Correlations between Pre-morbid Personality and Depression Scales in Stroke Patients
Article information
Abstract
Objective
To investigate the correlation between pre-morbid personality and depression scales in patients with stroke.
Method
The subjects of this study included 45 patients with stroke and their caregivers. We conducted an interview of patients with Beck Depression Inventory (BDI) and also evaluated general characteristic (age, sex, location of lesion, cause of stroke, duration of illness, educational background, history of medication for depression) and functional level. Caregivers were evaluated with Hamilton Rating Scale for Depression (HRSD) for depressive mood, with NEO-PI (Neuroticism, Extraversion and Openness Personality Inventory) for pre-morbid personality. The results of each questionnaire were analyzed in order to investigate their correlation. The results were statistically analyzed with independent t-test, ANOVA, and Pearson correlation test.
Results
The HRSD score of the caregivers had a significant correlation with the BDI score (p=0.001) of the patients. The BDI score correlated with Neuroticism (p=0.021) and the HRSD score also correlated with Neuroticism (p=0.015). There were no statistical correlation of depression with sex, age, case of stroke, location of lesion, duration of illness and functional level.
Conclusion
Among pre-morbid personalities, neuroticism of NEO-PI is the only factor which is significantly correlated with depression scales in stroke patients. Evaluating pre-morbid personality can be helpful in predicting the depressive mood in stroke patients, so we may have early intervention for it.
INTRODUCTION
The psychological symptoms that may occur after stroke include depression, anger, aggression, anxiety, apathy, catastrophic reaction, psychosis and mania,1 of which the most common symptom is depression.2 1/3-2/3 of patients suffer from post-stroke depression, of which the main symptoms were reportedly loss of energy in 83% of patients, sleep disorder in 67%, increase of brooding in 60%, and hopelessness in 39%.3
Special attention is needed in post-stroke depression because it prevents patients from participating in active rehabilitation, resulting in the failure of rehabilitation.4 Studies show post-stroke depression attributes to the stroke itself, sequelae of stroke, risk factors of major depressive disorder, severe cognitive dysfunction and physical disability after stroke.5 Of the risk factors that predict major depressive disorder, women, family history, and past history are also reported major risk factors of post-stroke depression.6 Pre-morbid personality, in particular neuroticism, which is another risk factor of major depressive disorder, has received little attention.7,8 Relevant studies have been presented several times abroad, but there have been none in Korea.
This study was conducted to determine the correlation between pre-morbid personality and depression scales in stroke patients. Furthermore, its correlation with location of lesion, sex, functional ability, age, cause of stroke, duration of illness (months), presence of underlying disease, educational background, and history of medication for depression was also investigated.
MATERIALS AND METHODS
Subjects
The study included 45 patients who were admitted to our department for stroke from January 2009 to September 2009. Those patients who could not conduct '3 step obey', those with aphasia, and those who suffered other psychological diseases before stroke were excluded. Selected caregivers were restricted to those who had known the patients before stroke and had visited the patients at least once a week.
Methods
Evaluating depression scale
To evaluate the subject's depression scale, BDI (Beck's depression index) standardized by Lee et al.9 was used. The score range was from 0 to 3. With 21 questions in total, 63 was the maximum score. In BDI, generally a person scoring more than 20 was identified as suffering from depression.9 However, depression was specified further as mild, moderate, severe and is open to changes according to other variables such as age. Therefore, this study did not use cut off value, but raw scores. Moreover, when measuring caregivers with HRSD (Hamilton rating scale for depression), the three categories (psychomotor retardation, agitation, insight) that required a direct evaluation of testers were excluded, results were also given in raw scores.
Evaluating pre-morbid personality
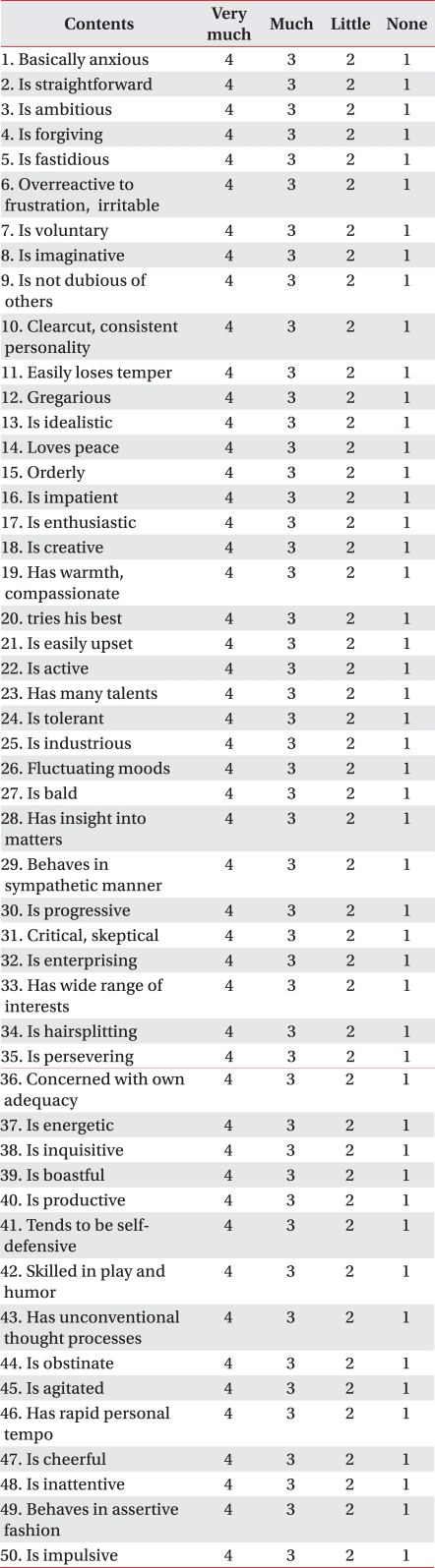
To evaluate premorbid personality, NEO-PI (Neuroticism, Extraversion and Openness Personality Inventory)10 standardized by Kang11 was used. It consists of 50 questions, with 4 scores each, and was convenient for patients and their caregivers to evaluate themselves. This test was used on caregivers who were evaluated with HRSD.
Others
General characteristics of patients (age, sex, location of lesion, cause of stroke, duration of illness, level of education, history of medication for depression) and functional level; K-MBI (Korean Modified Barthel Index), HMS (Hand Movement Scale), FAC (Functional Ambulatory Category); were also assessed.
Statistical analysis
Data was analyzed by SPSS for Windows version 12.0 (SPSS Inc., Chicago, USA), and statistical level of significance was controlled to less than 0.05. Pearson correlation analysis was performed in order to find the correlation between pre-morbid personality and depression scales, between the HRSD score of the caregivers and the BDI score of the patients. The correlation between depression scale and other factors (age, sex, location of lesion, causes of stroke, duration of illness, presence of underlying disease, education background, usage of depression drugs, physical function level) were also investigated, using student t-test and one-way ANOVA according to the factor's number of parameters. Moreover, parameters that were reported to be statistically significant were analyzed with multiple regression analysis.
RESULTS
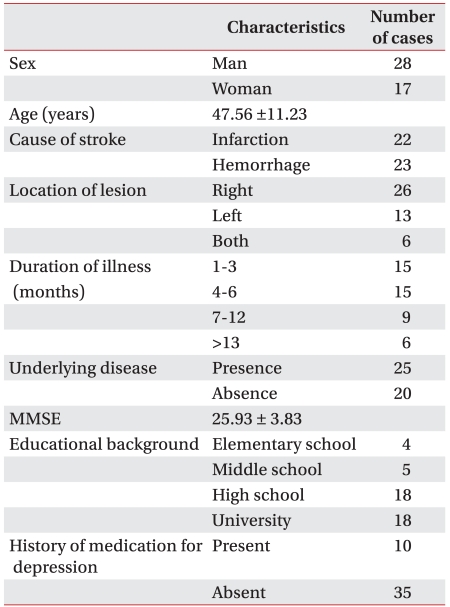
General characteristics of patients (Table 1)
The average age of onset was 47.56±11.23 (range 27-62). Out of the 45 patients, 28 were male and 17 were female. The cause of stroke were found to be cerebral infarction in 22 patients, cerebral hemorrhage in 23, right hemiplegia in 13, left hemiplegia in 26, and quadriplegia in 6. The duration of illness averaged 6.7 months, and 25 patients had underlying diseases while 20 did not. A total of 4 patients had graduated from elementary school, 5 from middle school, 18 from high school, and 18 from university including technical college. Ten patients had been administered depression drugs. Specifically, 7 patients were taking SSRI (1 paroxetine, 3 fluoxetine, 2 sertraline, 1 escitalopram), 2 were taking SNRI (milnacipran), and 1 was taking an atypical antidepressant (bupropion).
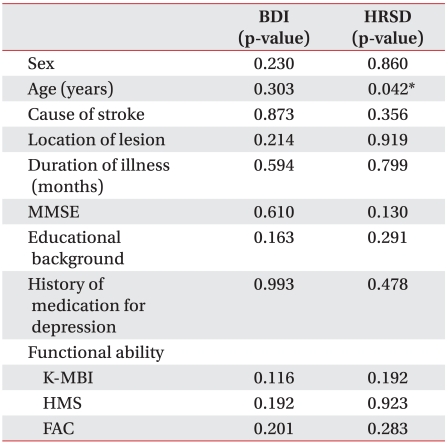
Age and depression scale
There was no significant correlation in age and Beck's depression index (r=0.157, p=0.303), but there was significant correlation in age and Hamilton rating scale for depression (r=0.303, p=0.042).
Sex and depression scale
In BDI, the average score of males was 11.86±8.62, and that of females was 14.94±7.54, which were statistically insignificant (p=0.230). In HRSD, the average score of males was 8.96±6.23, and that of females was 9.29±5.91, which were also statistically insignificant in independent t-test (p=0.860).
The causes of stroke and depression scale
In BDI, the average score of patients with cerebral hemorrhage was 12.83±8.23 and the average score of patients with cerebral infarction was 13.23±8.52, which were statistically insignificant (p=0.873). In HRSD, the average scores of patients with hemorrhage and infarction were 9.91±5.92 and 8.28±6.20, respectively, which were of insignificant (p=0.356).
Location of lesion and depression scale
In BDI, the average score of patients with right hemiplegia was 10.54±7.02, that of patients with left hemiplegia was 14.88±8.97, and that of patients with quadriplegia was 10.33±6.31 which had no statistical significance (p=0.214). The average HRSD score of patients with right hemiplegia was 9.46±4.63, that of patients with left hemiplegia was 8.77±6.20, and that of patients with quadriplegia was 9.09±6.05 again having no statistical significance (p=0.919).
Duration of illness and depression scale
No statistical significance was found in both BDI and duration of illness which were classified into 4 groups (p=0.594). HRSD showed the same result of having no statistical significance with duration of illness (p=0.799).
MMSE (mini-mental state exam) and depression scale
The MMSE average score of patients 25.93±3.83, having no correlation with BDI (r=0.078, p=0.610), but not with HRSD (r=-0.229, p=0.130).
Education background and depression scale
The average BDI score of patients who had finished primary school was 19.25±7.04, that of patients who had graduated from middle school was 7.80±3.96, that of patients who had graduated from high school was 14.33±9.14, and that of patients who had graduated from university was 11.78±7.80, showing no statistical significance (p=0.163). The average HRSD score of patients who had finished primary school was 12.25±4.43, that of patients who had graduated from middle school was 12.80±2.39, that of patients who had graduated from high school was 8.50±6.65, and that of patients who had graduated from university was 7.94±6.12, again showing no statistical significance (p=0.291).
Usage of depression drugs and depression scale
The average BDI score of patients who were taking depression drugs was 13.00±8.67, and that of those patients who were not taking such drugs was 13.03±8.30, which were statistically insignificant (p=0.993). The average HRSD score of patients who were taking depression drugs was 10.20±5.24, and that of those who were not taking such drugs was 8.77±6.30, again statistically insignificant (p=0.478).
K-MBI, HMS, FAC assessed physical function level and depression scale
In case of quadriplegia, the more severely damaged parts were mainly assessed. K-MBI showed a wide range of scores from 10 to 100, not correlating with BDI (r=-0.237, p=0.116) nor HRSD (r=-0.198, p=0.192). HMS also did not correlate with BDI (p=0.192) nor HRSD. FAC did not correlate with BDI (p=0.201), nor HRSD (p=0.283) (Table 2).
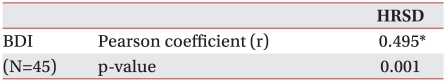
The correlation of BDI with HRSD
BDI and HRSD showed valid correlation (Table 3).
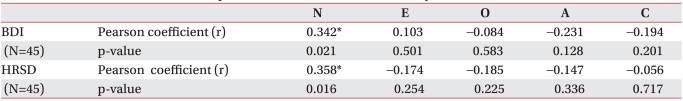
The correlation between depression and pre-morbid personality
Among the types of NEO-PI, BDI showed no statistical cor relation with E (extraversion), O (open ness to experience), A (agreeableness), C (conscientiousness). The only type of personality that correlated statistically with BDI was N (neuroticism). The results were same with the correlation with HRSD. Therefore, it could be concluded that post-stroke depression and neuroticism are correlated with each other (Table 4).
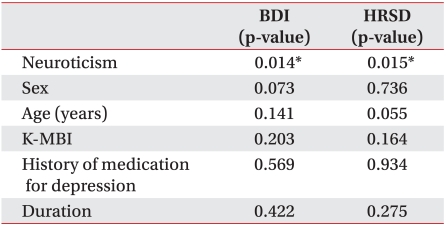
Multiple regression analysis of the main parameters
N (neuroticism) and basic information such as age and sex were results that were significant in univariate study, and the adaptation to ordinary life, usage of depression drugs, and duration of illness were reported as significant in other reports. Therefore, these factors were used as standards for measuring depression scales for multiple regression analysis. In regards to BDI N (neuroticism), sex, age, K-MBI, usage of depression scale, and duration of illness, there were no multicollinearity (Durbin-Watson value: 1.612), and were only significantly correlated with neuroticism. The results were same with HRSD. There were no multicollinearity (Durbin-Watson value: 1.676), and its correlation was only valid with neuroticism (Table 5).
DISCUSSION
According to the study of Robinson et al.12 in 1983 with DSM-III, post-stroke depression has 27% probability of leading to major depressive disorder and 20% to dysthymia. In the study by Astrom et al.13 in 1993, 25% of 73 patients were diagnosed with depression by DSM-III. Another study, the lowest prevalence rates were depressive disorder found in patients that studied in community settings where 14% of the patients were found to have major depression, while 9% had minor depression. In outpatient settings, which vary between 3 months and 3 or more years following stroke, the prevalence rate for major depression was 24.0%, and for minor depression was 23.9%.14 Suicide ideation or pessimism is less frequently seen than apathy, which often demotivates people, in depression.15,16
Lack of energy and depressive moods are one of the major symptoms of depression. In physical terms, cognitive dysfunction or psychological symptoms arouses, distracting people from living an ordinary life. The study conducted by Pyun and Kim17 revealed that a person's adaption of living everyday life was significantly higher when he did not suffer depression. Another study4 relating depression and the result of rehabilitation showed that depression discourages people from participating in active rehabilitation, reducing the probability of achieving the originally aimed goal of rehabilitation. Because depression is a chronic disorder, post-stroke depression is prone to occur at any time. This is problematic not only to the individual but also to the family, eventually expanding as a problem for the whole society. If post-stroke depression were predictable in advance, close observation and support may be given. Special treatment such as education of caregivers, psychological therapy and preventive medication can be also provided. Early detection and treatment of depression is important in the sense that it enables better comprehensive rehabilitation results of not only depression but also stroke.
The most widespread way to determine depression is DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition), but its drawback remains that quantitative analysis is impossible and it requires specialists. Aben et al.,18 reported that HRSD is most similar to DSM-IV and the highest sum of sensitivity and specificity, and that although BDI, HADS (Hospital Anxiety and Depression Scale), SCL-90, and HRSD differ in terms of sensitivity and specificity, they are all valid as screening tests. BDI is commonly used for its time-efficiency and a small number of questions that reduce confusion in patients.9
Depression among patients with stroke was studied in relation to its correlation with other factors. The study of Robinson et al.19 concluded that patients with damaged frontal lobe had higher possibilities of suffering post-stroke depression. Moreover, the study of Morris et al.20 agreed to this conclusion, reporting that patients with damaged left hemisphere, the frontal lobe and basal ganglia in particular, suffered more severe depression. The study of Carson et al.,21 however, suggested that the location of lesion and post-stroke depression did not correlate. The effect of gender on the diseases is also controversial. While Paolucci et al.22 maintained that patients with cerebrovascular disease are at a much higher risk, Kaji et al.23 found no statistical correlation. This study also failed in discovering any correlation of depression with the damaged part in cerebrum or gender.
Personality traits are integral and organized behaviors that characterize an individual. This refers to the reactions of an individual to diverse circumstances, specifically those with stability and consistency, making it appropriate for deduction. There are 5 classifications that show both personality traits common in most humans and differences among individuals. We conducted this study based on the Big Five Structure/Five Factor Model, which shows that the personality traits of individuals is divided largely into 5 factors.24-28
There are studies presented abroad showing that N (neuroticism), one of the 5 factors, is closely related to post-stroke depression,29-31 but there have been no studies like this in Korea. This is most likely because there are not many tests that can be used for practical medical purposes rather than mere evaluation of personality. NEO-PI10 was selected carefully among tests that fulfilled the following conditions: differentiates of the 5 personality traits, quantitative analysis is possible, has a comparatively short measuring time, is easy for those at low cognitive level to understand, and is confirmed after translated into Korean. In Korea, the translation modified into by Kang11 (N: neuroticism, E: extraversion, O: openness to experience, A: agreeableness, C: conscientiousness) (Appendix 1) was used.
NEO-PI was used in a variety of areas, studying borderline personality disorder and paranoid personality disorder had a positive correlation with neuroticism (N), schizotypal personality disorder positively correlated with neuroticism (N) and negatively correlation with extraversion (E).32 In addition, it was reported that anxiety and schizophrenia have a positive correlation with neuroticism (N), mania has a positive correlation with extraversion (E), paranoia and antisocial personality have a negative correlation with agreeableness (A).33
This is because neuroticism (N) is defined as a personality trait that accumulates negative emotions (fear, anger, frustration).10,29 High neuroticism (N) is generally associated with being emotionally anxious, displaying hostility towards others, and being sensitive to what others think.33 This contributes to making a response to the changed appearance after stroke the most depressed compared to other types of traits.
The limitations of this study included a small number of subjects which made generalization difficult. Also, there were relatively more patients with damage in the left cerebral hemisphere, which is the result of excluding patient subjects of severe cognitive and communication dysfunction. Premorbid personality was not determined by NEO-PI based on the supposition that some change would take place in the patient, but there lies the possibility that a disparity may exist between the caregivers witness and the patients real personality before stroke. It is helpful, however, in the sense that screening tests can be done when patients are hospitalized and there is active rehabilitation when neuroticism is identified through the test.
CONCLUSION
Through this study, we found that in predicting depression of patients with stroke, knowing pre-morbid personality measured with NEO-PI is more helpful than knowing age, sex, causes of stroke, location of lesion, duration of illness, presence of underlying disease, education background, usage of depression drugs, or physical viability. Furthermore, not only BDI evaluated directly by the patient but also HRSD evaluated by intimate caregivers showed the correlation between premorbid personality and post-stroke depression scale. This conclusion signifies that premorbid personality helps predict depression, and that psychological and emotional support can be designed in a more specific manner along with medical treatment. Therefore, this should be considered seriously when setting rehabilitation goals of patients with stroke.
Appendices
Appendix 1
NEO-PI Questionnaire of Pre-morbid personality