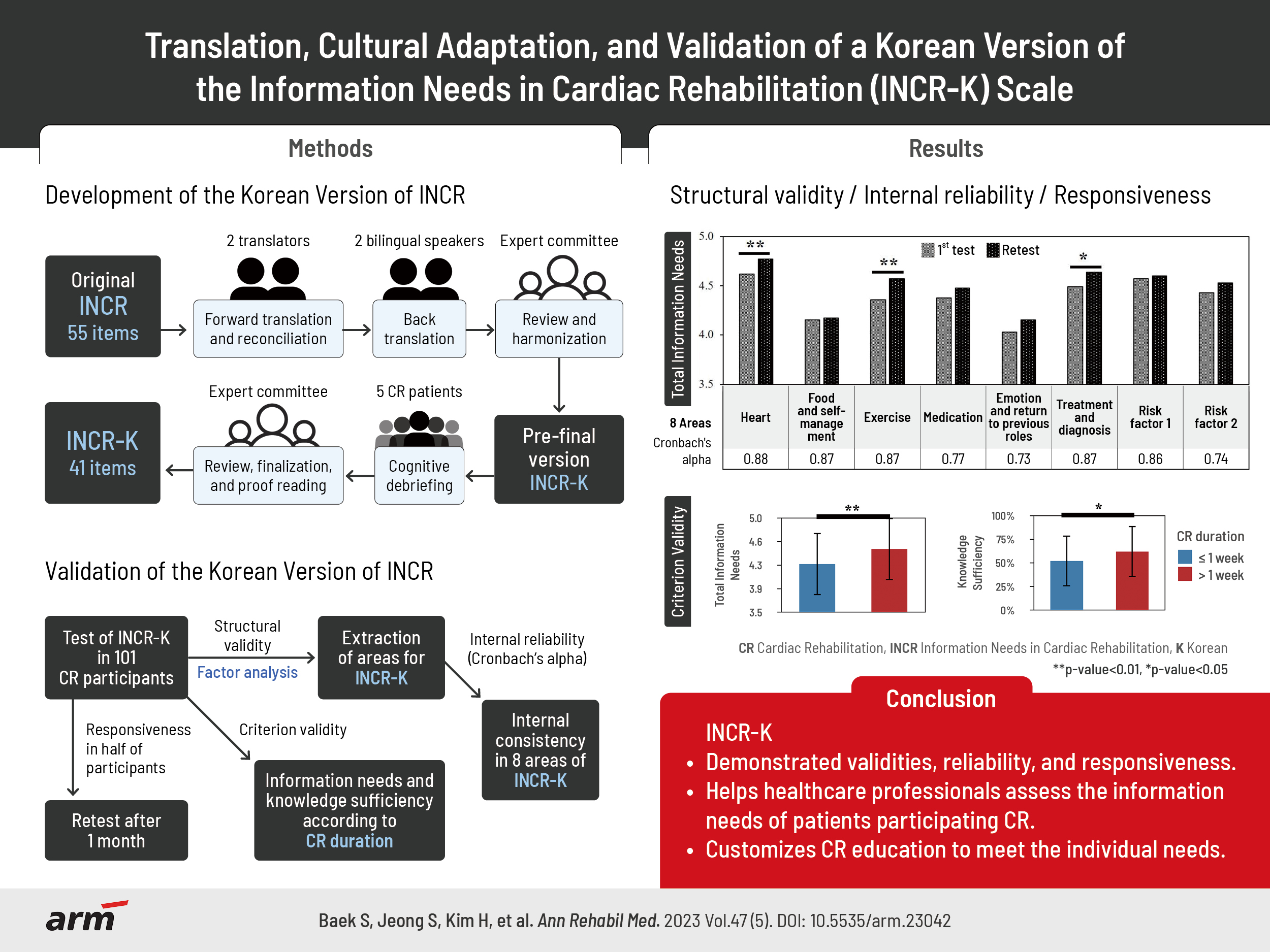
Translation, Cultural Adaptation, and Validation of a Korean Version of the Information Needs in Cardiac Rehabilitation Scale
Article information
Abstract
Objective
To translate and culturally adapt the Information Needs in Cardiac Rehabilitation (INCR) questionnaire into Korean and perform psychometric validation.
Methods
The original English version of the INCR, in which patients are asked to rate the importance of 55 topics, was translated into Korean (INCR-K) and culturally adapted. The INCR-K was tested on 101 cardiac rehabilitation (CR) participants at Kangwon National University Hospital and Seoul National University Bundang Hospital in Korea. Structural validity was assessed using principal component analysis, and Cronbach’s alpha of the areas was computed. Criterion validity was assessed by comparing information needs according to CR duration and knowledge sufficiency according to receipt of education. Half of the participants were randomly selected for 1 month of re-testing to assess their responsiveness.
Results
Following cognitive debriefing, the number of items was reduced to 41 and ratings were added to assess participants’ sufficient knowledge of each item. The INCR-K structure comprised eight areas, each with sufficient internal consistency (Cronbach’s alpha>0.7). Criterion validity was supported by significant differences in mean INCR-K scores based on CR duration and knowledge sufficiency ratings according to receipt of education (p<0.05). Information needs and knowledge sufficiency ratings increased after 1 month of CR, thus supporting responsiveness (p<0.05).
Conclusion
The INCR-K demonstrated adequate face, content, cross-cultural, structural, and criterion validities, internal consistency, and responsiveness. Information needs changed with CR, such that multiple assessments of information needs may be warranted as rehabilitation progresses to facilitate patient-centered education.
INTRODUCTION
Cardiovascular diseases (CVDs) represent a significant global health burden [1]. The implementation of secondary prevention strategies for CVDs has demonstrated remarkable effectiveness [2]. However, successful secondary prevention relies on patients’ knowledge and adoption of multiple health behavior changes [3]. Unfortunately, many patients do not achieve optimal risk reduction despite available interventions [4]. Therefore, it is crucial for healthcare providers to assess the information needs of cardiac patients to enhance treatment outcomes [5,6]. Nonetheless, accurately identifying patient information needs can be challenging for healthcare providers due to differences in perceived importance between clinical personnel and patients [7]. Moreover, patient information needs evolve over time, particularly as they transition back to their daily routines and incorporate various therapies [8]. Additionally, patient subpopulations may have diverse information needs based on factors such as sex, age, ethnicity, and socioeconomic status [7].
Extensive research has been dedicated to exploring patients’ information needs following various cardiovascular events, such as revascularization [9], acute coronary syndrome [10], post-myocardial infarction [8], and heart failure [11]. Surprisingly, limited attention has been given to investigating information needs in the context of cardiac rehabilitation (CR), despite patient education being a fundamental element of CR programs that aim to assist patients in implementing secondary prevention recommendations [12]. It is therefore recommended that an assessment of patient information needs be conducted prior to initiating patient education within CR, enabling the customization of educational interventions to meet individual needs and optimize outcomes [13].
In order to facilitate the identification of specific information needs in CR patients, a self-administered questionnaire called the Information Needs in Cardiac Rehabilitation (INCR; Appendix 1) was developed and subjected to psychometric validation in a Canadian context [14]. The INCR has since undergone translation and cultural adaptation for Chinese, Spanish, and Portuguese populations [15-17]. In the Korean setting, limited research has been conducted on the information needs of individuals with cardiac disorders. While several instruments have been developed in medically advanced countries since the 1990s to assess the information needs of cardiac patients [10], the availability of locally developed tools in this area remains scarce in Korea. To address this gap, a recent study aimed to translate the INCR questionnaire into Korean [18]. However, this study had certain limitations, particularly in terms of sample size, with only 45 participants, which was insufficient to establish the validity of the tool. Additionally, previous studies did not assess the construct and criterion validities of the translated INCR questionnaire.
The primary objective of the current study was to translate and culturally adapt the INCR tool for implementation in the Korean context and subsequently conduct a comprehensive psychometric validation involving a participant sample size of over 100 individuals. Furthermore, the study aimed to determine the participants’ highest priority information needs using the questionnaire.
METHODS
Design
This study was conducted in two stages. First, the INCR was translated and cross-culturally adapted into Korean version of the Information Needs in Cardiac Rehabilitation (INCR-K). Based on the COSMIN taxonomy [19], this first stage was to establish face, content, and cross-cultural validities of the scale. Face and content validities assess the extent to which a questionnaire accurately reflects its intended measurements. Several methods were employed to demonstrate face and content validities during translation, including cognitive debriefing, qualitative semi-structured interviews for feedback, and reviews conducted by an expert committee. The second step was the psychometric validation of the INCR-K through a cross-sectional survey, with repeated administration of the INCR-K in a random subsample. Structural validity, internal reliability, criterion validity, and responsiveness were assessed. This study was reviewed and approved by the Institutional Review Boards of Kangwon National University Hospital (IRB No. A-2022-01-005-002) and Seoul National University Bundang Hospital (IRB No. B-2207-769-303), and each participant provided informed written consent..
Materials
The INCR tool, developed and validated in English, assesses the information needs of patients undergoing CR. It consists of 55 items across 10 areas [14]. The 10 areas identified were the heart (physiology, symptoms, and surgical treatments), nutrition, exercise/physical activity, medication, work/vocational/social, stress/psychological factors, general/social concerns, emergency/safety, diagnosis and treatment, and risk factors. Each item in the INCR-K, which assesses information needs, is rated on a 5-point Likert scale of 1 (really not important) to 5 (very important). The tool can be used to tailor educational interventions for patients undergoing CR, with higher scores indicating higher information needs. Furthermore, the tool can be used regardless of the CR participation duration.
Translation and cross-cultural adaptation of the INCR
The translation and cross-cultural adaptation of the INCR followed the Patient-Reported Outcomes Translation and Linguistic Validation Task Force guidelines by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) [20], which include the following steps: (1) forward translation, (2) reconciliation, (3) back translation and review, (4) harmonization, (5) cognitive debriefing, (6) review of cognitive debriefing results and finalization, and (7) proofreading and final report.
Two independent translators (one was a medical doctor involved in the study and the other was not medical doctor) forward translated the INCR into Korean. Afterward, the two translations were reviewed for ambiguities, and any discrepancies were reconciled. Back translation was performed by two bilingual native English speakers fluent in Korean and blinded to the original English version. One translator was a healthcare provider, whereas the other was not.
An expert committee consisting of eight health professionals and translators compared the back translations to the original instrument for harmonization; in addition, the committee reviewed translations for linguistic, semantic, technical, and conceptual consistencies. This process resulted in the prefinal version of the INCR-K.
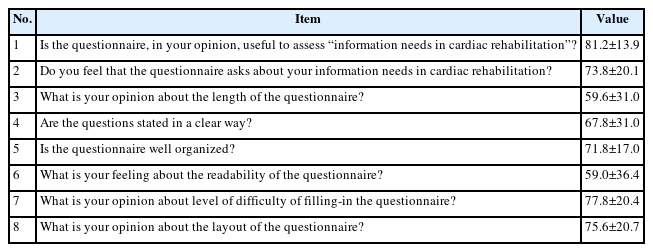
Regarding cognitive debriefing, the prefinal version was tested with five Korean patients from Kangwon National University Hospital receiving outpatient CR. The time required to complete the questionnaire was recorded, and patients were asked to provide feedback through qualitative semi-structured interviews. The patients were asked to rate the readability, length, and clarity of the questionnaire through 10 items, eight of which (Table 1) were rated through a visual analogue scale of 0–100 mm; 0 meaning not usable at all and 100 meaning very usable (i.e., higher scores denote more positive perceptions of the scale). These were analyzed using descriptive statistics. The remaining two questions (“If any of the questions in the survey are unclear, please tell us what they are” and “If any of the questions in the survey are duplicated, please tell us which one is the question”) were open-ended.
In the review of the input from cognitive debriefing by the expert committee, any ambiguous and redundant expressions were modified after a discussion. Finally, the refined version of the INCR-K was set for psychometric validation (Appendix 2).
Psychometric validation
Participants
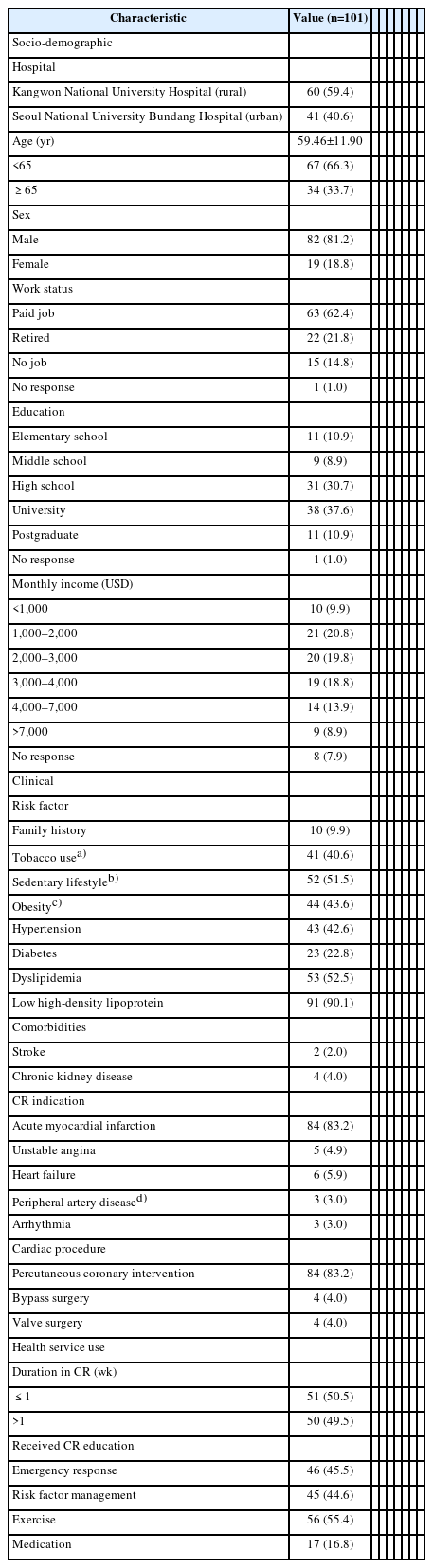
In total, 104 patients were recruited from the CR programs at Kangwon National University Hospital and Seoul National University Bundang Hospital in Korea (Fig. 1). Seoul National University Bundang Hospital is situated in an urban locale, while Kangwon National University Hospital is located in a rural area. Sample size calculation for psychometric analysis was based on the recommendation of Hair et al. [21], which stipulates a minimum of 100 participants. The inclusion criteria consisted of patients diagnosed with CVDs who underwent CR between February 2022 and December 2022. Exclusion criteria encompassed individuals under the age of 18 years, those with literacy problems, and those with severe visual, cognitive, or mental impairments that hindered their ability to complete the questionnaire. Upon enrollment, all participants underwent either a cardiopulmonary exercise test or an electrocardiogram-monitored exercise session. Additionally, all participants completed the CR education schedule, as documented in their medical records.
Measures
Participants completed the INCR-K questionnaire, and the scores of all items were averaged to determine the participants’ total information needs. In addition, the average score per area was calculated. Data from participants who did not complete more than 20% of the items were excluded from analysis. In addition to completing the INCR-K, participants provided self-reported sociodemographic characteristics, such as sex, age, income, educational attainment, and work status. Although the participants completed their education sessions during CR, they were asked about their experience with receiving CR education in specific topics, including emergency, risk factor, exercise, and medication, with response options of “yes” or “no.” The criterion for determining whether education had been received was based on the participants’ self-report, regardless of the actual content or extent of education. In addition, the participants were requested to indicate their preferred mode of education delivery (Appendix 3). Data on risk factors [22], diagnosed CVDs, comorbidities, treatment procedures, duration of CR, and number of CR sessions undertaken were obtained from the patients’ medical charts.
Statistical analysis (psychometric validations and descriptive analysis)
Structural validity was assessed using principal component analysis. The suitability of the data for this analysis was assessed using the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett’s sphericity test [23]. KMO values>0.60 were considered acceptable, and a p-value<0.05 in Bartlett’s sphericity test was considered significant. Areas with eigenvalues>1.0 were extracted according to the Kaiser-Guttman criterion [24]. The matrix was interpreted using the varimax method with Kaiser normalization. Factor loading values>0.30 indicated representation in each area [25]. The internal consistency of each area was calculated using Cronbach’s alpha, and a value>0.7 was considered to reflect satisfactory internal correlation between items of the same area [26].
Criterion validity was assessed using a t-test to compare the total INCR-K score (the mean of all items) among patients with different CR durations. The duration of CR was defined as the period starting from the initial of CR session, which could consist of either a cardiopulmonary exercise test or an electrocardiogram-monitored exercise session, up to the point of the completing of the questionnaire. The categorization of CR duration into two groups (≤1 week and >1 week) was motivated in the intention to observe potential changes in information needs between initial and subsequent participants after starting CR. The choice of using 1-week threshold was informed by that the average duration of phase 1 in CR is less than 1–2 weeks [27]. Furthermore, to assess the criterion validity of the newly introduced “knowledge sufficiency” scores, the INCR-K scores were compared to self-reported receipt of educational engagement.
To assess responsiveness, the questionnaire was re-administered 1 month after the first administration to half of the patients who were randomly selected using a computer-generated sequence. In our study, this 1-month interval was selected to correspond with the range of intervals (ranging from 3 weeks to 3 months) employed in previous studies [28,29]. Subsequently, the INCR-K scores for each area in the first and second administrations were compared using t-tests.
Descriptive statistics were used to describe the INCR-K scores and determine whether patients had sufficient knowledge of each item. Data analysis was performed using IBM SPSS Statistics 25.0 (IBM Corp.). Statistical significance was set at p<0.05.
RESULTS
Translation and cultural adaptation
Forward translation, reconciliation, back translation, and harmonization
During the forward translation of the INCR from English to Korean, appropriate consideration was given to the cultural implications of the Korean honorifics. After back translation, the discrepancies between the original and back-translated versions were identified and resolved. During harmonization, the expert committee decided to remove three items from the original questionnaire (original INCR items 37, 38, and 41) [14] because of the differences in medical systems between Canada and Korea. Afterward, the resulting prefinal version, consisting of 52 items, was subjected to cognitive debriefing.
Cognitive debriefing
The prefinal version of the INCR-K was tested on five patients. The researchers maintained a neutral stance throughout the self-administration process, encouraging the participants to complete all the questions. The questionnaire was completed in an average of 7 minutes and 44 seconds. The results of the subsequent semi-structured interviews showed high ratings of the INCR-K in terms of usefulness (mean score, 81.2±13.9). In contrast, the INCR-K was rated as relatively difficult to read (59.0±36.4), lengthy (59.6±31.0), and possessing some unclear sentences (67.8±31.0; Table 1). During the interviews, some participants commented that the medical terminology in the prefinal version was difficult to understand. Other participants expressed dissatisfaction with the number of items, redundant content, and vague expressions in the questionnaire.
Review of cognitive debriefing results and finalization
After reviewing the results of cognitive debriefing, the expert committee and the developer of the original INCR (Sherry L. Grace) revised the prefinal version; the revisions were as follows: (1) Incomprehensible expressions were modified to make them easier to understand; (2) Items with redundant or less relevant content were deleted, thus reducing the total number of items from 52 to 41; and (3) Vague expressions were clarified. Details of each change are provided below.
Respondents in the cognitive debriefing phase commented that several items were difficult to understand, particularly the item “What is angioplasty?”, which is an unfamiliar medical term to many patients. To address this problem, the word “stent” was added, making it #6 “What is angioplasty and stent placement?”. The term “stent” is a well-known term to patients.
To address the issue of length in the prefinal version and improve the overall readability of the questionnaire, we removed items that contained overlapping content. Three items regarding drug intake were identified to be similar; thus, the items “How do I remember to take my medication?” and “Are there foods I should avoid while taking these medications?” were deleted, leaving only item “How do I take my medication in the right way?” (INCR-K#21). Three items regarding stress were had overlapping content, and the items “How does stress affect my heart?” and “What can I do to reduce stress in my life?” were deleted, leaving only item “How can I cope with stress?” (INCR-K#27). Furthermore, two items on angina and chest pain were identified to have similar meanings, and the item “How do I recognize angina symptoms?” was deleted, leaving item “What should I do if I feel angina or chest pain?” (INCR-K#30) in the questionnaire. Three items regarding risk factors were similar in content; thus, the items “What are the risk factors that I cannot control?” and “What are the risk factors that I can control?” were deleted. The remaining item “What can I do to bring my risk factors under control?” (INCR-K#36) was retained. Finally, three similar items regarding tobacco use were evaluated and items “What are the benefits of quitting smoking?” and “What supports are available to help me quit smoking?” were deleted, leaving INCR-K#40, “How does tobacco affect the heart?” in the questionnaire.
Items with vague expressions were rephrased. For example, the item “When should I stop physical exercise?” was revised to “When should I stop exercise for safety?” (INCR-K#18) to better convey the intent of the question, which was to assess patients’ knowledge of the symptoms that should prompt the cessation of exercise during CR. To enhance clarity and comprehension, the item “What are the effects of complementary and alternative medications?” was revised to “Are complementary and alternative therapies (health supplements, Chinese medicine/acupuncture, massage, etc.) effective?” (INCR-K#23). This revision aimed to provide a clearer understanding of “complementary and alternative therapies.” To ensure the relevance of the questionnaire to the Korean context, specific examples such as “health supplements, Chinese medicine/acupuncture, massage, etc.” were thoughtfully selected from two studies that specifically investigated the role of complementary and alternative treatments in CR [30,31]. These examples were carefully incorporated into the study to ensure that the questionnaire accurately reflected the Korean context. Finally, item “What feelings are common after a heart attack?” was revised to “What feelings are common after a heart attack? (Can I seek help if I feel depressed or anxious?)” (INCR-K#25) to clarify the intent of the question, which was to check for depression and anxiety that may occur after a heart attack.
Furthermore, to streamline the questionnaire, questions that were not applicable to all participants were excluded. This decision was primarily made to avoid an unnecessarily lengthy questionnaire, which could result in reduced response rates, respondent fatigue, and compromised data quality. Questions regarding specific topics such as preventing low blood sugar during exercise, caring for the feet during an exercise program, returning to an old job, or driving after a heart condition were removed. Instead, the questions focused on information needs relevant to a broader patient population, allowing for the development of a concise and efficient questionnaire. This approach improved the response rates and enhanced the overall quality of the collected data.
In the harmonization phase, two items were initially deleted because of differences between the Canadian and Korean medical systems. However, after revising the items to be appropriate for the Korean medical system, these two items were reintegrated into the INCR-K as “Is there a support system that can help patients with heart disease?” (INCR-K#29) and “When (in what cases) do I need to make an outpatient appointment or go to the emergency room?” (INCR-K#31). Initially, these questions were phrased as “What services, support organizations and groups are available?” and “When should I call the doctor?”, respectively.
Finally, in addition, respondents were asked to rate not only the importance of each item, but also whether they perceived they already had sufficient knowledge of the topic area (yes/no). Thus, in CR programs, the focus of the medical staff education can be on the areas where the patients require more knowledge. The total knowledge sufficiency score was calculated based on the percentage of “yes” responses for all items.
Proofreading and final report
The final version of the 41-item INCR-K is provided in Appendix 2.
Psychometric validation
Characteristics of the participants
Initially, 104 patients provided informed consent to participate in the study; however, three patients were excluded from the analysis owing to failure to answer any of the items in the INCR-K, resulting in a total of 101 participants included in the study. As shown in Table 2, the item completion rates were high.
Table 3 shows the sociodemographic and clinical characteristics of the participants. Half the participants had recently started receiving CR. Approximately half of the participants had received heart education, but less than 25% had received education regarding medication at the time of survey administration.
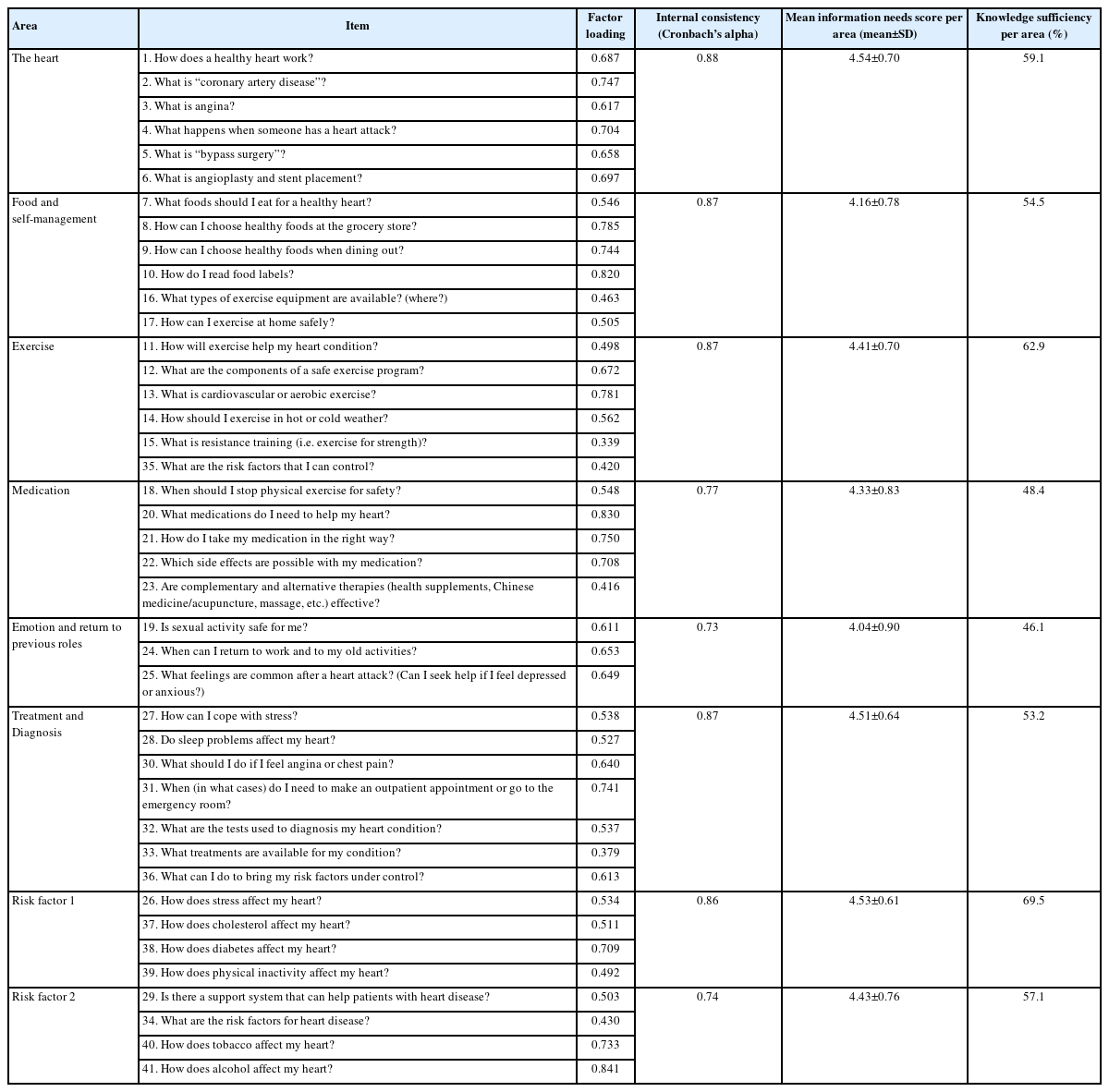
Factor analysis and internal consistency
Through translation and adaptation, the original 55 items of the INCR were reduced to 41 items in the final INCR-K. To assess structural validity, a factor analysis was conducted on the 41 items of the INCR-K using principal component analysis. The results showed that the data was suitable for factor analysis, with a KMO index of 0.824 (above 0.60) and a Bartlett’s test of sphericity of χ2=2,880.63 (p <0.001).
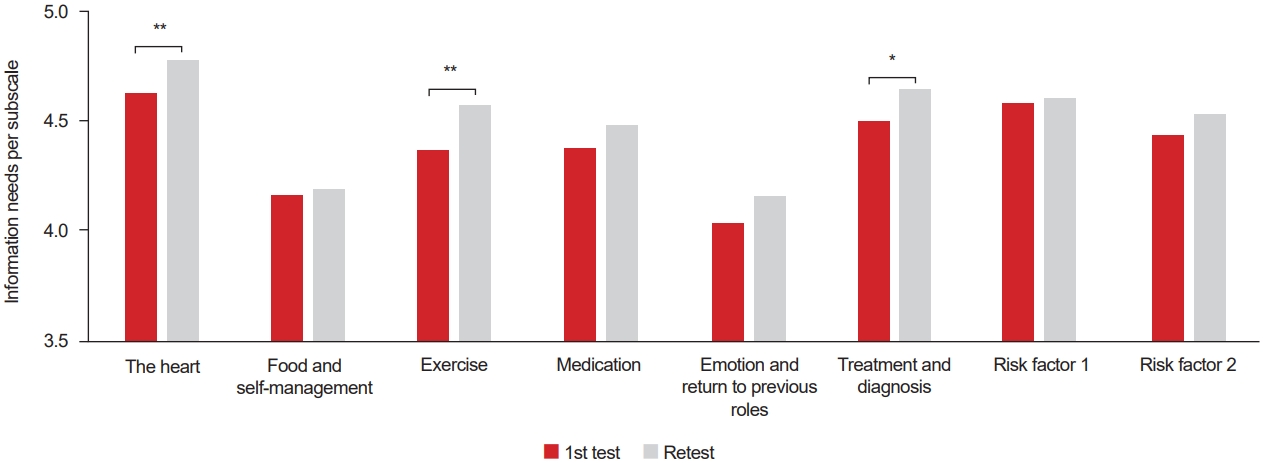
Eight areas were extracted, which accounted for 70.8% of the total variance. Table 4 presents the factor loading for the 41 items in the INCR-K. These areas included the heart, food and self-management, exercise, medication, emotion and return to previous roles, treatment and diagnosis, risk factors 1, and risk factor 2. The internal consistency of each area was assessed using Cronbach’s alpha of 0.73–0.88. All areas were considered internally consistent (α>0.70), as shown in Table 4.
Criterion validity
As shown in Fig. 2A, the mean INCR-K scores were compared based on CR duration. For CR durations categorized as ≤1 week (n=51, 50.5%) and >1 week (n=50, 49.5%), the mean INCR-K scores were 4.27±0.49 and 4.51±0.32, respectively. The results showed that patients with a longer CR duration perceived information as more important (p=0.005). Among 51 patients who had CR duration ≤1 week, 32 were inpatients, while the remaining 19 were outpatients. All 50 patients with CR duration >1 week were all outpatients.
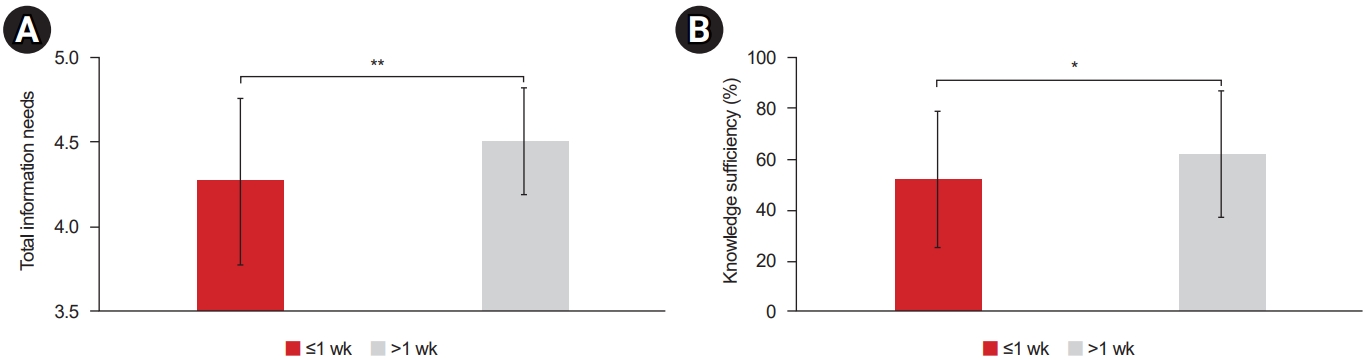
Total information needs (range, 1–5) (A) and knowledge sufficiency (range, 0%–100%) (B) based on cardiac rehabilitation duration, n=101. Significant differences are indicated by asterisks (*p<0.05, **p<0.01).
In addition, the criterion validity of the added knowledge sufficiency ratings was supported because the receipt of heart education was significantly related to these ratings of knowledge sufficiency (p<0.05), as shown in Fig. 3. Moreover, the criterion validity was supported because a longer CR duration corresponded to a higher knowledge sufficiency (p=0.04; Fig. 2B).
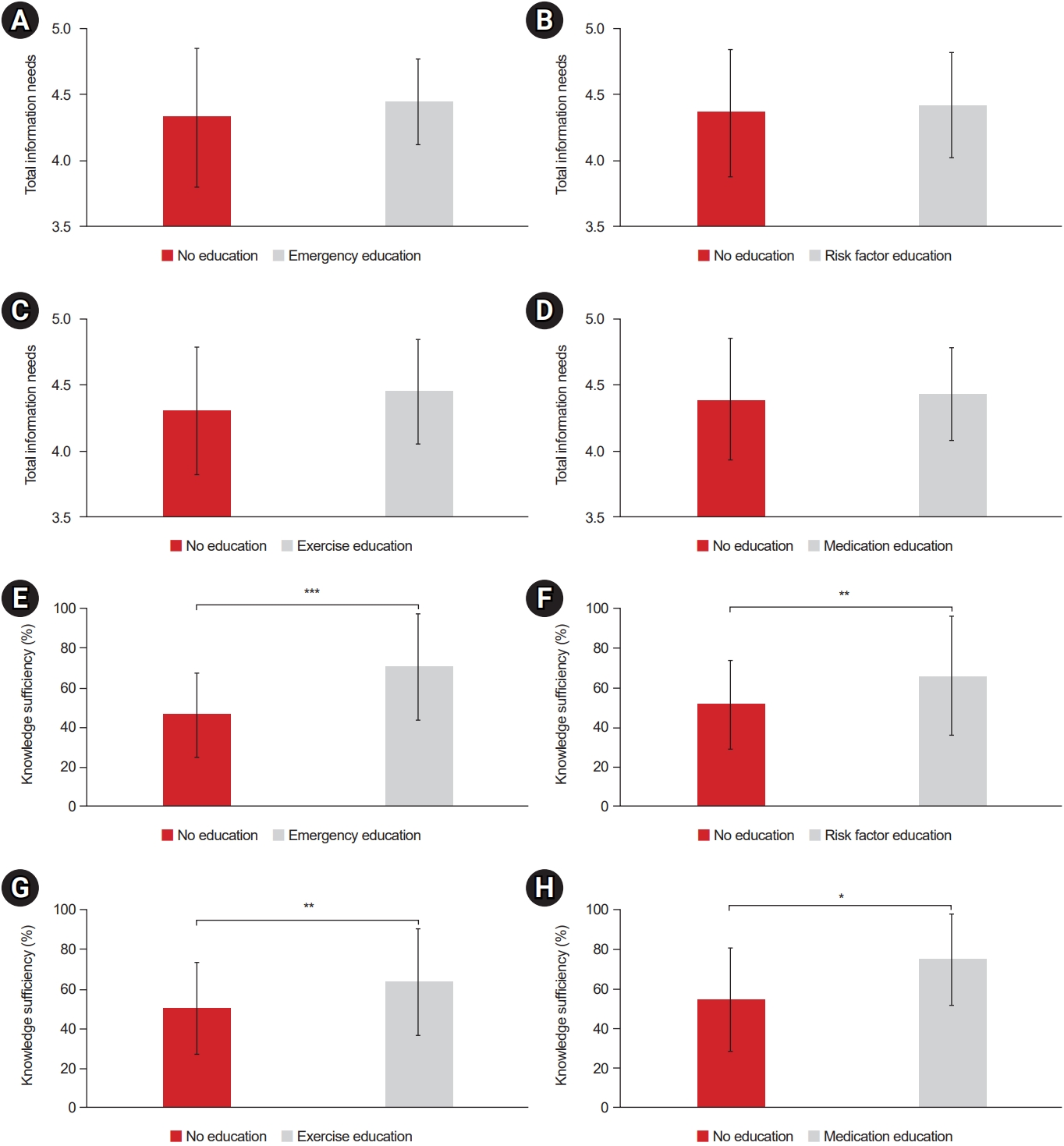
Total information needs (range, 1–5) (A-D) and knowledge sufficiency (range, 0%–100%) (E-H) by receipt of cardiac rehabilitation education, by topic. Perceived knowledge sufficiency was significantly related to previous receipt of heart education, but there were no differences in information needs, suggesting that patients understood the importance of the topics. Significant differences are indicated by asterisks (*p<0.05, **p<0.01, ***p<0.001).
Responsiveness
Of the randomly selected participants, 10 did not complete the INCR a second time and three completed the second questionnaire after more than 3 months (Fig. 1). Fig. 4 displays the INCR-K item scores per area at the first and second administrations. All areas were rated as more important during the second administration. There was a significant difference in information needs according to time in the following areas: the heart, exercise, and treatment and diagnosis. Specifically, during the first test, patients were most interested in learning about “the heart” and “treatment and diagnosis.” However, during the second test, participants reported their greatest information needs to be related to “the heart” and “exercise.”
Descriptive analysis of information needs and knowledge sufficiency and preferred educational delivery modes
The mean INCR-K score on the first administration was 4.38±0.43, with 85.1% of all participants rating the importance of the informational items as high (INCR-K score≥4). The three items with the highest ratings were as follows: #30 “What should I do if I feel angina or chest pain?” (4.79±0.46), #4 “What happens when someone has a heart attack?” (4.75±0.56), and #1 “How does a healthy heart work?” (4.66±0.55). Whereas, three items with the lowest information need were #23 “Are complementary and alternative therapies (health supplements, Chinese medicine/acupuncture, massage, etc.) effective?” (3.54±1.06), #19 “Is sexual activity safe for me?” (3.76±1.01), and #10 “How do I read food labels?” (3.80±0.87; Table 2).
Among the eight areas of the INCR-K, participants rated “the heart” and “risk factor 1” (e.g., stress, cholesterol, diabetes, and physical inactivity) as the most important information needs (4.54±0.70 and 4.53±0.61, respectively). Meanwhile, “emotion and return to previous roles” and “food and self-management” were rated as the lowest information needs (4.04±0.90 and 4.16±0.78, respectively; Table 4).
Table 2 presents knowledge sufficiency, expressed as the percentage of “yes” responses for each item. Knowledge sufficiency was 12.1%–82.8%. Specifically, the items with the highest knowledge sufficiency were #40 “How does tobacco affect my heart?”, #41 “How does alcohol affect my heart”, and #11 “How will exercise help my heart condition?”. Prior to psychometric validation, we hypothesized that items demonstrating higher knowledge sufficiency would indicate a reduced need for additional information. However, information needs remained high among participants with prior knowledge. The mean INCR-K score was 4.53±0.65 for participants with knowledge and 4.18±0.81 for those without knowledge (p<0.001).
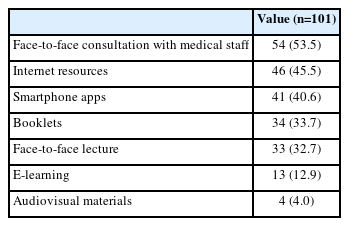
Table 5 shows that the preferred method of educational delivery was face-to-face consultation with medical staff (53.5%). Conversely, the least preferred method was through audiovisual materials (4.0%).
DISCUSSION
Fulfilling the information needs of cardiac patients positively affects the patients’ quality of life, satisfaction with care, and health outcomes [6]. To effectively address these needs, healthcare providers must evaluate the information needs of patients with cardiac diseases participating in CR programs. To assess the information needs in Korea, we translated the original INCR into Korean, culturally adapted it, and validated its psychometric properties. An abridged version comprising 41 items was finalized. This revised version also incorporated knowledge sufficiency rating, which may prove helpful in the current era where many patients receive health information online. The results supported the face, content, cross-cultural, and criterion validities of the INCR-K as well as its internal reliability and responsiveness.
The INCR enables healthcare providers to effectively identify and address the information needs of patients undergoing CR, thus bridging the information gap between medical staff and patients and ultimately resulting in improved outcomes [5,6]. In a previous study, the original version of the INCR was employed to identify the information needs of patients and gaps in the educational curriculum of patients undergoing CR [32]. Modifying the curriculum based on these findings can enhance the effectiveness and efficiency of education. Hence, further studies in Korea are warranted to assess the effectiveness of implementing the INCR-K in patient education.
The results of this study agrees with those of previous studies in some aspects but differ in others. First, similar to previous studies, this study established the criterion validity of INCR based on CR duration [14,15]. Decker et al. [8] observed that as the duration of CR increased, there was a corresponding increase in patients’ information needs. Initially, patients depend heavily on the clinicians’ decisions, particularly when confronted with life-threatening situations. However, as the CR program progresses and their condition stabilizes, patients gradually become more involved in the decision-making process. Consequently, the increase in information needs is attributable to the growing number of questions related to decision making. According to Ghisi et al. [33], extended CR participation enhances knowledge sufficiency. Continuous engagement in a CR program allows patients to reinforce their knowledge through repeated training sessions. Consequently, as the duration of CR increases, patients’ knowledge sufficiency improves. Second, the item (INCR-K#30) with the highest information needs was related to emergency and safety issues, which is consistent with the results of previous studies [6,34,35]. Emergency situations such as angina and heart attack were considered the most important, and this finding was consistent regardless of the stage of the patient in the CR program. Furthermore, it was observed that the “risk factor 1” area (e.g., stress, cholesterol, diabetes, and physical inactivity) demonstrated elevated information needs compared to other areas (Table 4). This finding aligns with those of previous studies reporting significant level of information need in this area [34,36]. The primary reason for heightened information needs in relation to risk factors may be attributable the intense fear of heart disease recurrence among individuals. This indicates that patients with a history of heart disease, particularly those who have had myocardial infarction, exhibit the highest level of concern regarding the possibility of recurrence and recognize the importance of managing risk factors for prevention [36]. Third, following translation and cultural adaptation, the number of items in the INCR questionnaire decreased from 55 to 41. Although these two areas were omitted, the overall structure of the INCR-K remained consistent with that of the original English version [14]. The initial version of the INCR encompasses 10 areas: heart, exercise/physical activity, medication, work/vocational/social, stress/psychological factors, general/social concerns, emergency/safety, diagnosis and treatment, risk factors, and barriers/goal setting. After translation and cultural adaptation, the INCR-K was created. It underwent a subsequent factor analysis, resulting in the identification of eight areas, namely heart, food and self-management, exercise, medication, emotion and return to previous roles, treatment and diagnosis, risk factor 1, and risk factor 2. Despite the variation in area composition between the original INCR and INCR-K, both questionnaires share common areas such as Heart, Exercise, Medication, Treatment and diagnosis, and Risk factor; thus ensuring the overall consistency of the questionnaire.
This study has several implications. First, it highlights the need for direct knowledge assessment to determine knowledge sufficiency more accurately. In the INCR-K, knowledge sufficiency was evaluated indirectly by asking patients to provide “yes” or “no” responses. However, solely confirming knowledge without direct assessment does not guarantee a precise understanding of the information. Although healthcare providers should prioritize addressing information that patients consider important and areas in which their knowledge is lacking, ascertaining patients’ actual comprehension without direct assessment remains challenging. Therefore, it is essential to ensure that patients understand the information using direct assessment methods. Furthermore, a distinction was observed between the actual implementation of education and the patients’ perceptions of receiving education. All 101 patients (100%) had received education as documented in their medical records; however, only 14 of 101 patients (13.9%) reported that they had received the complete education. This discrepancy suggests that patients may not feel confident about receiving sufficient education, thus highlighting the need for continued educational efforts. We believe that enhancing the curriculum by reinforcing education that patients did not acknowledge will result in a more effective delivery of education. Finally, the findings of this study emphasize the importance of regularly assessing patient information needs throughout their CR program, as these needs may change over time. This continued assessment can ensure that information needs are met and support optimal patient self-management.
To ensure efficient patient education in clinical settings, it is crucial to prioritize two key areas: the “area with the highest information needs” and “area with the lowest knowledge sufficiency.” The area with the highest information needs corresponds to the topics that patients are most curious about, whereas the area with the lowest knowledge sufficiency relates to subjects that patients have the least understanding. Among the various areas examined, the “heart” area demonstrated the highest information needs, with a score of 4.54±0.70 (Table 4). This result can be attributed to the significance of heart disease and patients’ priority of acquiring information and knowledge related to their heart health. Therefore, it is recommended to develop and implement educational programs that specifically focus on the “heart” area in clinical practice to enhance the knowledge of heart health. In contrast, the area of “emotion and return to previous roles” displayed the lowest knowledge sufficiency (Table 4). Patients’ lack of knowledge in this area is attributable to their perception of heart disease, primarily as a physical ailment, resulting in an insufficient understanding of the emotional challenges and importance of resuming their previous roles. Comorbid psychiatric disorders are prevalent in CR patients and significantly affect their quality of life [37]. Therefore, it is essential to incorporate regular psychiatric assessments into CR programs and provide robust support for patients to resume their previous roles [37].
This study had some limitations. First, although this study met the minimum sample size of 100 participants, as recommended by Hair et al. [21], the same authors suggested a minimum of five subjects per item for factor analysis, which would require 205 participants for the 41-item INCR-K. However, the assumptions were met for the factor analysis, and the solution converged, assuaging the sample size concerns. However, a larger sample size would be required to establish construct validity, although this has been established in other INCR versions; thus, any concerns in this regard would be minimal. In addition, this study was performed in only two regions of Korea. Future studies in other regions are warranted to establish generalizability.
In conclusion, the INCR-K questionnaire has satisfactory psychometric properties; hence, it can be used to assess the information needs of Korean patients undergoing CR. The results provide evidence of the face, content, cross-cultural, structural, and criterion validities, internal consistency, and responsiveness of the INCR-K. The INCR-K tool can support healthcare professionals in determining the information needs of patients undergoing CR. Therefore, education can be tailored to their individual needs.
Notes
No potential conflict of interest relevant to this article was reported.
None.
Conceptualization: Baek S, Kim WS, Grace SL. Formal analysis: Jeong S, Baek S. Investigation: Jeong S, Kim H, Cha S, Choi E. Methodology: Jeong S, Kim WS, Chang WK, Kim C, Grace SL, Baek S. Project administration: Baek S. Visualization: Jeong S, Baek S. Writing – original draft: Jeong S, Baek S. Writing – review and editing: Jeong S, Kim WS, Chang WK, Grace SL, Baek S. Approval of final manuscript: all authors.