodiagnostic findings suggest a demyelinating process of the ulnar nerve, despite the imaging findings that the nerve was swollen around the wrist, we provided conservative treatment of pain relief and physical therapy (oral non-steroidal anti-inflammatory drug, and infrared heat therapy) after which her symptoms improved. A final follow-up nerve conduction study was performed 4.5 years after the carpal tunnel release and demonstrated spontaneous full recovery of the right ulnar neuropathy at the wrist. There was no abnormally prolonged latency difference or conduction block in the segment between the pisiform and 2 cm proximal to the pisiform along the ulnar motor and sensory segment at the wrist.

Initial ulnar motor and sensory short segment studies (SSS) at the wrist (A, C) demonstrate abnormally prolonged differences in latency within the segment between the pisiform (P) and 2 cm proximal to the pisiform (P+2), as well as a conduction block (54.1%) of the ulnar sensory nerve in the same segment. Long-term follow-up SSS (about 4 years later) revealed complete recovery of the focal ulnar nerve lesion (B, D). AMP: Amplitude, P-3: 3 cm distal to the pisiform, LD1: Latency difference (motor, onset latency; sensory, peak latency) in the segment between P and P+2, LD2: Latency difference in the segment between P and P-3. Asterisks indicate abnormal values.

Longitudinal view of right wrist ultrasonography (A) demonstrates ulnar nerve swelling (arrow) between the pisiform (P) and 2 cm proximal to the P (P+2), as compared to the left side (B). Cross-sectional views (C-F) of the right ulnar nerve reveals a larger area (8 mm2) at the 1 cm proximal to P (P+1, D) than at the other sites (C, E, F; 4-5 mm2). L: Lateral side, M: Medial side, P+3: 3 cm proximal to P.
DISCUSSION
Open carpal tunnel release for CTS is safe and highly effective in relieving pain and paresthesia soon after the procedure.1 It is, however, not without complications. Postoperative complications can be categorized into three classes, which include persistent, recurrent, and new symptoms. Persistent complications occur most frequently, with an incidence of 7 to 20%. The rate of recurrence after a few months in patients who have minimal to moderate symptoms is reported as up to 6%. Most causes of new symptoms may be iatrogenic, and the incidence for new problems is about 1%.5
There are several studies that describe cases in which carpal tunnel syndrome coincides with ulnar nerve entrapment. Cassvan et al.6 reported a 46% incidence of associated ulnar nerve neuropathy at the wrist in a retrospective study of 248 patients with CTS. Recently, a case-control study, including 99 healthy volunteers and 181 patients with CTS, suggested that there might not be a statistically significant association between CTS and ulnar neuropathy at the wrist.7 However, many reports have demonstrated symptomatic and electrophysiologic relief of ulnar neuropathy following carpal tunnel release in patients who had electrophysiologically confirmed carpal tunnel syndrome and ulnar neuropathy at the wrist. Pressures, according to angiocatheter measurements, in the carpal tunnel and in Guyon's canal showed significantly decreased pressures in Guyon's canal after open carpal tunnel release.8
Direct ulnar nerve injury may occur during an open carpal tunnel release because of the nerve's anatomical adjacency, but only one case of delayed ulnar neuropathy at the wrist following open carpal tunnel release has been reported,3 which demonstrated that the translocation of carpal contents resulted in the compression of the ulnar nerve in Guyon's canal several months after open carpal tunnel release. Magnetic resonance imaging of the involved wrist revealed that the superficial and deep finger flexor tendons with the carpal tunnel had been translocated over the hook of hamate and into Guyon's canal.3
In this case, preoperative NCS showed normal ulnar sensory responses bilaterally. In the first follow-up NCS, bilateral ulnar nerves were not tested, but there was no concern about intraoperative ulnar nerve injury, as the symptoms of carpal tunnel syndrome were progressively relieved. In addition, according to the patient, the tingling sensation on the right fifth finger was a new symptom and not the persistence of a residual symptom. Three weeks after the first follow-up study, the third NCS was performed. Despite the electrophysiological improvement of the right median motor and sensory responses, the right ulnar sensory and motor responses displayed delayed latencies, and the sensory response was of decreased amplitude, as compared to the previous study. In particular, the ulnar motor and sensory short segmental study at the wrist demonstrated that the focal lesion of the right ulnar nerve was localized between the pisiform and 2 cm proximal to the pisiform. Focal ulnar nerve swelling at the same site and the mildly flattened ulnar artery and nerve at the level of pisiform were confirmed using ultrasonographic imaging (Fig. 3). Structural change in Guyon's canal (irregular floor line), which was susceptible to irritate the ulnar nerve, may be caused by the loosened transverse carpal ligament and anterior displacement of intracarpal elements. This change may result in decreasing the area of Guyon's canal and flattening the ulnar artery and nerve. Previous ultrasonographic study in carpal tunnel syndrome had reported that the transverse carpal ligament had shown a significant anterior displacement postoperatively at the pisiform level,9 and ulnar neuropathy at the wrist after open carpal tunnel release had suggested to be probably complicated.10 The long-term follow-up NCS revealed complete recovery of the focal ulnar lesion without surgical treatment.
In conclusion, this case report demonstrates a very rare complication of carpal tunnel release. In this case, idiopathic delayed ulnar neuropathy following an open carpal tunnel release with complete recovery did not require surgical treatment. This delayed, idiopathic ulnar neuropathy at the wrist following carpal tunnel release can be easily confused with intra-operative injury or recurrent median neuropathy. It may be caused by the transient irritation of a neural fiber resulting from a postoperative structural change. This case also demonstrates that a combination of segmental electrodiagnosis and ultrasonography can be useful for the differential diagnosis of ulnar neuropathy at the wrist after carpal tunnel release. This report suggests that ulnar neuropathy at the wrist is worth considering as a delayed complication of open carpal tunnel release.