- Search
| Ann Rehabil Med > Volume 46(1); 2022 > Article |
|
Abstract
Objective
Methods
Results
AUTHOR CONTRIBUTION
Conceptualization: Kim EK, Lee JH, Kim KW, Lim JY, Lee SU, Chung SG, Oh BM. Methodology: Kim JY, Kim EK, Shim HS, Lee JH, Lee GJ, Kim KW, Lim JY, Beom JW, Lee SY, Lee SU, Chung SG, Oh BM. Formal analysis: Kim JY, Kim EK, Oh BM. Funding acquisition: Kim KW, Chung SG, Oh BM. Project administration: Kim EK, Lee JH, Lee GJ, Beom JW, Lee SY, Oh BM. Visualization: Kim JY, Kim EK. Writing - original draft: Kim JY, Kim EK, Shim HS. Writing - review and editing: all authors. Approval of final manuscript: all authors.
ACKNOWLEDGMENTS
SUPPLEMENTARY MATERIALS
Fig. S1.
Fig. S2.
Table S5.
Fig. 1.

Fig. 2.
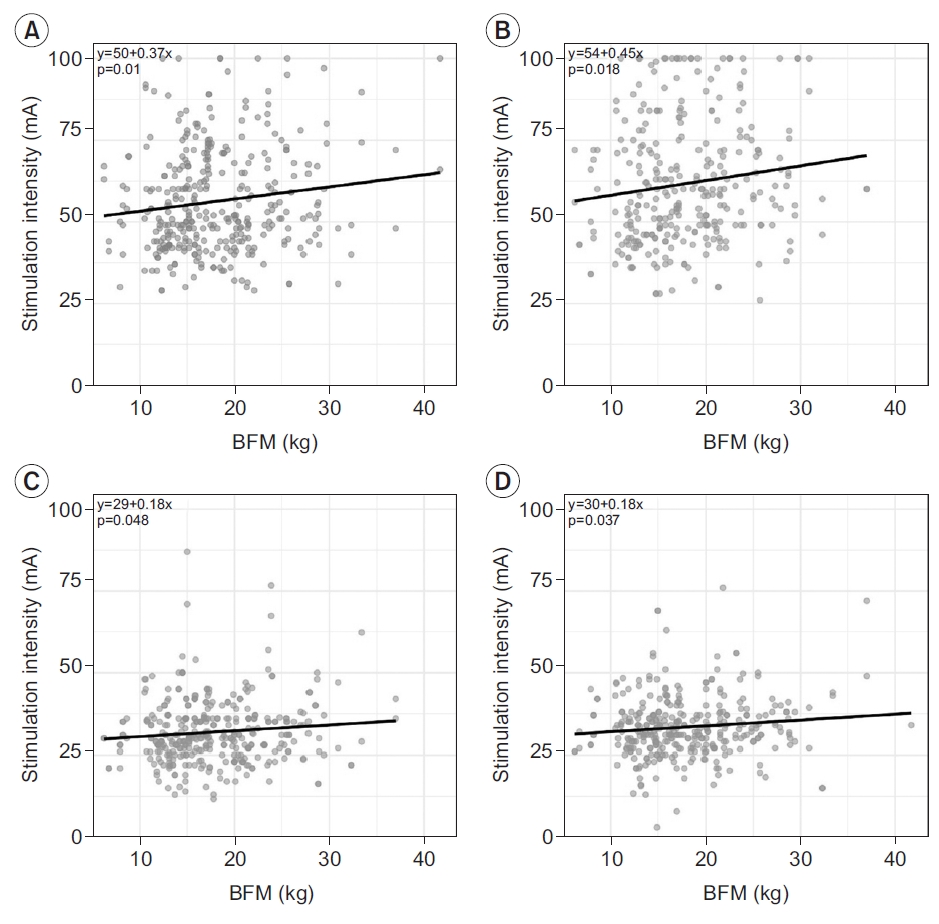
Table 1.
|
Male |
Female |
p-value |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 20s (n=100) | 50s (n=100) | 20s (n=100) | 50s (n=98) |
20s vs. 50s |
Male vs. female |
|||||
| Male | Female | 20s | 50s | |||||||
| Distal | Lonset (ms) | 4.1±1.3 (2.8–5.4) | 4.0±1.0 (3.0–5.0) | 4.0±1.2 (2.8–5.2) | 3.8±1.1 (2.7–4.8) | 0.202 | 0.009** | 0.175 | 0.001** | |
| 3rd–97th percentile | 3.1–5.4 | 3.4–5.1 | 3.1–5.4 | 3.0–4.7 | ||||||
| Ampbase-peak (mV) | 17.7±8.2 (9.5–26.0) | 16.2±7.1 (9.1–23.3) | 19.0±8.7 (10.3–27.7) | 17.0±8.7 (8.3–25.6) | 0.013* | 0.001** | 0.034* | 0.243 | ||
| 3rd–97th percentile | 10.2–24.4 | 8.4–23.3 | 12.1–27.6 | 10.2–24.4 | ||||||
| Amppeak-peak (mV) | 30.2±12.9 (17.3–43.0) | 27.2±14.8 (12.3–42.0) | 33.2±15.7 (17.6–48.9) | 28.7±13.0 (15.6–41.7) | 0.003** | <0.001** | 0.004** | 0.145 | ||
| Aneg (mVms) | 47.2±19.1 (28.1–66.3) | 39.7±22.3 (17.3–62.0) | 53.8±25.2 (28.7–79.0) | 40.6±19.2 (21.4–59.7) | <0.001** | <0.001** | <0.001** | 0.543 | ||
| Dneg (ms) | 6.1±1.8 (4.3–7.8) | 5.7±1.4 (4.3–7.1) | 6.2±1.6 (4.6–7.8) | 5.7±1.5 (4.2–7.1) | <0.001** | <0.001** | 0.229 | 0.842 | ||
| Proximal | Ampbase-peak (mV) | 14.2±6.5 (7.7–20.7) | 12.8±7.1 (5.7–19.9) | 15.2±7.7 (7.5–22.9) | 13.3±6.8 (6.5–20.1) | 0.004** | <0.001** | 0.045* | 0.299 | |
| Amppeak-peak (mV) | 24.1±10.7 (13.4–34.8) | 21.0±11.4 (9.6–32.4) | 26.9±13.3 (13.6–40.2) | 22.4±10.0 (12.3–32.4) | <0.001** | <0.001** | 0.002** | 0.082 | ||
| Aneg (mVms) | 41.7±18.6 (23.1–60.4) | 34.4±20.0 (14.5–54.4) | 48.2±23.2 (25.0–71.4) | 35.8±16.4 (19.4–52.2) | <0.001** | <0.001** | <0.001** | 0.296 | ||
| Dneg (ms) | 6.6±1.6 (5.0–8.3) | 6.2±1.5 (4.7–7.7) | 6.8±1.7 (5.1–8.5) | 6.2±1.5 (4.7–7.7) | <0.001** | <0.001** | 0.279 | 0.743 | ||
| Proximal-to-distal | NCV (m/s) | 50.3±15.2 (35.1–65.5) | 48.8±9.1 (39.6–57.9) | 49.6±14.7 (34.8–64.3) | 48.4±14.1 (34.2–62.5) | 0.056 | 0.078 | 0.390 | 0.534 | |
| 3rd–97th percentile | 37.6–63.7 | 41.7–57.8 | 39.7–59.7 | 40.8–55.9 | ||||||
| Ratioarea | 0.89±0.22 (0.67–1.10) | 0.87±0.15 (0.72–1.02) | 0.90±0.19 (0.71–1.09) | 0.89±0.14 (0.75–1.02) | 0.225 | 0.344 | 0.395 | 0.093 | ||
| Ratioamp | 0.81±0.24 (0.57–1.05) | 0.79±0.16 (0.63–0.95) | 0.80±0.15 (0.65–0.95) | 0.79±0.14 (0.65–0.93) | 0.158 | 0.312 | 0.563 | 0.968 | ||
Values are presented as mean±expanded uncertainty (range). However, Aneg, Dneg, and Ratioarea are presented as mean±2 standard deviation (range).
Lonset, onset latency; Ampbase-peak, baseline to negative peak amplitude; Amppeak-peak, negative peak to positive peak amplitude; Aneg, negative spike area; Dneg, negative spike duration; NCV, nerve conduction velocity; Ratioarea, proximal-to-distal area ratio; Ratioamp, proximal-to-distal amplitude ratio.
Table 2.
|
Male |
Female |
p-value |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 20s (n=100) | 50s (n=100) | 20s (n=100) | 50s (n=98) |
20s vs. 50s |
Male vs. female |
|||||
| Male | Female | 20s | 50s | |||||||
| Distal | Lonset (ms) | 4.3±1.2 (3.1–5.4) | 4.2±1.4 (2.8–5.6) | 4.1±1.7 (2.5–5.8) | 4.0±1.4 (2.7–5.4) | 0.694 | 0.218 | 0.261 | 0.029* | |
| 3rd–97th percentile | 3.2–5.3 | 3.1–5.5 | 2.9–5.9 | 2.8–5.1 | ||||||
| Ampbase-peak (mV) | 7.1±3.8 (3.4–10.9) | 5.9±3.8 (2.1–9.8) | 6.0±3.1 (2.9–9.0) | 4.8±2.7 (2.1–7.5) | <0.001** | <0.001** | <0.001** | <0.001** | ||
| 3rd–97th percentile | 4.1–11.1 | 3.0–9.3 | 3.3–8.8 | 2.8–7.1 | ||||||
| Amppeak-peak (mV) | 11.6±6.4 (5.1–18.0) | 9.3±6.5 (2.9–15.8) | 9.9±5.3 (4.5–15.1) | 7.4±4.5 (2.9–11.9) | <0.001** | <0.001** | <0.001** | <0.001** | ||
| Aneg (mVms) | 21.2±13.1 (8.1–34.3) | 16.2±11.4 (4.8–27.6) | 18.1±9.4 (8.7–27.5) | 13.4±8.1 (5.2–21.5) | <0.001** | <0.001** | <0.001** | <0.001** | ||
| Dneg (ms) | 5.9±1.7 (4.3–7.6) | 5.5±1.4 (4.1–7.0) | 6.1±1.9 (4.1–8.0) | 5.6±1.4 (4.2–7.0) | <0.001** | <0.001** | 0.253 | 0.762 | ||
| Proximal | Ampbase-peak (mV) | 6.7±3.6 (3.1–10.3) | 5.4±3.6 (1.8–9.0) | 5.6±3.0 (2.6–8.6) | 4.4±2.6 (1.8–7.0) | <0.001** | <0.001** | <0.001** | <0.001** | |
| Amppeak-peak (mV) | 10.7±5.8 (4.9–16.5) | 8.4±6.0 (2.3–14.4) | 9.1±5.2 (4.0–14.3) | 6.8±4.3 (2.5–11.1) | <0.001** | <0.001** | <0.001** | <0.001** | ||
| Aneg (mVms) | 20.9±12.8 (8.1–33.7) | 15.7±11.0 (4.7–26.7) | 17.8±4.5 (8.3–27.2) | 12.9±7.8 (5.1–20.7) | <0.001** | <0.001** | <0.001** | <0.001** | ||
| Dneg (ms) | 6.3±1.7 (4.6–8.1) | 6.1±1.5 (4.7–7.6) | 6.4±2.0 (4.4–8.4) | 6.0±1.5 (4.5–7.4) | 0.033* | <0.001** | 0.395 | 0.430 | ||
| Proximal-to-distal | NCV (m/s) | 50.7±8.5 (42.2–59.3) | 49.0±8.2 (40.8–57.3) | 51.3±14.0 (37.2–65.3) | 50.7±13.7 (37.0–64.4) | 0.002** | 0.354 | 0.345 | 0.003** | |
| 3rd–97th percentile | 44.8–58.2 | 42.4–57.3 | 44.5–57.7 | 43.3–58.9 | ||||||
| Ratioarea | 0.98±0.14 (0.84–1.12) | 0.97±0.19 (0.78–1.16) | 0.97±0.13 (0.83–1.10) | 0.95±0.18 (0.77–1.13) | 0.485 | 0.171 | 0.436 | 0.260 | ||
| Ratioamp | 0.93±0.19 (0.74–1.12) | 0.90±0.24 (0.66–1.14) | 0.93±0.17 (0.77–1.10) | 0.91±0.21 (0.70–1.11) | 0.019* | 0.012* | 0.939 | 0.733 | ||
Values are presented as mean±expanded uncertainty (range). However, Aneg, Dneg, and Ratioarea are presented as mean±2 standard deviation (range).
Lonset, onset latency; Ampbase-peak, baseline to negative peak amplitude; Amppeak-peak, negative peak to positive peak amplitude; Aneg, negative spike area; Dneg, negative spike duration; NCV, nerve conduction velocity; Ratioarea, proximal-to-distal area ratio; Ratioamp, proximal-to-distal amplitude ratio.
Table 3.
|
Male |
Female |
p-value |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 20s (n=100) | 50s (n=100) | 20s (n=100) | 50s (n=98) |
20s vs. 50s |
Male vs. female |
||||
| Male | Female | 20s | 50s | ||||||
| Lonset (ms) | 2.9±0.7 (2.2–3.6) | 2.9±0.7 (2.2–3.5) | 2.8±0.7 (2.2–3.5) | 2.8±0.7 (2.0–3.5) | 0.193 | 0.020* | 0.039* | 0.003** | |
| 3rd–97th percentile | 2.4–3.3 | 2.4–3.3 | 2.4–3.3 | 2.2–3.3 | |||||
| Ampbase-peak (μV) | 26.8±15.5 (11.3–42.3) | 21.7±11.9 (9.8–33.6) | 29.4±14.5 (14.9–43.8) | 23.9±13.5 (10.4–37.4) | <0.001** | <0.001** | 0.010* | 0.010* | |
| 3rd–97th percentile | 14.0–39.1 | 14.1–31.3 | 13.7–39.7 | 13.8–35.4 | |||||
| Amppeak-peak (μV) | 28.3±19.7 (8.6–48.0) | 23.3±14.2 (9.1–37.5) | 31.3±18.0 (13.3–49.3) | 26.1±15.9 (10.2–41.9) | <0.001** | <0.001** | 0.022* | 0.008** | |
| 3rd–97th percentile | 13.0–47.6 | 12.2–36.2 | 13.2–48.1 | 14.4–41.8 | |||||
| Aneg (μVms) | 19.2±14.6 (4.6–33.8) | 14.3±8.8 (5.5–23.1) | 20.5±13.6 (6.9–34.1) | 16.3±11.6 (4.7–27.9) | <0.001*** | <0.001** | 0.189 | 0.007** | |
| Dneg (ms) | 1.9±0.6 (1.3–2.5) | 1.9±0.6 (1.3–2.5) | 1.8±0.4 (1.4–2.2) | 1.8±0.4 (1.4–2.2) | 0.795 | 0.077 | 0.001** | 0.082 | |
Values are presented as mean±expanded uncertainty (range). However, Aneg and Dneg, are presented as mean±2 standard deviation (range).
Lonset, onset latency; Ampbase-peak, baseline to negative peak amplitude; Amppeak-peak, negative peak to positive peak amplitude; Aneg, negative spike area; Dneg, negative spike duration.
Table 4.
|
Male |
Female |
p-value |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 20s (n=100) | 50s (n=100) | 20s (n=100) | 50s (n=98) |
20s vs. 50s |
Male vs. female |
||||
| Male | Female | 20s | 50s | ||||||
| Lonset (ms) | 2.9±0.6 (2.2–3.5) | 2.9±0.7 (2.2–3.6) | 2.7±0.6 (2.1–3.4) | 2.7±0.7 (2.0–3.4) | 0.053 | 0.536 | 0.002** | <0.001** | |
| 3rd–97th percentile | 2.4–3.3 | 2.4–3.4 | 2.4–3.1 | 2.2–3.3 | |||||
| Ampbase-peak (μV) | 21.7±13.5 (8.3–35.2) | 17.1±12.4 (4.7–29.5) | 23.7±14.1 (9.6–37.9) | 18.2±10.5 (7.7–28.8) | <0.001** | <0.001** | 0.030* | 0.129 | |
| 3rd–97th percentile | 12.7–34.3 | 9.3–28.6 | 12.8–37.9 | 10.7–27.7 | |||||
| Amppeak-peak (μV) | 23.6±19.1 (4.5–42.7) | 18.6±14.6 (4.0–33.2) | 26.9±19.0 (7.9–45.9) | 20.1±13.9 (6.2–34.1) | <0.001** | <0.001** | 0.014* | 0.131 | |
| 3rd–97th percentile | 11.7–44.3 | 8.8–31.6 | 12.0–44.4 | 10.0–34.8 | |||||
| Aneg (μVms) | 15.4±11.2 (4.2–26.6) | 11.2±10.2 (1.0–21.4) | 17.5±12.4 (5.1–29.9) | 12.1±8.2 (3.9–20.3) | <0.001** | <0.001** | 0.011* | 0.186 | |
| Dneg (ms) | 2.0±0.8 (1.2–2.8) | 2.1±0.6 (1.5–2.7) | 1.9±0.6 (1.3–2.5) | 2.0±0.8 (1.2–2.8) | 0.462 | 0.571 | 0.206 | 0.206 | |
Values are presented as mean±expanded uncertainty (range). However, Aneg and Dneg, are presented as mean±2 standard deviation (range).
Lonset, onset latency; Ampbase-peak, baseline to negative peak amplitude; Amppeak-peak, negative peak to positive peak amplitude; Aneg, negative spike area; Dneg, negative spike duration.
Table 5.
|
Side-to-side difference |
||
|---|---|---|
| Mean±SD | Mean+2SD | |
| Tibial nerve | ||
| Lonset (ms) | 0.47±0.45 | 1.37 |
| Ampbase-peak (%) | 18.46±13.80 | 46.06a) |
| NCV (%) | 8.42±7.51 | 23.44b) |
| Common peroneal nerve | ||
| Lonset (ms) | 0.42±0.42 | 1.26 |
| Ampbase-peak (%) | 19.50±15.09 | 49.68 |
| NCV (%) | 5.85±5.04 | 15.93 |
| Sural nerve | ||
| Lonset (ms) | 0.13±0.11 | 0.35 |
| Ampbase-peak (%) | 10.23±8.61 | 27.45 |
| Amppeak-peak (%) | 14.14±10.67 | 35.48 |
| Superficial peroneal nerve | ||
| Lonset (ms) | 0.17±0.15 | 0.47 |
| Ampbase-peak (%) | 11.99±9.93 | 31.85 |
| Amppeak-peak (%) | 14.24±10.38 | 35.00 |
REFERENCES
- TOOLS







