Outcome Measurement in Balance Problems: Berg Balance Scale
Article information
Balance has been recognized as a crucial factor, as it involves maintaining posture during static stance and transitioning between movements, and it plays a significant role in performing daily activities. Consequently, numerous studies have been conducted to evaluate balance ability over the years [1].
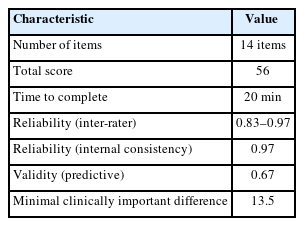
The Berg Balance Scale (BBS) is the best-known balance measure that assesses balance and fall risk in adults. The BBS consists of 14 items with an ordinal scale of 0 to 4 for a total of 56 points (a lower score indicates higher fall risk). Zero score indicates the lowest level of function and 4 score the highest level of function and it takes approximately 20 minutes to complete. The items evaluate from the static position with increasing difficulty by decreasing the base of support to dynamic activities. The BBS is designed with content closely resembling real-life daily activities, making it easy to learn and allowing for repetitive evaluations. It requires minimal cost, time, and simple equipment [2-4]. Additionally, even patients in the acute phase of stroke, many of whom may be unable to sit or stand, can undergo the assessment, highlighting its advantages [4].
The clinical utility of the BBS includes the ability to estimate rehabilitation outcomes using the total score of the scale. Research on estimating rehabilitation outcomes suggests that scores measured at admission using the BBS are inversely related to the length of hospitalization and can predict the duration of hospitalization and eventual discharge decisions [5]. Additionally, studies have categorized functional levels based on scores; for instance, scores ranging from 0 to 20 indicate the ability to walk with a walking aid, scores from 21 to 40 suggest the ability to walk with assistance, and scores from 41 to 56 indicate independent walking capability [6]. The BBS also serves as a predictor of fall risk, with scores of 41–56 indicating low risk, 21–40 indicating medium risk, and 0–20 indicating high risk [7].
Berg et al. [3,4] reported that the reliability of the BBS was 0.83 as measured by Cronbach’s alpha coefficient in a study involving the general elderly population, and 0.97 in a study involving stroke patients, indicating high reliability (Table 1). This suggests that the BBS may be particularly useful for assessing balance in stroke patients, showing higher reliability in this population compared to its original purpose of assessing fall risk in the elderly. The BBS has been validated for use in individuals with spinal cord injury and has the advantage of being valuable for other neurologic populations [8]. The Korean version of BBS has also been verified for validity and reliability [9].
The minimal clinically important difference (MCID) for balance improvement was 13.5 points in stroke patients, indicating that the BBS MCID does clinically detect changes in balance abilities in persons with stroke [10].
There are limitations in the BBS. The BBS doesn’t measures the quality of gait and the speed of walking, therefore, may be less useful than other tools where motor control is a bigger contributor to poor balance than muscle weakness. It also has a ceiling effect in younger people (<75) who have balance problems even if they have an increased risk of falling. [11].
In conclusion, the BBS is a useful outcome measure in predicting the risk of falls, assessing balance deficits, providing a numerical score that can be tracked for improvement over time, and even assessing the length of stay at inpatient rehabilitation.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING INFORMATION
None.